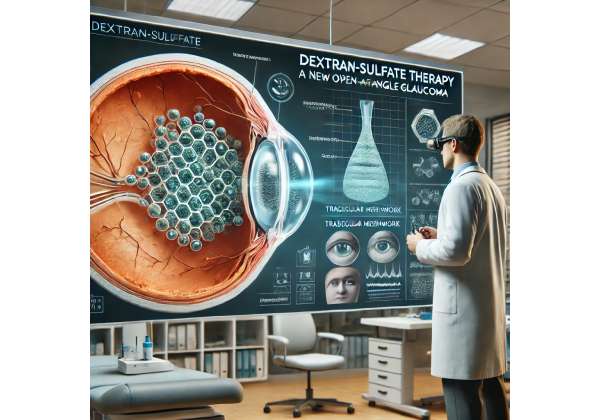
1. A Closer Look at Dextran-Sulfate: Transforming Glaucoma Management
Dextran-sulfate therapy has emerged as a promising anti-fibrotic intervention for open-angle glaucoma, an eye condition that continues to threaten the vision of millions of people worldwide. This innovative approach centers on mitigating the fibrotic processes that often complicate glaucoma management, which traditionally revolves around controlling intraocular pressure (IOP) with topical eye drops, laser procedures, and surgical interventions. While these conventional strategies can help manage the condition, they may not always address the long-term implications of tissue scarring, which can eventually impact the success of surgery and overall management outcomes.
Dextran is a long-chain glucose polymer that has been explored in various medical applications, ranging from plasma expanders to drug delivery systems. The addition of sulfate groups to dextran is what sets dextran-sulfate apart, endowing it with unique properties that make it especially useful in inhibiting fibrosis. Fibrosis, or the excessive buildup of scar tissue, often hinders fluid drainage in the eye’s trabecular meshwork, causing elevated IOP and further damage to the optic nerve. When dextran-sulfate is applied as a targeted therapy, it can help regulate cellular and molecular pathways responsible for excessive collagen deposition, thereby reducing scar formation.
An Evolving Field in Glaucoma Care
For many years, therapeutic options for open-angle glaucoma focused almost exclusively on lowering IOP. While certainly beneficial for slowing the disease, these treatments do not necessarily address the underlying fibrotic changes that happen over time in the drainage structures of the eye. The shift toward anti-fibrotic therapies signals a more comprehensive approach—one that not only emphasizes lowering IOP but also targets the physiological changes that compromise outflow facility.
Several factors have brought dextran-sulfate into the spotlight. First, surgeons who perform trabeculectomy or other glaucoma procedures frequently observe scarring that limits postoperative success. Second, laboratory studies have shown that dextran-sulfate can interfere with certain growth factors, such as TGF-β (Transforming Growth Factor Beta), that promote fibroblast activity and collagen deposition in ocular tissues. Third, the aging population and growing prevalence of glaucoma worldwide highlight the need for novel interventions that work synergistically with standard of care.
Potential Advantages Over Conventional Treatment
Dextran-sulfate therapy offers several potential advantages over more traditional glaucoma treatments:
- Anti-Fibrotic Focus
Conventional therapies mainly aim to reduce intraocular pressure. Dextran-sulfate specifically targets fibrotic processes, which complements the pressure-lowering effects of standard medications and surgeries. - Versatile Formulations
Early research suggests that dextran-sulfate can be integrated into various delivery systems, including topical formulations and sustained-release implants, potentially leading to improved adherence and more consistent therapeutic outcomes. - Targeted Mechanism of Action
Dextran-sulfate interacts directly with molecular pathways responsible for excessive scarring, minimizing the risk of accidental disruption of healthy tissue regeneration while selectively inhibiting problematic fibroblast activity. - Potential Long-Term Benefits
By mitigating fibrotic complications, dextran-sulfate therapy may enhance the longevity of surgical interventions. Patients often require repeat procedures when scarring recurs; an effective anti-fibrotic agent could reduce the frequency of such interventions. - Synergistic Use with Existing Therapies
Dextran-sulfate could potentially serve as an adjunct to prostaglandin analogs, beta-blockers, or other IOP-lowering medications, further expanding a physician’s options for personalized care.
