Pseudopapilledema is a condition in which the optic disc appears swollen, similar to true papilledema but without the underlying cause of elevated intracranial pressure (ICP). Pseudopapilledema optic disc swelling is usually benign and caused by congenital or developmental anomalies such as optic disc drusen, hyperopia, or other structural irregularities. Unlike true papilledema, which is a medical emergency requiring immediate treatment, pseudopapilledema generally does not endanger vision or overall health.
Pathophysiology
The primary distinction between pseudopapilledema and true papilledema is in the underlying causes. In true papilledema, increased ICP causes optic disc swelling, which can indicate serious conditions such as intracranial tumors, hydrocephalus, or brain hemorrhage. Pseudopapilledema, on the other hand, is caused by anatomical variations or benign conditions, and there is no associated increase in ICP.
Optical Disc Drusen
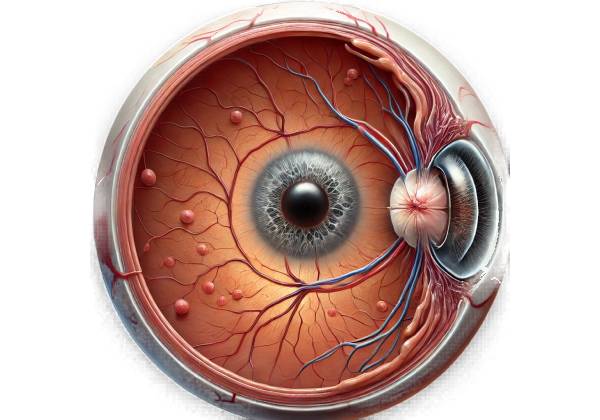
Optical disc drusen is one of the most common causes of pseudopapilledema. These are calcified deposits that accumulate in the optic nerve head, giving the appearance of swelling. Optic disc drusen are typically congenital, but they can become more visible with age. They can be buried within the optic disc or visible from the surface. The exact cause of optic disc drusen is unknown, but it is thought to be abnormal axoplasmic flow in the optic nerve.
Hyperopia
High hyperopia (farsightedness) can also result in pseudopapilledema. Because of the eye’s shorter axial length, hyperopic eyes may have an elevated and crowded optic disc. This anatomical configuration can give the false impression that the optic disc is swelling.
Other Structural Anomalies
Other congenital or developmental anomalies, such as crowded optic nerve heads or small optic cups, may also cause pseudopapilledema. These conditions are typically benign and do not indicate underlying pathology.
Epidemiology
Pseudopapilledema can occur at any age, but it is most commonly detected during childhood or adolescence due to congenital factors such as optic disc drusen. The prevalence of pseudopapilledema is unknown, owing to its benign nature and the fact that it is not always clinically significant. However, optic disc drusen are thought to occur in 0.3% to 2% of the general population.
Clinical Presentation
The clinical presentation of pseudopapilledema varies according to the underlying cause. However, there are some similarities that help distinguish it from true papilledema:
- Visual Symptoms: The majority of patients with pseudopapilledema are asymptomatic and only discover the condition during routine eye exams. In some cases, patients may experience transient visual disturbances such as flickering lights or brief episodes of vision loss, particularly if the optic disc is drusen.
- Fundoscopic Appearance: A fundoscopic examination reveals an elevated and swollen optic disc. However, unlike true papilledema, there are rarely any associated hemorrhages, cotton-wool spots, or exudates. Optic disc drusen may appear as yellowish, glistening deposits on the optic disc.
- Visual Fields: Visual field testing can reveal peripheral field defects, such as arcuate scotomas, which are associated with optic disc drusen. These defects are usually stable and non-progressive.
- Optic Nerve Function: In most cases, pseudopapilledema preserves optic nerve function. Patients do not experience severe vision loss or other neurological symptoms associated with true papilledema.
Differential Diagnosis
It is critical to distinguish pseudopapilledema from true papilledema and other conditions that present similarly. Differential diagnosis includes:
- True Papilledema: True papilledema is caused by elevated ICP and manifests as bilateral optic disc swelling, which is frequently accompanied by symptoms such as headache, nausea, vomiting, and transient visual obscuration. Neuroimaging and lumbar puncture are necessary to confirm elevated ICP.
