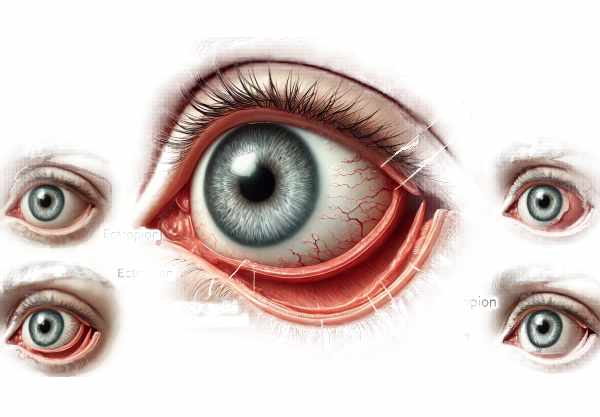
What is Ectropion?
Ectropion is an ocular condition in which the eyelid margin, usually the lower eyelid, turns outward and away from the eyeball. This condition can expose the inner eyelid surface and conjunctiva, resulting in dryness, irritation, and discomfort. Ectropion is more common in older adults due to natural weakness of the muscles and tissues surrounding the eyes, but it can also be caused by congenital defects, trauma, or previous surgeries. Understanding ectropion is critical for accurate diagnosis and treatment that prevent complications and maintains ocular health.
Ectropion insights
Pathology and Etiology
Ectropion is a condition in which the lower eyelid turns outward, away from the eye, exposing the inner surface of the eyelid and potentially causing various symptoms and complications. Ectropion’s underlying causes fall into several categories:
- Involutional (Age-Related) Ectropion: This is the most common type of ectropion, and it is typically seen in the elderly. As people age, the connective tissues and muscles that support their eyelids weaken. The lower eyelid relaxes and loses tone and elasticity, causing it to droop and turn outward. Furthermore, age-related skin changes such as loss of elasticity and collagen contribute to the development of ectropion.
- Cicatricial Ectropion: This type of ectropion is caused by scarring or contraction of the skin and underlying tissues near the eyelid. Scar tissue can pull the eyelid outward, causing ectropion. Cicatricial ectropion can be caused by trauma, burns, chemical injuries, previous surgeries, or chronic inflammatory conditions like blepharitis.
- Paralytic Etropion: Paralytic ectropion is caused by paralysis of the facial nerve (cranial nerve VII), which affects the muscles that move the eyelids. Bell’s palsy, tumors, and surgical damage to the facial nerve can all cause ectropion. Without proper muscle function, the lower eyelid cannot hold its normal position and turns outward.
- Mechanical Ectropion: Mechanical ectropion occurs when external factors physically pull the eyelid away from the eye. Tumors, cysts, or masses near the eyelid can exert pressure and cause it to evert. Prolonged use of certain eye drops or medications can also lead to mechanical ectropion.
- Congenital Ectropion: This rare type of ectropion occurs at birth and is frequently associated with other congenital abnormalities like Down syndrome or ichthyosis. Congenital ectropion can be caused by structural abnormalities in the eyelid or surrounding tissues.
Symptoms and Clinical Presentation
Ectropion symptoms vary according to the severity of the condition, but typically include:
- Excessive Tearing (Epiphora): One of the most distinguishing features of ectropion is excessive tearing. When the lower eyelid turns outward, the tear drainage system becomes disrupted, resulting in tears spilling over the eyelid and down the face.
- Dryness and Irritation: Exposing the inner eyelid surface and conjunctiva to air can result in dryness, irritation, and a gritty sensation. The affected eye may feel scratchy or uncomfortable, particularly in windy or dry conditions.
- Redness and Inflammation: The exposed conjunctiva and inner eyelid may turn red and inflamed. Chronic exposure and irritation can cause conjunctivitis or blepharitis, which exacerbates the discomfort.
- Light Sensitivity (Photophobia): When the conjunctiva is exposed and irritated, the eye becomes more sensitive to light, causing discomfort and squinting.
