What is Hereditary Optic Neuropathy?
Hereditary optic neuropathies are a class of genetic disorders marked by progressive degeneration of the optic nerves, resulting in visual impairment. These conditions are inherited and can occur at any stage of life, from infancy to adulthood. The two most prevalent types are Leber’s hereditary optic neuropathy (LHON) and dominant optic atrophy (DOA). Patients with these conditions usually have a gradual loss of vision, beginning with central vision and progressing to more severe visual deficits. Understanding the genetics and clinical manifestations of these disorders is critical for diagnosis and treatment.
Comprehensive Investigation of Hereditary Optic Neuropathies
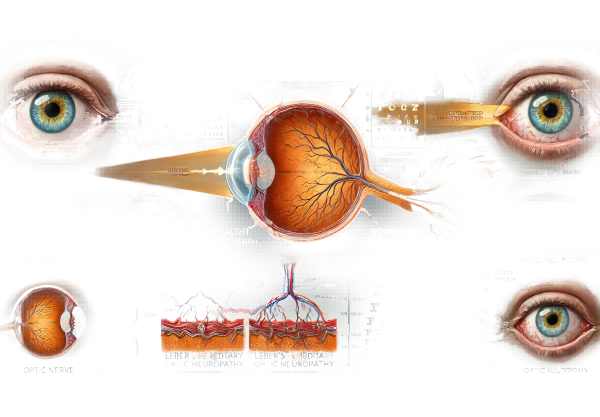
Hereditary optic neuropathies are a group of genetic disorders that cause optic nerve degeneration, which results in vision loss. The optic nerves’ primary function is to transfer visual information from the retina to the brain. When these nerves deteriorate, visual acuity suffers, limiting an individual’s ability to perform daily tasks. The most common types of hereditary optic neuropathies are Leber’s hereditary optic neuropathy (LHON) and dominant optic atrophy (DOA), which have distinct genetic and clinical characteristics.
Leber’s Hereditary Optic Neuropathy(LHON)
LHON is a mitochondrial genetic disorder that primarily affects young males, though females may also be affected. It is caused by mutations in mitochondrial DNA (mtDNA), which is inherited from the mother. LHON is most commonly associated with mutations in the ND1, ND4, and ND6 genes, which encode components of the mitochondrial respiratory chain complex I.
Pathophysiology
Mutations in LHON disrupt the mitochondrial respiratory chain’s normal function, resulting in decreased ATP production and increased production of reactive oxygen species. This mitochondrial dysfunction selectively damages retinal ganglion cells (RGCs) and their axons, particularly those that form the optic nerve, causing progressive vision loss.
Clinical Manifestations
LHON patients typically present with acute or subacute painless vision loss in one eye, followed by similar vision loss in the other eye within a few weeks or months. Vision loss primarily affects central vision, resulting in a central scotoma, which is a missing portion of the visual field. This can severely impair activities such as reading and facial recognition. In some cases, peripheral vision is relatively intact, but severe cases can result in legal blindness.
Dominant optic atrophy (DOA)
DOA is another common form of hereditary optic neuropathy with autosomal dominant inheritance. The most frequently implicated gene in DOA is OPA1, which is found on chromosome 3. OPA1 encodes a protein required for mitochondrial function and structure.
Pathophysiology
Mutations in OPA1 cause mitochondrial dysfunction and impaired membrane fusion. This causes a loss of mitochondrial DNA integrity and decreased energy production, affecting retinal ganglion cells and their axons in a manner similar to LHON.
Clinical Manifestations
DOA typically presents in the first decade of life as a gradual, painless loss of vision. DOA, unlike LHON, causes bilateral vision loss that progresses slowly. Patients frequently report a central or centrocecal scotoma, decreased color vision, and reduced visual acuity. The severity of vision loss varies greatly among affected individuals, with some maintaining relatively good vision while others suffer significant impairment.
