Fuchs’ Dystrophy is a progressive eye disease that primarily affects the endothelial layer of the cornea, leading to corneal swelling, reduced visual acuity, and significant discomfort. Over the past two decades, corneal surgeons have sought better and more sophisticated solutions to address the failure of the endothelium—one of the most critical layers ensuring corneal clarity. Descemet Membrane Endothelial Keratoplasty (DMEK) has emerged as a leading-edge surgical procedure that selectively replaces only the diseased endothelial layer with healthy donor tissue. By preserving the integrity of most of the patient’s native cornea, DMEK offers more predictable and often dramatic improvements in vision compared to older techniques. Below is a comprehensive exploration of how DMEK works, why it’s considered the “gold standard” for Fuchs’ Dystrophy, and what patients can expect before, during, and after this transformative procedure.
1. Redefining Corneal Transplantation: An Overview of DMEK
Descemet Membrane Endothelial Keratoplasty (DMEK) is a partial-thickness corneal transplant procedure aimed at replacing only the dysfunctional endothelial layer of the cornea. Unlike older grafting methods—such as full-thickness penetrating keratoplasty (PK) or even Descemet Stripping Endothelial Keratoplasty (DSEK)—DMEK involves transplanting a much thinner layer of donor tissue, which is basically Descemet’s membrane plus the healthy donor endothelial cells.
How DMEK Stands Out
- Precision and Selectivity
DMEK addresses just the endothelial layer, approximately 10 to 15 microns in thickness. Traditional transplants may replace multiple corneal layers, sometimes unnecessarily. - Quicker Visual Recovery
Because it preserves the patient’s native stromal and epithelial layers, DMEK often results in faster resolution of corneal edema. Patients frequently notice substantial improvement in vision within weeks to a few months. - Reduced Rejection Risks
With DMEK, the transplanted tissue is less immunogenic, lowering the probability of graft rejection compared to full-thickness grafts or thicker lamellar techniques.
Ideal Candidates for DMEK
- Fuchs’ Endothelial Dystrophy: The leading indication, as Fuchs’ primarily affects the endothelial cells responsible for fluid regulation in the cornea.
- Other Endothelial Pathologies: Patients with bullous keratopathy or endothelial failure post-surgery may be considered if the rest of the cornea remains healthy.
- Desire for Faster, Superior Visual Outcomes: Individuals seeking to minimize complications and expedite clarity find DMEK appealing.
By zeroing in solely on what needs replacement, DMEK stands as a quintessential example of minimally invasive corneal surgery. Up next, an in-depth look at Fuchs’ Dystrophy itself explains why focusing on the endothelium can have such profound implications for ocular health.
2. Fuchs’ Dystrophy: Unraveling the Culprit Behind Endothelial Failure
Fuchs’ Dystrophy is a hereditary condition, named after Austrian ophthalmologist Ernst Fuchs. Its hallmark is the progressive loss of endothelial cells—the corneal layer responsible for pumping excess fluid out of the stroma. As cells are lost, corneal edema and haziness ensue, eventually causing visual impairment.
Fuchs’ Dystrophy in Brief
- Genetic Underpinnings
Fuchs’ Dystrophy often follows an autosomal dominant inheritance pattern with incomplete penetrance, meaning not all individuals with the mutation develop severe disease. Variants in the TCF4 gene, among others, have been associated with the condition. - Stages of Disease
- Early or Preclinical: Patients may remain asymptomatic, with slight corneal guttata (tiny bumps on Descemet’s membrane) visible under slit-lamp exam.
- Mild to Moderate: Individuals begin noticing fluctuating vision, especially upon waking, due to overnight swelling. Corneal guttata becomes more pronounced.
- Severe: Chronic swelling leads to persistent hazy vision, glare, halos around lights, and in advanced cases, painful bullae on the cornea.
- Symptoms Impact
Fuchs’ Dystrophy can significantly reduce quality of life. Activities like driving at night become challenging, and reading or working in bright environments can be hampered by glare and blurred vision.
Conventional Therapies
Before DMEK, patients might rely on:
- Hypertonic Solutions: Eye drops (e.g., 5% sodium chloride) that temporarily draw fluid out of the cornea.
