Persistent Fetal Vasculature (PFV), formerly known as persistent hyperplastic primary vitreous (PHPV), is a congenital eye condition caused by the inability of the fetal hyaloid vascular system to regress. This vascular system normally feeds the developing lens and vitreous during fetal development and is expected to regress by the time of birth. When this regression fails, remnants of the vascular system remain, resulting in a variety of ocular abnormalities that can impair vision.
PFV is usually diagnosed in infancy and can appear unilaterally (in one eye) or bilaterally (in both eyes). Clinical signs include leukocoria (a white pupillary reflex), microphthalmia (an abnormally small eye), cataracts, elongated ciliary processes, and retinal detachment. If left untreated, these structural anomalies can have a significant impact on visual acuity, potentially leading to amblyopia or blindness.
A comprehensive ophthalmic examination is usually used to diagnose PFV, which is then supported by imaging techniques such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI). These imaging modalities aid in the identification of abnormal vascular remnants and associated ocular structures. Early diagnosis and intervention are critical for effectively managing PFV and improving visual outcomes.
Conventional Persistent Fetal Vasculature Treatment
The management and treatment of PFV are complex and tailored to each patient’s unique anatomical and functional abnormalities. Traditional treatments aim to preserve vision and prevent complications by combining medical and surgical interventions.
Observation and Monitoring: In mild cases of PFV that have no significant impact on vision or ocular structure, careful observation and regular monitoring may be advised. This method entails performing periodic eye exams to assess the stability of the condition and detect any changes that may necessitate intervention.
Medical Therapy: While there are no specific medications to treat PFV, supportive treatments such as atropine drops or patching therapy can help manage amblyopia (lazy eye) and promote visual development in the affected eye. Additionally, medications may be prescribed to treat secondary complications such as glaucoma.
Surgical Intervention: Surgery is frequently required in cases where PFV severely impairs vision or poses a risk of further complications. The type of surgical intervention depends on the specific ocular abnormalities and can include:
- Lensectomy: Removing the cataractous lens is a common procedure for PFV patients with cataracts. This surgery attempts to clear the visual axis and improve light entry into the eye.
- Vitrectomy: Vitrectomy is the surgical removal of the vitreous gel, which may contain fetal vasculature remnants. This procedure reduces traction on the retina and prevents retinal detachment.
- Retinal Detachment Repair: In cases where PFV causes retinal detachment, surgical repair is required to reattach the retina and restore function. Scleral buckling and pars plana vitrectomy are two possible techniques.
- Glaucoma Surgery: If PFV is associated with secondary glaucoma, surgical interventions like trabeculectomy or glaucoma drainage device implantation may be required to control intraocular pressure and protect the optic nerve.
Postoperative Care and Rehabilitation: After surgery, comprehensive postoperative care is required to ensure proper healing and optimal visual outcomes. This includes routine follow-up visits, visual rehabilitation, and, in some cases, the use of corrective or contact lenses to correct refractive errors.
Innovative Treatment Options for Persistent Fetal Vasculature (PFV)
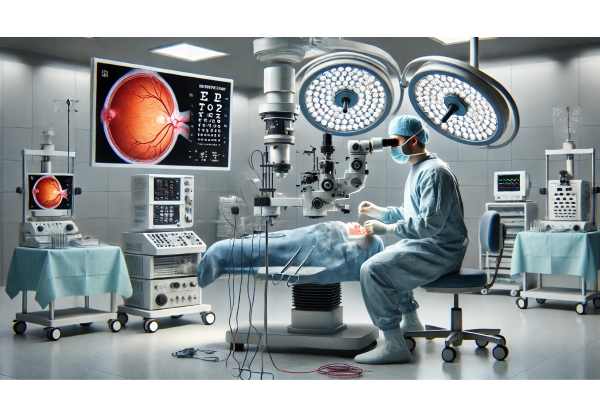
Recent advances in medical research and technology have resulted in significant improvements in the treatment and management of PFV. These cutting-edge approaches seek to improve surgical precision, visual outcomes, and reduce the risk of complications. Here, we look at some of the most effective and innovative treatments for PFV management.
Advanced Imaging Techniques
Advanced imaging technologies have transformed the diagnosis and surgical planning for PFV. High-resolution imaging modalities provide detailed visualization of ocular structures, allowing for precise assessment and targeted intervention.
Optical Coherence Tomography (OCT): OCT is a non-invasive imaging method for creating high-resolution cross-sectional images of the retina and other ocular tissues. It allows for detailed visualization of the vitreous, retina, and optic nerve, which aids in early diagnosis and accurate assessment of PFV. Enhanced depth imaging OCT (EDI-OCT) can improve visualization of deep ocular structures, assisting in surgical planning and postoperative monitoring.