Other Types of Hereditary Optic Neuropathy
While LHON and DOA are the most common types, other hereditary optic neuropathies exist, often with similar clinical features. This includes:
- Behr Syndrome is a rare condition marked by early-onset optic atrophy, ataxia, spasticity, and developmental delays.
- The Wolfram Syndrome: This syndrome, also known as DIDMOAD (diabetes insipidus, diabetes mellitus, optic atrophy, and deafness), is caused by mutations in the WFS1 gene and results in progressive vision loss, among other systemic issues.
- OPA3-related optic atrophy: This condition, caused by mutations in the OPA3 gene, is linked to early-onset optic atrophy and may be accompanied by other neurological symptoms.
Gene Basis and Inheritance Patterns
Hereditary optic neuropathies are typically inherited in three ways: mitochondrial, autosomal dominant, and autosomal recessive.
- Mitochondrial Inheritance: As seen in LHON, mutations occur in mitochondrial DNA and are passed down from mother to offspring.
- Autosomal Dominant Inheritance: As seen in DOA, a single copy of the mutated gene inherited from one parent is enough to cause the disorder.
- Autosomal Recessive Inheritance: The mutated gene must be present in two copies, one from each parent, as seen in some rarer forms such as Behr Syndrome.
Effects on Quality of Life
Hereditary optic neuropathies have a significant impact on quality of life because vision loss progresses over time. Patients frequently encounter difficulties in education, employment, and daily living activities. The psychological effects can be severe, resulting in anxiety, depression, and social isolation. Early detection, genetic counseling, and assistance from healthcare providers and support groups are critical for overcoming these obstacles.
Diagnostic methods
Hereditary optic neuropathies are diagnosed using a combination of clinical evaluation, imaging studies, and genetic tests. Early and accurate diagnosis is critical for effective treatment and genetic counseling.
Clinical Evaluation
A thorough clinical examination is the first step in diagnosing hereditary optic neuropathies. This includes:
- Patient History: Detailed documentation of the onset, progression, and nature of visual symptoms, as well as a family history of related conditions.
- Visual Acuity Testing: Measuring central and peripheral vision to determine the degree of vision loss.
- Ophthalmoscopic Examination: Examine the optic disc for signs of pallor or atrophy, which may indicate optic neuropathy.
Imaging Studies
Imaging studies are essential for visualizing the optic nerves and retinal structures.
- Optical Coherence Tomography (OCT): Produces high-resolution cross-sectional images of the retina, allowing for detailed evaluation of RNFL thickness and ganglion cell layer integrity.
- Magnetic Resonance Imaging (MRI) is used to rule out other possible causes of optic neuropathy, such as compressive lesions or demyelinating diseases.
Genetic Testing
Genetic testing is the definitive method for diagnosing hereditary optic neuropathies, which involves analyzing DNA samples to identify specific mutations associated with the condition. This includes:
- Mitochondrial DNA Analysis: Used to detect common mutations in LHON, such as those in the ND1, ND4, and ND6 genes.
- Nuclear DNA Analysis: To detect mutations in genes such as OPA1 in DOA and other relevant genes in less common forms of hereditary optic neuropathies.
Electrophysiological Tests
Electrophysiological tests can provide more information about optic nerve function.
- Visual Evoked Potentials (VEP): Measures electrical activity in the brain in response to visual stimuli, which aids in determining the functional integrity of optic pathways.
Treatment
The goal of treating hereditary optic neuropathies is to alleviate symptoms, slow disease progression, and improve quality of life. Currently, there is no cure, but several approaches can help reduce the severity of these conditions.
- Nutritional Supplements: High-dose vitamins and antioxidants, such as vitamin B12, vitamin C, vitamin E, and coenzyme Q10, are frequently used to promote mitochondrial function and protect against oxidative stress. In LHON, idebenone, a synthetic analogue of coenzyme Q10, has shown promise in improving visual outcomes, especially when administered early in the disease course.