- Hair Dryer Method: Some doctors recommend using a blow dryer at arm’s length upon waking, to evaporate corneal fluid.
- PK or DSEK: Historically, full-thickness grafts or partial-thickness endothelial keratoplasty were the main surgical routes.
However, many of these measures offer incomplete or short-lived relief. DMEK stands poised as a more refined surgical approach that directly tackles the root cause: nonfunctioning endothelium. The next section outlines precisely how DMEK achieves this targeted fix by outlining the procedure’s core mechanics.
3. Targeted Repair: How DMEK Restores Corneal Clarity
Descemet Membrane Endothelial Keratoplasty is fundamentally about exchanging diseased endothelium for healthy donor tissue. This approach spares about 95% of the patient’s cornea, making it a remarkably precise surgery. Below is a detailed glimpse into the step-by-step process.
Preparing the Patient
- Comprehensive Eye Exam: Surgeons examine corneal thickness (pachymetry), endothelial cell counts (if possible), and rule out any coexisting pathologies like cataracts or macular disease.
- Preoperative Counseling: Patients learn about possible outcomes, the importance of air/gas bubble positioning post-op, and the extended follow-up regimen.
Donor Tissue Preparation
- Harvesting the Endothelium
Eye banks prepare the donor tissue by carefully peeling away Descemet’s membrane (with intact endothelium) from a healthy donor cornea. - Storage Medium
The micro-thin donor graft is stored in a specialized fluid until surgery, ensuring cell viability.
Surgical Steps
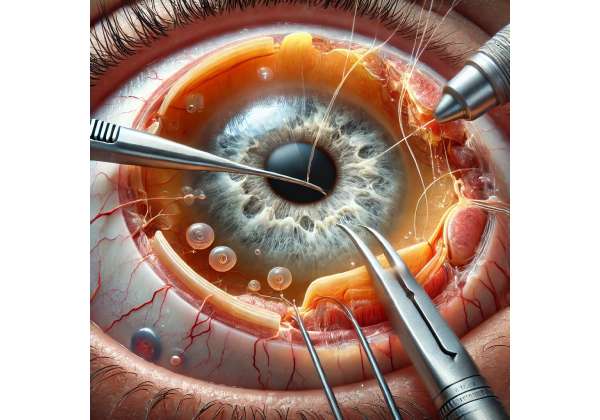
- Removing Diseased Descemet’s Membrane
The surgeon creates a small incision and uses microinstruments or a reverse Sinskey hook to detach and strip the patient’s malfunctioning endothelium along with Descemet’s membrane—a process sometimes called “Descemet Stripping.” - Inserting Donor Graft
The donor membrane is rolled or folded into a slim tube-like shape and gently injected into the anterior chamber. Under a microscope, the surgeon unrolls and positions the tissue. - Air or Gas Bubble
A carefully measured air or gas bubble is introduced to press the new endothelial layer against the stromal interface, encouraging it to adhere properly. - Incision Closure
Small corneal incisions often self-seal or might be sutured with ultrafine stitches. Patients typically remain face-up post-op for several hours to help the graft adhere.
Why DMEK’s Thin Grafts Matter
- Minimal Refractive Changes: Substituting only the endothelium avoids shifting corneal shape or introducing significant astigmatism.
- Faster Restoration of Vision: The cornea regains clarity rapidly since fewer layers intervene between the outside world and the patient’s retina.
- Less Immune Attack: The reduced amount of donor tissue lowers the target for rejection, often resulting in milder rejection episodes if they occur at all.
Once the graft is in place, a well-orchestrated follow-up protocol helps ensure successful healing. The next section clarifies the ins and outs of how surgeons and patients collaborate to keep that graft well-positioned, healthy, and stable in the weeks and months after surgery.
4. Putting DMEK into Practice: Application and Postoperative Care
DMEK is an outpatient procedure in many modern eye centers, but success hinges on careful management from surgery day through the subsequent weeks. Patients who follow recommended guidelines typically enjoy better, longer-lasting results.
Immediate Postoperative Protocol
- Air Bubble Positioning
Patients often lie flat on their back for several hours immediately after surgery, ensuring the bubble supports the graft. Some surgeons advise repeating this positioning periodically for a day or two to bolster adhesion. - Eye Shield and Drops
An eye shield or patch is usually placed for protection. Additionally, patients begin a regimen of antibiotic and steroid eye drops to prevent infection and modulate inflammation.