- Papillitis: Inflammation of the optic nerve head, papillitis can cause optic disc swelling and is frequently associated with pain, vision loss, and a relative pupillary defect. Infections, optic neuritis, and inflammatory diseases are all possible causes.
- Ischemic Optic Neuropathy: This condition causes sudden vision loss due to reduced blood flow to the optic nerve head, resulting in disc swelling. It is distinguishable from pseudopapilledema by its sudden onset and associated vascular risk factors.
- Malignant Hypertension: Severe hypertension can result in optic disc swelling due to hypertensive retinopathy. Blood pressure measurement and systemic evaluation are essential for diagnosing this condition.
- Diabetic Papillopathy: Diabetic papillopathy is a rare complication of diabetes characterized by mild optic disc swelling. It is frequently self-limiting and distinguishable from pseudopapilledema by the presence of diabetic retinopathy and systemic diabetes management.
Complications
Pseudopapilledema is generally benign and does not cause significant complications. However, there are some risks associated with misdiagnosis.
- Overtreatment: Misinterpreting pseudopapilledema as true papilledema can result in unnecessary and invasive procedures, such as neuroimaging and lumbar puncture.
- Underdiagnosis: Failure to detect true papilledema in a patient with optic disc swelling can delay the diagnosis of serious underlying conditions, such as intracranial tumors or hydrocephalus, which require immediate treatment.
- Visual Field Defects: Although rare, some patients with optic disc drusen may develop progressive visual field loss over time. Visual fields should be monitored on a regular basis to detect changes early on.
Prognosis
The prognosis for patients with pseudopapilledema is generally good, especially if the condition is correctly identified and monitored. The majority of patients do not experience significant visual impairment or progression of symptoms. Individuals with optic disc drusen should be monitored for complications such as visual field loss or choroidal neovascularization.
Methods to Diagnose Pseudopapilledema
A comprehensive clinical evaluation is required to diagnose pseudopapilledema, which includes a detailed patient history, a thorough eye examination, and specialized imaging studies. The goal is to differentiate pseudopapilledema from true papilledema and other causes of optic disc swelling in order to guide appropriate treatment.
Clinical Examination
- Visual Acuity Testing: Measuring visual acuity is useful in determining the effect of optic disc swelling on vision. The majority of patients with pseudopapilledema have normal or near-normal visual acuity.
- Slit-Lamp Examination: A slit-lamp examination provides detailed visualization of the anterior segment of the eye, assisting in the identification of any associated anomalies or signs of inflammation.
- Fundoscopic Examination: Direct or indirect ophthalmoscopy is essential for evaluating the optic disc. In pseudopapilledema, the optic disc is elevated and swollen, with visible drusen. The absence of hemorrhages, cotton-wool spots, and exudates distinguishes it from true papilledema.
- Gonioscopy: This examination assesses the anterior chamber angle and can reveal other structural abnormalities that may contribute to optic disc swelling.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and optic nerve head. It aids in the detection of optic disc drusen as well as the thickness of the retinal nerve fiber layer (RNFL), which can be increased in pseudopapilledema.
- B-Scan Ultrasonography: B-scan ultrasonography is a non-invasive imaging technique that can detect buried optic disc drusen by producing cross-sectional images of the optic nerve head. It is especially useful when drusen are not visible during a fundoscopic examination.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and taking a series of photographs of the retina. It aids in the assessment of retinal blood flow and distinguishes optic disc drusen from other causes of disc swelling, as drusen do not typically leak dye.
- Fundus Autofluorescence (FAF): FAF imaging detects the natural fluorescence emitted by specific structures in the eye, such as the optic disc drusen. This technique aids in the visualization of drusen and differentiates them from other causes of optic disc elevation.
Specialized Tests
- Visual Field Testing: Automated perimetry, such as the Humphrey Visual Field Analyzer, maps the patient’s visual field by presenting light stimuli in different locations and recording the responses. This test detects common visual field defects associated with optic disc drusen, including arcuate scotomas and peripheral field loss.
- Electroretinography (ERG): ERG assesses retinal cells’ electrical responses to light stimuli. It provides information on retinal function and aids in distinguishing pseudopapilledema from other retinal conditions that exhibit similar symptoms.