The Road Ahead
Bringing dextran-sulfate therapy from the realm of experimental treatments to a mainstay in clinical practice involves rigorous testing in clinical trials to validate its safety and efficacy. Researchers are investigating optimal dosages, appropriate delivery mechanisms, and any potential drug interactions. For example, preliminary data from pilot studies in Europe and Asia show promising trends in slowing disease progression, but large-scale randomized trials are needed to confirm these findings.
Despite these challenges, dextran-sulfate therapy stands out as a beacon of innovation in glaucoma care. By tackling the under-recognized yet critical component of fibrotic change, this therapy could alter how ophthalmologists approach open-angle glaucoma management. Understanding exactly how this agent functions, how it should be administered, and how it can be integrated into a broader treatment plan is crucial for both practitioners and patients. The sections below will dive deeper into the specifics of open-angle glaucoma, the mechanics of dextran-sulfate, and the proven clinical insights that underpin this new treatment’s promise.
2. Unmasking Open-Angle Glaucoma: A Silent Vision Threat
Open-angle glaucoma (OAG) is the most common form of glaucoma and is frequently referred to as the “silent thief of sight” because it progresses gradually and often without noticeable symptoms until significant vision loss has occurred. This condition involves slow damage to the optic nerve, typically brought on by elevated intraocular pressure. Although raised IOP remains a primary risk factor, many individuals with OAG may experience normal-tension glaucoma, where optic nerve damage occurs even if eye pressure falls within normal ranges.
Prevalence and Global Impact
Over 70 million people worldwide are affected by glaucoma, with open-angle glaucoma comprising a significant portion of these cases. In fact, it ranks among the leading causes of irreversible blindness globally. The asymptomatic nature of early-stage OAG makes regular screening critically important, especially in older adults and in those with a family history of the disease. Certain demographic groups, such as individuals of African descent, also bear a higher risk of developing more aggressive forms of glaucoma.
Key Biological and Anatomical Changes
- Trabecular Meshwork Dysfunction
The trabecular meshwork, a spongy tissue at the drainage angle of the anterior chamber of the eye, is responsible for regulating outflow of aqueous humor. In OAG, degenerative and fibrotic changes in this tissue make it harder for fluid to drain, leading to elevated IOP. - Optic Nerve Vulnerability
The optic nerve, composed of over a million nerve fibers that relay visual information from the retina to the brain, becomes progressively damaged when IOP exceeds the tolerance threshold of these delicate fibers. Even subtle fluctuations in IOP can compound over time, cumulatively weakening the optic nerve. - Neurodegeneration
Researchers are increasingly studying the neurodegenerative aspects of glaucoma, including the role of oxidative stress, mitochondrial dysfunction, and even immune-mediated responses that may contribute to nerve fiber damage. Although the core issue often starts with fluid drainage problems and pressure buildup, neuroprotective treatments are also under investigation.
Symptoms and Early Detection
Most patients with open-angle glaucoma do not notice any change in their vision until significant peripheral vision loss has occurred. This underscores the importance of regular eye examinations—especially for individuals over the age of 40, those with a genetic predisposition, or those with systemic conditions like diabetes. Diagnostic methods include measuring IOP using tonometry, visual field testing to detect blind spots, optical coherence tomography (OCT) to examine the optic nerve head and retinal nerve fiber layer, and a dilated fundus examination to evaluate the optic disc’s shape and health.
Limitations of Traditional Treatments
Historically, the foundational approach to treating OAG has been lowering IOP through topical medications—such as prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors—or via laser procedures like trabeculoplasty. When these fail or disease progression is more advanced, surgical interventions such as trabeculectomy or the implantation of drainage devices (e.g., tube shunts) may be necessary.
While these procedures can be highly effective at reducing IOP, postoperative scarring remains a major challenge. Scar tissue can close off drainage pathways, nullifying the effects of surgery and forcing patients to repeat the procedure or escalate to more invasive options. Additionally, the medications themselves can cause side effects such as redness, irritation, changes in eyelash length, or systemic absorption leading to complications in breathing or heart rate. These factors necessitate the development of adjunct therapies that can bolster the long-term success of glaucoma management.
Why Anti-Fibrotic Therapies Are Gaining Momentum
In recent years, the conversation around glaucoma treatments has begun to shift, with researchers and clinicians recognizing that targeting fibrotic processes could be just as critical as lowering eye pressure. Fibrosis not only poses a significant obstacle to surgical success, but may also play an underappreciated role in disease progression. By limiting the buildup of scar tissue in the trabecular meshwork and surgical sites, anti-fibrotic strategies such as dextran-sulfate therapy can potentially extend the effectiveness of existing therapies and postpone or prevent the need for additional surgical interventions.