- Supportive Therapies: These include low vision aids, occupational therapy, and mobility training, which help patients adapt to vision loss and maintain their independence. Assistive technologies, such as screen readers and magnification devices, can help people perform everyday tasks and access information.
- Genetic Counseling: Providing genetic counseling to patients and their families is critical for understanding inheritance patterns, family implications, and testing options. It also provides psychological support and assistance in family planning decisions.
Innovative and Emerging Therapies
- Gene Therapy: Gene therapy is a promising field of study for hereditary optic neuropathy. This method involves delivering a functional copy of the defective gene to the affected cells. Clinical trials for LHON using adeno-associated viral (AAV) vectors to deliver the ND4 gene have yielded promising results, with some patients seeing significant visual improvement.
- Mitochondrial Replacement Therapy: This novel approach seeks to replace damaged mitochondria with healthy ones. While still in experimental stages, mitochondrial replacement therapy has the potential to treat mitochondrial disorders such as LHON by restoring normal mitochondrial function.
- Pharmacological Approaches: Researchers are looking into drugs that improve mitochondrial function and cellular energy production. Agents such as EPI-743, a synthetic analogue of vitamin E, are being tested for their ability to improve mitochondrial function and protect retinal ganglion cells.
- Stem Cell Therapy: Stem cell therapy is an emerging field that has the potential to regenerate damaged optic nerve cells. Preclinical studies have shown that stem cell transplantation can promote retinal ganglion cell survival and regeneration, though this is still in the experimental phase.
Clinical trials
Participating in clinical trials gives patients access to cutting-edge therapies while also helping to advance our understanding of these conditions. Patients with hereditary optic neuropathies should speak with their doctors about current clinical trials and the potential benefits of participating.
Combining these treatment strategies can help healthcare providers better manage hereditary optic neuropathies, slowing disease progression and improving affected individuals’ quality of life.
Best Practices to Prevent Hereditary Optic Neuropathy
While hereditary optic neuropathies are genetic and cannot be completely avoided, certain practices can help reduce the risk and improve condition management:
- Genetic Counseling: People with a family history of hereditary optic neuropathies should seek genetic counseling to better understand their risk and explore genetic testing. Early detection enables timely intervention and management.
- Regular Eye Exams: Routine eye exams can aid in detecting early signs of optic neuropathy. Individuals at risk should have comprehensive eye exams once a year, or as recommended by their ophthalmologist.
- Healthy Lifestyle: Maintaining a healthy lifestyle, which includes a balanced diet high in antioxidants, regular exercise, and abstaining from smoking and excessive alcohol consumption, can benefit overall health and potentially alleviate some aspects of mitochondrial dysfunction.
- Avoid Environmental Toxins: Limiting exposure to environmental toxins and chemicals that can exacerbate mitochondrial dysfunction is critical. This includes avoiding tobacco smoke, specific medications, and industrial chemicals.
- Protect Eyes from UV Radiation: Wearing UV-blocking sunglasses can help protect the eyes from damage caused by sunlight.
- Stay Informed: Staying up to date on the latest research and developments in hereditary optic neuropathy can help patients and families make informed decisions about their care and potential participation in clinical trials.
- Prompt Medical Attention: If you experience symptoms like sudden vision loss, seek medical attention right away, especially if you have a family history of hereditary optic neuropathies. Early intervention can help to manage the condition more effectively.
Individuals at risk for hereditary optic neuropathies can take proactive steps to monitor their eye health and potentially reduce the severity of these conditions by implementing these preventive measures.
Trusted Resources
Books
- “Inherited Retinal Diseases: A Diagnostic and Therapeutic Approach” by Stephen H. Tsang
- “Retinal Degenerative Diseases: Mechanisms and Experimental Therapy” by Catherine Bowes Rickman, Matthew M. LaVail, and Christine Grimm
- “Mitochondrial Dysfunction in Neurodegenerative Disorders” by Amy Katherine Reeve and Swee Hong Gee