- Neuroimaging: If the diagnosis is uncertain or there are atypical features, magnetic resonance imaging (MRI) or computed tomography (CT) may be used to rule out intracranial pathology. These tests can help detect elevated ICP or other abnormalities associated with true papilledema.
Pseudopapilledema Management
The primary goal of managing pseudopapilledema is to carefully monitor and address any underlying conditions that may be contributing to the appearance of the optic disc. Because pseudopapilledema is typically benign and does not require aggressive treatment, the emphasis is on distinguishing it from true papilledema and avoiding unnecessary interventions.
Monitoring and Observation
- Regular Eye Examinations: Patients diagnosed with pseudopapilledema should see an ophthalmologist on a regular basis to monitor any changes in their condition. This includes routine visual acuity tests, fundoscopic exams, and imaging studies to monitor the stability of optic disc drusen or other structural abnormalities.
- Visual Field Testing: Regular visual field tests are critical for detecting changes in vision that could indicate progression or complications. Early detection of visual field defects can help guide future management and intervention, if necessary.
Addressing the Underlying Conditions
- Management of Hyperopia: Corrective lenses or contact lenses can help patients with hyperopia who suffer from pseudopapilledema by optimizing vision and reducing eye strain. This does not directly treat pseudopapilledema, but it does improve overall visual function.
- Systemic Health Monitoring: Because optic disc drusen can occasionally be associated with systemic conditions such as connective tissue disorders, a comprehensive systemic evaluation may be required. Collaboration with primary care physicians or specialists can help to manage any related health issues.
Managing Risks and Complications
- Patient Education: Educating patients on the benign nature of pseudopapilledema is critical for reducing anxiety and ensuring adherence to monitoring schedules. Patients should be aware of the signs and symptoms that require immediate medical attention, such as sudden vision changes or headaches.
- Avoiding Unnecessary Interventions: Differentiating pseudopapilledema from true papilledema is critical for avoiding unnecessary diagnostic tests and invasive procedures such as lumbar punctures or neuroimaging. Accurate diagnosis and clear communication with patients and other healthcare providers can help to avoid these interventions.
Surgical Interventions
Pseudopapilledema rarely requires surgical intervention. However, if optic disc drusen cause significant visual field loss or complications like choroidal neovascularization, surgical options may be considered:
- Laser Photocoagulation: Laser photocoagulation can help manage abnormal blood vessels and prevent further vision loss in patients with choroidal neovascularization due to optic disc drusen.
- Vitrectomy: In rare cases, when optic disc drusen cause severe visual impairment or other complications, vitrectomy may be considered. This surgical procedure removes the vitreous gel from the eye and is usually reserved for severe cases.
Ongoing Research and Emerging Therapies
The pathophysiology and treatment of pseudopapilledema are currently being studied. Emerging therapies and advances in imaging technology are helping to improve our understanding and treatment of this condition. Patients and healthcare providers should be aware of new developments that may provide additional diagnostic or therapeutic options in the future.
Trusted Resources and Support
Books
- “Neuro-Ophthalmology Illustrated” by Valérie Biousse and Nancy J. Newman: This comprehensive book provides detailed information on neuro-ophthalmic conditions, including pseudopapilledema. It offers valuable insights for both clinicians and patients.
- “Clinical Pathways in Neuro-Ophthalmology: An Evidence-Based Approach” by Andrew G. Lee and Paul W. Brazis: This book covers a wide range of neuro-ophthalmic disorders, providing evidence-based approaches to diagnosis and management, with relevant information on pseudopapilledema.
Organizations
- American Academy of Ophthalmology (AAO): The AAO provides extensive resources, guidelines, and continuing education for ophthalmologists and patients dealing with various eye conditions, including pseudopapilledema. AAO Website
- North American Neuro-Ophthalmology Society (NANOS): NANOS is a professional organization dedicated to the field of neuro-ophthalmology. It offers educational resources, research updates, and patient information on conditions like pseudopapilledema. NANOS Website
- National Eye Institute (NEI): Part of the National Institutes of Health, the NEI conducts and supports research on eye diseases and provides comprehensive educational resources on various ocular conditions, including pseudopapilledema. NEI Website