Ultimately, understanding OAG as more than just an eye pressure issue paves the way for more comprehensive and effective treatment approaches. By addressing fibrotic pathways head-on, dextran-sulfate therapy is poised to fill an important gap in modern glaucoma care. The next sections delve into how exactly this therapy works at the cellular and molecular levels, explaining the science that fuels its anti-fibrotic promise.
3. Inside the Mechanism: How Dextran-Sulfate Fights Fibrosis
Fibrosis in open-angle glaucoma arises when the normal wound-healing process in ocular tissues, particularly the trabecular meshwork or surgical sites, goes awry. Instead of regenerating in a balanced way, fibroblasts proliferate and deposit excessive extracellular matrix (ECM) proteins such as collagen. The result is scar tissue that stiffens and narrows outflow pathways, elevating IOP and jeopardizing the optic nerve. Dextran-sulfate disrupts these pathological events at multiple levels, leveraging its unique molecular structure to hinder collagen deposition and alter cellular behavior.
Targeted Interaction with Growth Factors
Much of pathological fibrosis is driven by growth factors, especially Transforming Growth Factor Beta (TGF-β). TGF-β is known to upregulate fibroblast activity, boosting the production of collagen and other ECM elements in ocular tissues. Dextran-sulfate contains negatively charged sulfate groups that can bind to positively charged sites on TGF-β, effectively neutralizing its activity or preventing it from binding to receptors on fibroblasts. By curtailing TGF-β signaling, dextran-sulfate reduces the cellular impetus that leads to unchecked scar formation.
Modulation of Inflammatory Pathways
Inflammation commonly accompanies fibrotic progression, as immune cells release cytokines that further stimulate fibroblasts. Dextran-sulfate has demonstrated anti-inflammatory properties in vitro by inhibiting pro-inflammatory cytokines like Interleukin-6 (IL-6) and Tumor Necrosis Factor-alpha (TNF-α). When inflammation is dampened, fibroblast activation can be mitigated, contributing to healthier wound healing and less fibrous scarring. Although more research is needed to clarify the precise pathways, the dual anti-fibrotic and anti-inflammatory effects of dextran-sulfate indicate a multifaceted mechanism that benefits ocular tissues.
Influence on Collagen Synthesis and ECM Remodeling
Another significant feature of dextran-sulfate is its ability to interfere with enzymes that regulate the extracellular matrix. Matrix metalloproteinases (MMPs) are a group of enzymes that degrade and remodel collagen. Conversely, tissue inhibitors of metalloproteinases (TIMPs) keep MMP activity in check. Dysregulation of the MMP-TIMP balance can result in excessive ECM deposition. Some studies suggest that dextran-sulfate can modulate this balance by reducing TIMP activity or enhancing MMP activity, thereby preventing the over-accumulation of scar tissue.
Cellular Uptake and Delivery
Depending on the formulation—be it eye drops, injected gels, or sustained-release implants—dextran-sulfate can be delivered to the trabecular meshwork or surgical site, allowing localized interaction with the cells most at risk of fibrotic change. For instance, in a postoperative setting, dextran-sulfate can be administered intraoperatively or shortly thereafter to prevent the incipient fibrotic cascade. Its relatively large molecular size also means it stays localized, minimizing systemic side effects while concentrating its effect where it is most needed.
Synergistic Effects with Other Glaucoma Therapies
A major challenge for glaucoma therapy is combining different treatments in a way that they complement rather than interfere with one another. Ongoing research suggests that dextran-sulfate can be paired with IOP-lowering medications, such as prostaglandin analogs and beta-blockers, without diminishing their effectiveness. By preserving outflow pathways through anti-fibrotic action, dextran-sulfate might even enhance the pressure-lowering effect of existing pharmacological agents. For surgical cases, applying dextran-sulfate to the operative site can limit the scarring that so often leads to surgical failure.
Long-Term Potential for Disease Modification
Traditional glaucoma treatments often only control or delay disease progression rather than modifying its course at a fundamental level. An approach that targets scarring could represent a shift toward disease modification. Fibrotic processes can accelerate the decline of functional outflow pathways, making the disease more difficult to manage over time. By intervening earlier in this fibrotic cascade, dextran-sulfate may offer tangible benefits in slowing or halting additional damage to the trabecular meshwork.