Ultrasound Biomicroscopy(UBM): UBM creates detailed images of the eye’s anterior segment using high-frequency sound waves. It is especially useful for assessing the ciliary body, iris, and lens, which provides critical information for surgical decision-making in PFV cases. UBM can help detect persistent fetal vasculature and assess its impact on nearby ocular structures.
Intraoperative Optical Coherence Tomography (iOCT): iOCT incorporates OCT imaging into the surgical microscope, providing real-time visualization of ocular structures during surgery. This technology improves surgical precision by providing continuous feedback on anatomical details, allowing surgeons to make more informed decisions and adjust their techniques as needed. iOCT is especially useful in complex PFV surgeries, where precise dissection and manipulation of delicate tissues are required.
Minimal Invasive Surgical Techniques
Advances in surgical techniques have resulted in the development of minimally invasive approaches to PFV management. These techniques aim to reduce surgical trauma, speed up recovery, and improve visual outcomes.
Microincision Vitrectomy Surgery (MIVS). MIVS involves the use of smaller gauge instruments (23-gauge, 25-gauge, or 27-gauge) during vitrectomy procedures. Smaller incisions reduce surgical trauma, promote faster healing, and lower the risk of complications. MIVS enables precise removal of vitreous opacities and persistent fetal vasculature, thereby improving the visual axis and reducing retinal traction.
Femtosecond Laser-Assisted Surgery: Femtosecond laser technology offers precise and controlled tissue dissection, allowing surgeons to perform delicate maneuvers with high accuracy. Femtosecond lasers can be used in PFV management for anterior segment surgeries like lensectomy and capsulotomy, improving surgical precision and lowering the risk of complications. The use of femtosecond lasers in PFV surgery is a new field with exciting potential for improving outcomes.
Endoscopic Vitrectomy: Endoscopic vitrectomy is a technique that uses an endoscope in conjunction with vitrectomy instruments to improve visualization and access to the posterior segment. This technique is especially useful when the anterior segment is opaque, limiting the view through traditional surgical microscopes. Endoscopic vitrectomy allows surgeons to perform precise dissection and removal of persistent fetal vasculature, which improves surgical outcomes in difficult PFV situations.
Gene Therapy and Molecular Treatments
Gene therapy and molecular treatments are a promising frontier in the treatment of congenital eye diseases, including PFV. These novel approaches seek to address the underlying genetic and molecular mechanisms that drive the disease, with the potential for long-term and even curative results.
Gene Editing Technologies: Advances in gene editing technologies, such as CRISPR-Cas9, have created new opportunities for correcting genetic defects linked to PFV. Gene editing, which precisely targets and modifies specific genes, has the potential to prevent abnormal fetal vasculature persistence and promote normal ocular development. While still in the experimental stage, gene editing shows great promise for future PFV treatments.
Antiangiogenic Therapies: Anti-angiogenic therapies aim to reduce the abnormal blood vessel growth associated with PFV. These treatments involve the use of molecules that inhibit angiogenesis, the process by which new blood vessels form. Intraocular administration of anti-angiogenic agents, such as vascular endothelial growth factor (VEGF) inhibitors, can reduce the proliferation of abnormal vasculature and mitigate the impact of PFV on ocular structures. Clinical trials are currently underway to assess the efficacy and safety of anti-angiogenic therapies in PFV management.
Regenerative Medicine and Stem Cell Therapy
Regenerative medicine and stem cell therapy have the potential to heal and regenerate damaged ocular tissues in PFV patients. These cutting-edge approaches take advantage of stem cells’ regenerative ability to restore normal ocular function and improve visual outcomes.
Mesenchymal Stem Cell Therapy: Mesenchymal stem cells (MSCs) can differentiate into a variety of cell types and secrete bioactive molecules that promote tissue repair and reduce inflammation. MSCs can be injected into the vitreous cavity or other affected ocular tissues to help repair damaged structures and improve visual function. Preclinical studies have yielded promising results, and clinical trials are currently underway to determine the safety and efficacy of MSC therapy in PFV patients.
Retinal Progenitor Cell Transplantation Retinal progenitor cells (RPCs) are a type of stem cell that can differentiate into retinal cells, and they have the potential to repair damaged retinal tissue in patients with PFV. RPC transplantation involves injecting these cells into the vitreous cavity, where they can integrate into the retina and help with tissue regeneration. Early-stage clinical trials have demonstrated the feasibility and safety of RPC transplantation, and additional research is being conducted to optimize the technique and assess its long-term benefits.