Follow-Up Visits
- 24-Hour Check: Surgeons confirm that the graft remains centered, and the air bubble is adequate. They also check intraocular pressure (IOP).
- 1-Week Appointment: The bubble typically shrinks or dissipates, and doctors verify partial adherence. Visual acuity improvements may start to appear.
- 1-Month and Beyond: By this stage, many patients see a significant drop in corneal edema, with vision continuing to improve over the next few months. Additional air or gas injections (known as “rebubbling”) might be performed if partial graft detachment occurs.
Potential Complications
While DMEK boasts high success rates, there are a few notable risks:
- Graft Detachment
The ultra-thin donor membrane can detach partially or fully, requiring rebubbling. However, partial detachments occasionally self-resolve or can be reattached with minimal intervention if discovered early. - Increased Intraocular Pressure
Pressure spikes may arise due to steroid-induced ocular hypertension or excessive air bubble size, which is why frequent checks are key. - Endothelial Rejection
Though less common than in full-thickness grafts, rejection remains possible. Patients must watch for redness, pain, or decreased vision and promptly report these signs.
Lifestyle and Recovery
- Visual Rehabilitation: Many individuals resume normal tasks within days, but best visual acuity can take 1 to 3 months to fully stabilize.
- Avoiding Eye Trauma: Low-impact routines and wearing protective eyewear during strenuous activity is recommended.
- Medication Compliance: Regular steroid drops are typically continued for several months to minimize rejection risk.
Adhering to these protocols helps patients maximize the swift, often dramatic gains in visual clarity. However, patient trust in the procedure also stems from robust scientific validation—something the following section covers in detail by exploring the surgery’s effectiveness and safety track record.
5. Real-World Success: Reviewing DMEK’s Effectiveness and Safety
Endothelial keratoplasty techniques have revolutionized corneal surgery by focusing only on the failing endothelial layer. DMEK stands at the forefront, frequently cited as the best approach for advanced Fuchs’ Dystrophy. Below is an overview of the procedure’s effectiveness and safety metrics as reflected in clinical data.
Rapid and Significant Visual Recovery
- Recovery Timeline
- Early Gains: By the first postoperative week, many patients see a measurable reduction in corneal edema. Colors become crisper, and visual clarity improves daily.
- Month 1–3: Significant leaps in best-corrected visual acuity (BCVA) occur, with many individuals reaching 20/25 or better depending on the baseline.
- Long-Term Stability: Once stabilized, results are typically sustained for years, provided post-op care is maintained.
- Contrast Sensitivity
DMEK recipients often experience improved contrast sensitivity—crucial for seeing in low-light environments—thanks to minimal changes in corneal architecture.
Low Rejection Rates
- Incidence: Studies report rejection episodes in DMEK at rates of about 1–5%, which is notably lower than in older grafting methods.
- Early Intervention: When recognized promptly, rejection episodes typically respond well to topical steroids, preserving graft function.
Comparisons with DSEK/DSAEK
- Thickness Differences: DSEK grafts are typically 100–200 microns thick, while DMEK tissue is often under 20 microns. This disparity yields better visual clarity with DMEK.
- Less Graft Dislocation: While DSEK dislocation rates can be significant, DMEK’s dislocation risk is somewhat offset by meticulous technique. That said, DMEK does require advanced surgical skill, meaning specialized training is essential.
Ongoing Surgical Refinements
- Pre-Loaded Tissues: Some eye banks now deliver pre-loaded DMEK scrolls, simplifying the surgery.
- Automated Tissue Preps: Machine-based donor tissue prep further reduces manual error, though it’s an area of continuing development.
Quality of Life Outcomes
From reading fine print to driving at dusk, patients consistently report significant life improvements post-DMEK. The minimal incision approach often leaves minimal astigmatism, ensuring both near and distance tasks are easier. With success rates frequently surpassing 90%, DMEK has solidified its position as a leading corneal transplant technique.
Armed with these compelling safety and efficacy figures, many potential recipients and practitioners look to the latest research for ongoing developments that might refine or extend the procedure’s benefits. The next section delves into that ever-expanding body of knowledge.