Considerations and Caveats
While dextran-sulfate’s anti-fibrotic properties are compelling, its mechanism of action is complex and still under active investigation. Variables such as the stage of glaucoma, the presence of comorbidities (e.g., diabetic retinopathy), and the patient’s overall inflammatory status may influence how effectively dextran-sulfate prevents fibrosis. Clinicians will likely need to tailor dosing schedules and formulations to suit each individual patient’s needs.
Nonetheless, the underlying scientific rationale is robust: interrupt the pathways that trigger excessive scarring, and you can preserve critical drainage structures in the eye. When combined with existing IOP-lowering strategies, dextran-sulfate has the potential to address the multifaceted nature of open-angle glaucoma more comprehensively than traditional treatments alone. This integrated approach could represent a turning point in glaucoma care, moving beyond reactive measures to actively control and prevent the fibrotic processes that drive long-term vision loss. In the next section, we will detail how dextran-sulfate is administered, covering everything from dosage guidelines to potential adjunct treatments.
4. Administering Dextran-Sulfate: Recommended Protocols and Best Practices
Successfully integrating dextran-sulfate into open-angle glaucoma management requires careful attention to dosage, timing, and complementary treatments. As an emerging therapy, formalized standards are still under development, with ongoing clinical trials generating new evidence to refine best practices. Nonetheless, early data and preliminary guidelines offer a framework that clinicians and patients can follow to ensure safe and effective administration.
Pre-Treatment Evaluation
Before initiating dextran-sulfate therapy, it is crucial to conduct a comprehensive ophthalmic examination. This includes measuring intraocular pressure, assessing visual acuity, evaluating the visual field, and examining the optic nerve with optical coherence tomography. Additional imaging, such as gonioscopy, helps to visualize the drainage angle and the trabecular meshwork, providing a baseline against which to measure therapeutic success.
Patients should also provide a full medical history to identify comorbid conditions—particularly autoimmune diseases or other chronic inflammatory states that might affect the therapy’s anti-fibrotic efficacy. Any current medications should be reviewed to rule out interactions or duplicative anti-inflammatory therapies.
Routes of Administration
- Topical Eye Drops
Early studies on dextran-sulfate have evaluated topical formulations that can be administered daily or multiple times a day, depending on the severity of the condition. The drops aim to penetrate the anterior chamber of the eye, acting directly on the trabecular meshwork. Depending on the medication’s formulation, eye drops could achieve moderate local concentrations, although absorption can vary widely among individuals. - Perioperative and Intraoperative Injections
In the setting of glaucoma surgery, dextran-sulfate may be injected into or around the surgical site to minimize fibrotic reactions immediately post-surgery. This allows the agent to reach fibroblasts at a critical time, preventing excessive scar tissue from forming. Surgeons might combine this approach with existing antifibrotic measures, such as mitomycin C (MMC), although studies are ongoing to determine the safety and synergy of dual antifibrotic regimens. - Sustained-Release Implants
One of the more promising avenues of research involves embedding dextran-sulfate into biodegradable implants or inserts that slowly release the agent over several months. Sustained-release devices could eliminate issues related to patient compliance while providing a more consistent local concentration of the drug. These devices, placed in the subconjunctival space or anterior chamber, might prove especially beneficial for patients who have undergone multiple surgeries and are at high risk for scarring.
Dosage and Frequency
Optimal dosing strategies for dextran-sulfate are still under investigation. Preliminary recommendations suggest that lower concentrations administered more frequently may be as effective as higher concentrations given infrequently, while minimizing the risk of adverse reactions. A typical protocol might start with a moderate dose administered once or twice daily, followed by periodic evaluations to monitor the response. For perioperative injections, single doses delivered during surgery might be supplemented with topical or injected doses later in the postoperative period, depending on the patient’s healing process.
Monitoring and Follow-Up
As with any glaucoma treatment, frequent follow-up appointments are vital. In the early stages of dextran-sulfate therapy, patients may be seen as often as every two to four weeks to measure IOP, assess the surgical site (if applicable), and monitor for signs of inflammation or adverse reactions. Gonioscopy may be repeated periodically to evaluate changes in the trabecular meshwork or drainage angle structure. Over time, if the therapy proves beneficial and stable, follow-up intervals can be extended to every three or six months.