- Corneal Exposure and Damage: In severe cases of ectropion, the cornea can become exposed, resulting in drying, abrasion, or ulceration. This can cause significant pain, blurred vision, and a higher risk of infection.
Effects on Quality of Life
Ectropion has a significant impact on an individual’s quality of life. The constant tearing and wiping of the eyes can be both bothersome and embarrassing. Chronic eye irritation and discomfort can disrupt daily activities like reading, driving, and working. In severe cases, the condition can cause visual impairment due to corneal damage. Ectropion’s cosmetic appearance, which includes the lower eyelid drooping and turning outward, can have an impact on a person’s self-esteem and confidence.
Risk Factors
Several factors raise the risk of developing ectropion.
- Age: The most important risk factor for ectropion is age. As people age, the connective tissues and muscles around their eyes weaken, increasing the risk of developing ectropion.
- Previous Eyelid Surgery: Those who have had eyelid surgery, such as blepharoplasty, are more likely to develop ectropion. Surgical procedures may alter the normal anatomy and support structures of the eyelids.
- Facial Nerve Paralysis: Bell’s palsy and tumors are two conditions that can cause paralytic ectropion.
- Chronic Inflammation: Chronic inflammatory conditions of the eyelids, such as blepharitis or allergic conjunctivitis, can increase the likelihood of developing cicatricial ectropion.
- Trauma or Injury: Trauma or injury to the eyelid or surrounding tissues can cause scarring and cicatricial ectropion.
- Genetic Conditions: Congenital ectropion is linked to genetic conditions like Down syndrome and ichthyosis.
Complications
Ectropion, if left untreated, can cause a number of complications, including
- Chronic Conjunctivitis: Prolonged exposure and irritation of the conjunctiva can lead to chronic inflammation and conjunctivitis, which causes redness, discharge, and discomfort.
- Corneal Ulceration: Severe ectropion can expose the cornea, resulting in drying, abrasion, and ulceration. Corneal ulcers are painful and can lead to significant vision loss if not treated quickly.
- Infection: The exposed conjunctiva and cornea are more vulnerable to bacterial infections, which can exacerbate the condition.
- Vision Loss: In severe cases, untreated ectropion can lead to permanent vision loss due to corneal damage and scarring.
Prognosis
The prognosis for people with ectropion is determined by the underlying cause and severity of the condition. Ectropion can often be successfully treated, resulting in significant improvements in symptoms and quality of life. Early detection and intervention are critical for preventing complications and maintaining ocular health.
Diagnostic methods
Ectropion is diagnosed using a combination of clinical evaluations and imaging techniques to determine the condition’s severity and underlying causes. Early and accurate diagnosis is critical for preventing complications and determining the best treatment plan.
- Visual Acuity Test: This basic test measures vision sharpness to determine whether ectropion is affecting visual acuity. Patients read letters from a standard eye chart at a set distance.
- External Examination: The ophthalmologist thoroughly examines the eyelids and the surrounding facial structures. This includes looking for any visible signs of inflammation, scarring, or abnormal eyelid positioning.
- Slit Lamp Examination: A slit-lamp microscope is used to examine the eyelids, conjunctiva, and cornea in great detail. This aids in detecting any secondary complications, such as conjunctivitis, corneal exposure, or ulcers.
- Eyelid Eversion Test: The doctor gently pulls the lower eyelid down to evaluate its tone and elasticity. The degree of eversion and the condition of the exposed conjunctiva are documented.
- Tear Film Break-Up Time (TBUT): This test measures the stability of the tear film. A fluorescein dye is applied to the patient’s eye, and they are instructed to blink. The time it takes for dry spots to appear on the cornea is measured to determine tear film stability.
- Schirmer’s Test: This test evaluates tear production. Strips of filter paper are placed beneath the lower eyelids, and the amount of moisture absorbed over a few minutes is recorded.
Innovative Diagnostic Techniques
- Digital Imaging and Photography: High-resolution imaging systems can provide detailed images of the eyelids and ocular surface. These images can be used to establish baseline documentation and track changes over time.