6. Ongoing Innovation: Latest Research Insights on DMEK
DMEK’s rise in corneal transplant circles has spurred an explosion of studies exploring everything from refined surgical maneuvers to advanced imaging. The collective findings reinforce DMEK’s role as a top-tier intervention for endothelial diseases like Fuchs’ Dystrophy.
1. Large-Scale Multicenter Trials
- Visual Acuity Benchmarks: Trials show that over 70–80% of eyes can achieve 20/25 vision or better after DMEK. Many centers confirm these results hold true across wide patient populations and varying severities of Fuchs’ Dystrophy.
- Longevity of Grafts: Follow-up data suggest stable outcomes for 5+ years, with minimal corneal decompensation or need for regrafts.
2. Big Data Registries
Organizations like the Cornea Society and national eye bank registries collaborate to gather outcome metrics. Preliminary analyses highlight:
- Steady or Declining Detachment Rates: As surgeons gain proficiency, detachment incidences drop well below 10% in many high-volume centers.
- Low Secondary Interventions: Most eyes do not require repeated surgeries, distinguishing DMEK from older methods where regrafts were more common.
3. Sweeping Technological Advances
- Ultra-High-Resolution OCT: Imaging advancements help surgeons assess graft orientation and thickness in real-time, potentially reducing complications.
- Gene Therapy and Pharmacological Aids: Some labs investigate whether regenerative peptides or gene therapy might further reinforce the newly transplanted endothelium.
4. Special Subgroups and Combination Procedures
- Phakic vs. Pseudophakic Eyes: Combined cataract surgery with DMEK is increasingly typical for older patients. Studies find no major compromise in DMEK results when performed simultaneously with lens removal.
- Preexisting Glaucoma: New research examines how to optimize outcomes for patients with borderline or advanced glaucoma, balancing IOP management with graft viability.
5. Surgeons’ Experience: The Learning Curve
Because DMEK demands precise tissue handling, research emphasizes the importance of a surgeon’s experience. Many propose that once a surgeon surpasses the initial learning curve (often 20–30 cases), complication rates drop drastically, and outcomes align with those seen in expert centers worldwide.
In sum, the constantly evolving scientific consensus cements DMEK as a hallmark procedure for Fuchs’ Dystrophy. Next, one practical concern remains: finances. The section below navigates therapy costs, insurance coverage, and patient support resources.
7. The Financial Side: Therapy Price Considerations for DMEK
The expense of DMEK can vary widely by region, hospital system, and insurance structure. Despite the procedure’s relative novelty, it often falls under corneal transplant reimbursements, given its recognized clinical success.
Typical Price Range and Influencing Factors
Procedure costs may average $4,000 to $8,000 per eye in many parts of the United States. However, this figure may rise or fall based on:
- Donor Tissue Fees: Eye banks charge fees for donor corneas, factoring in costs of screening, shipping, and tissue preparation.
- Surgical Setting: Outpatient surgical centers might be more economical than inpatient hospital settings.
- Insurance Coverage: Public health services (like Medicare in the U.S.) or private insurers typically cover a significant portion if the surgery is deemed medically necessary to restore vision.
Potential Out-of-Pocket Costs
- Co-Pays and Deductibles: Patients with higher deductible plans or partial coverage may need to cover a portion of the surgical and facility fees.
- Follow-Up and Medications: Steroid drops or additional visits for rebubbling can add incremental costs. Some or all may be covered under comprehensive policies.
- Financing Options: Many practices collaborate with financing companies that offer monthly payment plans for uncovered expenses.
Patient Assistance and Grants
Select non-profits or government assistance programs provide grants or low-interest medical loans for corneal transplantation procedures, especially for those with limited income. Engaging with a clinic’s billing department early in the process helps clarify potential financial burdens and identifies any charitable avenues.
Disclaimer:
This article is intended for informational purposes only and should not be construed as medical advice. Always seek the guidance of a qualified medical professional regarding any eye condition or potential treatments.
We invite you to share this article with friends, family, or on social platforms such as Facebook and X (formerly Twitter). By spreading knowledge about DMEK’s transformative role in treating Fuchs’ Dystrophy, you can help individuals struggling with corneal disease make informed decisions that could improve their vision—and their lives.