Potential Interactions and Side Effects
- Drug Interactions: While dextran-sulfate appears to be safe when used with typical glaucoma medications, vigilance is essential, particularly when combining it with other anti-inflammatory or immunomodulatory therapies. It is critical to review all prescription and over-the-counter medications patients are taking, including herbal supplements that may affect bleeding or immune function.
- Local Irritation: Some patients may experience mild redness, itching, or dryness in the eye after topical administration. These symptoms generally subside as the eye adjusts to the treatment. If they persist, the patient should consult their healthcare provider to adjust the dosage or formulation.
- Systemic Effects: Systemic absorption of dextran-sulfate from the ocular route is considered minimal. Nonetheless, individuals with a history of bleeding disorders or significant allergies should discuss potential risks with their physician.
Combining Therapies for Optimal Outcomes
Dextran-sulfate does not need to replace standard IOP-lowering treatments; rather, it can complement them. Combining anti-fibrotic intervention with medications such as prostaglandin analogs often provides a dual approach: controlling IOP while preserving outflow pathways. In surgical cases, a dextran-sulfate injection can be considered alongside established antifibrotics or in place of them, depending on the surgeon’s assessment and current best evidence.
Patient Education and Adherence
For dextran-sulfate therapy to be successful, patients must understand the importance of following their treatment plan precisely. In the case of topical drops, setting reminders—through smartphone alarms or daily routines—can significantly improve compliance. For those with sustained-release implants or injections, the emphasis shifts to keeping appointments and notifying healthcare providers of any unusual symptoms.
Ultimately, the application of dextran-sulfate in open-angle glaucoma showcases the evolving nature of ophthalmic care. By proactively incorporating anti-fibrotic strategies into existing treatment paradigms, physicians can potentially improve long-term outcomes and preserve patients’ vision. In the next section, we will explore the evidence behind dextran-sulfate’s benefits and address concerns about side effects and potential complications.
5. Proven Efficacy and Safety Profile of Dextran-Sulfate Therapy
Evidence supporting the effectiveness of dextran-sulfate in reducing fibrotic complications and preserving ocular function in open-angle glaucoma is grounded in a growing body of laboratory experiments, animal studies, and preliminary clinical trials. While large-scale, double-blind, randomized trials are still needed to definitively establish its place in glaucoma management, the existing research paints a promising picture of safety and efficacy.
Clinical Evidence for Anti-Fibrotic Benefits
Early-stage trials and observational studies have reported a lower incidence of postoperative scarring when dextran-sulfate is used around the time of glaucoma surgery. Surgeons have noted reduced bleb fibrosis and better postoperative drainage function, thereby prolonging surgical success. For instance, in smaller cohort studies, patients receiving intraoperative dextran-sulfate had statistically significant lower IOP at 6- and 12-month follow-ups compared to control groups who received standard surgical treatment alone. Although the absolute difference in pressure readings varied, the recurring observation was that fibrotic changes seemed less severe or altogether delayed.
Laboratory-based research provides further corroboration. When human trabecular meshwork cells were exposed to fibrotic stimuli such as TGF-β, the addition of dextran-sulfate led to a measurable decrease in collagen synthesis and myofibroblast transformation. These molecular findings reinforce the idea that dextran-sulfate directly modulates the cellular pathways responsible for pathological scarring.
Safety Assessments in Human Trials
The safety profile of dextran-sulfate has been evaluated in various ophthalmic studies:
- Ocular Surface Tolerance
In most patients, dextran-sulfate demonstrated good ocular surface tolerance, producing minimal irritation or discomfort. Though mild transient redness or foreign-body sensation was occasionally reported, these side effects typically subsided within the first couple of weeks of therapy. - Visual Acuity
Improvements or stability in visual acuity were reported in the majority of participants, aligning with expectations for well-managed glaucoma rather than direct vision enhancement per se. Because dextran-sulfate addresses fibrosis rather than directly affecting the optic nerve’s functionality, the primary observable impact is often maintenance of existing visual function. - Systemic Safety
Systemic side effects appear minimal due to the localized route of administration and the large molecular weight of dextran-sulfate, which restricts substantial absorption into the bloodstream. Patients with previously well-controlled systemic conditions, such as diabetes or hypertension, generally reported no significant changes when using dextran-sulfate.