- Ocular Surface Staining: Fluorescein, rose bengal, and lissamine green are used to stain the ocular surface. These dyes aid in the detection of dryness, damage, or inflammation on the conjunctiva and cornea.
- Tear Osmolarity Testing: This test determines the concentration of solutes in the tear film. High tear osmolarity indicates tear film instability, which can aid in the diagnosis of dry eye caused by ectropion.
- Dynamic Imaging: Techniques like high-speed video imaging can record blink dynamics and eyelid movements in real-time. This aids in determining the functional aspects of the eyelids and detecting any anomalies.
Comprehensive Evaluation
A comprehensive evaluation that incorporates both standard and novel diagnostic techniques allows for a thorough understanding of ectropion and its impact on the ocular surface. This thorough evaluation is essential for developing an effective treatment plan tailored to each patient’s specific needs.
Treatment
Treating ectropion entails addressing the underlying cause, relieving symptoms, and avoiding complications. The severity of the condition determines the treatment options, which range from conservative management to surgical intervention.
Standard Treatment Options
- Lubricating Eye Drops and Ointments: Artificial tears and lubricating ointments moisturize the eye, reducing dryness and irritation. These are frequently the first line of treatment for mild cases of ectropion.
- Warm Compresses: Applying warm compresses to the affected eyelid can help relieve irritation and promote drainage of any blocked tear ducts.
- Eyelid Taping: Taping the lower eyelid upwards can provide temporary relief by allowing the eyelid to rest more naturally against the eye.
- Moisture Shields: Wearing a moisture shield, especially while sleeping, can help retain moisture and protect the exposed ocular surface.
- Topical Steroids: In cases of inflammation, topical steroids may be used to reduce swelling and irritation in the eyelids and conjunctiva.
Surgical Treatment Alternatives
- Eyelid Tightening (Lateral Tarsal Strip Surgery): This procedure tightens the lower eyelid by shortening and securing the lateral canthal tendon. It is widely used to treat involutional ectropion.
- Eyelid Reconstruction: In cases of cicatricial ectropion caused by scarring, reconstructive surgery may be required. This may entail skin grafts or flaps to release scar tissue and restore normal eyelid function.
- Medial Canthoplasty: This surgical technique involves tightening the medial canthal tendon, which can help reposition the eyelid closer to the eye.
- Orbicularis Muscle Repair: Repairing or repositioning the orbicularis oculi muscle can help with paralytic ectropion and improve eyelid closure and function.
Innovative and Emerging Therapies
- Minimally Invasive Procedures: Advances in surgical techniques have resulted in the creation of minimally invasive procedures that shorten recovery time and improve cosmetic outcomes. These include laser treatments and radiofrequency tightening.
- Biologic Agents: Research is being conducted into the use of biologic agents that target specific inflammatory pathways. These medications can help manage chronic inflammation caused by cicatricial ectropion.
- Stem Cell Therapy: Experimental treatments using stem cells aim to regenerate damaged tissues and improve eyelid function. This emerging field shows promise for future treatment options.
- Gene Therapy: While still in the experimental stage, gene therapy has the potential to address the underlying genetic causes of congenital ectropion and provide long-term solutions.
Supportive Treatments
- Regular Monitoring: Regular follow-up visits with an ophthalmologist are required to monitor the condition and adjust treatment plans as necessary.
- Patient Education: Educating patients about their condition and the importance of following treatment plans can improve outcomes and reduce complications.
- Lifestyle Changes: Reminding patients to protect their eyes from environmental irritants like wind and dust, as well as to avoid rubbing their eyes, can help manage symptoms.
Trusted Resources
Books
- “Oculoplastic Surgery: The Essentials” by William P. Chen
- “Eyelid and Periorbital Surgery” by Mark A. Codner and Clinton D. McCord Jr.
- “Principles and Practice of Ophthalmic Plastic and Reconstructive Surgery” by Stephen L. Bosniak