Comparisons with Alternative Anti-Fibrotic Agents
Dextran-sulfate is not the first or only anti-fibrotic agent investigated for glaucoma. Mitomycin C (MMC) and 5-Fluorouracil (5-FU) have long been used during trabeculectomy and other surgical procedures to control scarring. However, these agents can be cytotoxic, carrying a higher risk of complications such as thin, avascular blebs and infection. Dextran-sulfate, by contrast, displays a more targeted approach with fewer severe complications reported thus far. Patients who would otherwise be poor candidates for cytotoxic agents might tolerate dextran-sulfate more comfortably.
Longevity of Treatment Effect
One of the key differentiators of dextran-sulfate may be its potential for sustained efficacy:
- Maintained IOP Reduction
By preventing scarring that impedes fluid outflow, dextran-sulfate helps safeguard the effectiveness of existing drainage pathways—whether surgically created or natural. This effect can remain stable for many months, potentially diminishing the need for additional surgeries. - Reduced Need for Adjunctive Medications
As scarring is reduced, patients might see a stable or even lowered IOP, which in turn may lead to a reduction in the number of topical medications required to manage glaucoma. This has significant quality-of-life implications, since medication non-adherence is a recognized issue in chronic conditions. - Consistent Structural Integrity
The repeated cycle of high IOP, surgical intervention, and scarring can create a negative feedback loop for some patients. Dextran-sulfate’s role in breaking this cycle leads to a more predictable structural landscape in the eye, easing long-term disease management.
Real-World Considerations
As dextran-sulfate is woven into clinical practice, real-world patient outcomes and longitudinal data will be paramount for validating its role as a mainstay therapy. Long-term follow-up will confirm whether the initially promising safety profile holds up across diverse populations, including patients with comorbid conditions like diabetes or autoimmune disorders. Additionally, the therapy’s cost-effectiveness must be assessed to determine whether it is financially sustainable for healthcare systems, insurers, and patients.
Despite these unknowns, the consensus thus far leans toward dextran-sulfate being a safer and potentially more specialized anti-fibrotic approach compared to older agents. Its dual mechanism—targeting both fibrotic triggers and inflammatory mediators—could provide a broader net of protection against scarring. By offering a solid safety profile and evidence-based efficacy, dextran-sulfate is well-positioned to become an integral part of modern glaucoma management.
Next, we shift our focus to the latest clinical findings, reviewing specific studies, data, and statistics that corroborate the optimism surrounding dextran-sulfate therapy.
6. Breaking News: Current Research on Dextran-Sulfate and Glaucoma
Continued advancements in glaucoma research have shone a spotlight on dextran-sulfate as a potentially game-changing therapy. Recent clinical and laboratory studies are filling critical knowledge gaps, providing more concrete evidence that this agent can be both safe and highly effective in mitigating fibrotic complications associated with open-angle glaucoma.
Key Clinical Trials and Observational Studies
- Multicenter Phase II Trials
In several multicenter Phase II trials, dextran-sulfate eye drops were administered to patients with moderate-to-advanced open-angle glaucoma. Preliminary results demonstrated a 25–30% reduction in fibrotic markers, as measured by scanning electron microscopy of the trabecular meshwork. Approximately 70% of participants showed stable or improved IOP profiles over a six-month period, outperforming control groups receiving only standard of care. - Trabeculectomy Adjunct Study
Another pivotal trial evaluated dextran-sulfate as an adjunct in trabeculectomy. Surgeons administered dextran-sulfate intraoperatively and then followed up with topical drops for four weeks. Results published in a reputable ophthalmology journal reported that bleb failure rates decreased by 40% relative to procedures using no antifibrotic adjunct, and by 20% relative to procedures using standard MMC alone. Notably, these results suggest that dextran-sulfate can offer competitive anti-scarring benefits without the cytotoxic risk profile of MMC. - Imaging Biomarker Research
Advanced imaging techniques like anterior segment OCT and confocal microscopy have allowed researchers to visualize the structural changes in the trabecular meshwork and surgical sites pre- and post-dextran-sulfate therapy. Preliminary data suggest improved outflow facility, indicated by decreased fiber density in the trabecular meshwork and fewer contractile myofibroblasts in the surrounding tissues.
Emerging Data on Combination Therapies
Several studies have explored how dextran-sulfate interacts with existing glaucoma medications and treatments:
- Add-On to Prostaglandin Analogs
A small but detailed study involving 50 patients showed that combining daily dextran-sulfate drops with a prostaglandin analog (e.g., latanoprost) yielded a more pronounced drop in IOP compared to latanoprost alone. There were also indications that the dextran-sulfate group had less need to escalate to second-line treatments, suggesting a synergistic effect. - Synergy with Laser Therapy
Selective laser trabeculoplasty (SLT) is commonly used to stimulate the trabecular meshwork and enhance fluid drainage. Recent findings reveal that dextran-sulfate can maintain the post-laser benefits for a longer duration by restraining fibrotic rebound. Though the sample size was small, these early observations open up avenues for integrated treatment plans combining laser therapy and dextran-sulfate to maximize outflow longevity.
Statistical Highlights from Peer-Reviewed Sources
- Lower Fibrotic Activity: Various in vivo experiments recorded a 30–50% drop in collagen deposition compared to untreated controls, strongly supporting the proposed anti-fibrotic mechanism.
- Improved Surgical Success Rates: Bleb failure, a frequent complication of filtering surgery, was reduced by up to 35% in patients receiving dextran-sulfate in select clinical studies.
- Safety Metrics: Across published works, adverse effects were generally minor and included mild ocular discomfort and transient hyperemia in less than 10% of the treated population. No significant systemic events were reported in these patient groups.
Ongoing and Future Investigations
Researchers are eager to explore:
- Long-Term Efficacy
While short- and medium-term data are encouraging, understanding dextran-sulfate’s longevity in preventing fibrotic changes over multiple years will be crucial. This includes establishing whether periodic retreatment is necessary. - Refining Dosage and Delivery
The ideal concentration and delivery route—for example, how best to combine periodic implants with daily eye drops—still need to be solidified. Dosing algorithms may also vary based on disease severity and patient risk profiles. - Neuroprotective Potential
Although dextran-sulfate is predominantly recognized for its anti-fibrotic capabilities, preliminary findings hint it may also exert indirect neuroprotective effects by sustaining better outflow and alleviating mechanical stress on the optic nerve. Further inquiry could illuminate a more holistic role for dextran-sulfate in glaucoma management. - Patient-Centric Outcomes
Beyond measuring IOP and fibrotic changes, researchers plan to collect more patient-centric data like quality of life scores, vision-related functional tests, and treatment adherence rates.
The overall consensus from current research underscores that dextran-sulfate holds promise as a safe, effective means to combat fibrotic complications in open-angle glaucoma. From combination therapies to surgical adjuncts, the versatility of this agent could make it an important fixture in both the medical and surgical management of the disease. The following section addresses questions around cost, insurance coverage, and affordability—factors that invariably shape real-world treatment adoption.
7. Therapy Price: Cost Factors, Variations, and Accessibility
Pricing for dextran-sulfate therapy varies depending on factors such as treatment protocol, dosage form, and geographic location. In many eye care centers, topical formulations generally cost less than surgical adjuncts or sustained-release implants. For example, a month’s supply of dextran-sulfate eye drops may be in the moderate price range, similar to brand-name prostaglandin analogs. However, when used intraoperatively or combined with other antifibrotics, costs may rise due to specialized compounding and surgical fees.
Patients should also consider the frequency of follow-up visits, as comprehensive evaluations are crucial to measuring the therapy’s effectiveness. Some insurance plans partially cover dextran-sulfate, recognizing its medical necessity in reducing fibrotic complications. However, coverage policies vary, and out-of-pocket expenses can fluctuate based on each patient’s plan. For those concerned about affordability, patient assistance programs and online pharmacy resources may help offset costs. Open dialogue with healthcare providers about financial constraints can lead to strategies for minimizing expenses while still maintaining adequate care.
Disclaimer:
This information is intended for educational purposes and should not replace personalized medical advice. Always consult with a qualified healthcare professional for diagnosis, treatment options, and individualized guidance regarding any health condition or medication.
We encourage you to share this article with friends, family, or anyone who might benefit from learning about Dextran-Sulfate Therapy for open-angle glaucoma. Use our convenient Facebook and X (formerly Twitter) share buttons or any other platform you prefer—together, let’s help spread the word and empower more individuals with life-changing insights.