A New Frontier in Restoring Corneal Clarity
Fuchs’ endothelial corneal dystrophy (FECD) is a progressive eye disease that affects the innermost layer of the cornea, the endothelium. Over time, patients may experience blurred vision, glare, or even debilitating sight impairment due to endothelial cell loss and excess fluid buildup in the cornea. Historically, corneal transplantation has been the standard solution once significant vision decline occurs. However, an innovative procedure known as Endothelial Cell Injection Therapy is transforming the landscape of FECD treatment. By harnessing the ability to culture and transplant healthy endothelial cells directly, this minimally invasive approach promises to restore corneal transparency without necessitating a full-thickness or partial-thickness corneal graft.
This advanced cell-based therapy is significant for a number of reasons. Firstly, it eliminates many of the complications associated with traditional corneal transplantation, such as graft rejection or slow recovery periods. Secondly, it paves the way for broader access to donor tissue, since a smaller number of donor corneas can potentially treat many more patients. Lastly, because the procedure requires only a minimal incision and introduces healthy cells into the diseased cornea, the post-operative healing period can be more comfortable and potentially faster.
Below, we delve into how this novel therapy works, unravel key details of its protocols and applications, explore the research that supports its efficacy and safety profile, and discuss cost considerations. Whether you have just been diagnosed with Fuchs’ corneal dystrophy or you are a medical professional seeking comprehensive insights, this article lays out the fundamentals of Endothelial Cell Injection Therapy, offering an in-depth look at its potential to revolutionize corneal care.
Transforming Corneal Care: How Does Endothelial Cell Injection Therapy Work?
Restoring vision in Fuchs’ endothelial corneal dystrophy revolves around one essential task: replenishing or revitalizing the corneal endothelium. The endothelium’s job is to regulate fluid levels within the cornea, ensuring the tissue remains transparent and healthy. However, in FECD, these cells gradually deteriorate, leading to fluid accumulation (edema) and eventual clouding of vision. Enter Endothelial Cell Injection Therapy—an approach that replaces these ailing cells with lab-cultured healthy ones.
Cultivating Healthy Corneal Endothelial Cells
One of the most remarkable aspects of this therapy is the ability to cultivate endothelial cells outside the body. Historically, corneal endothelial cells were believed to be non-regenerative, meaning that if significant cell loss occurred, vision could only be repaired via transplantation. Advances in cell biology have since demonstrated that, under certain lab conditions, human endothelial cells can indeed be grown and multiplied. Key steps include:
- Donor Tissue Harvest: A small segment of healthy corneal endothelium is obtained from an eligible donor cornea. Unlike full donor corneas for traditional transplants, this sample can be far smaller, reducing the demand for high-quality graft tissue.
- Enzymatic or Mechanical Isolation: Lab technicians separate the endothelium from other corneal layers, ensuring only the endothelial cell population is harvested.
- Expansion in Culture: The extracted cells are placed in specialized media containing growth factors, nutrients, and other supportive conditions. Under these controlled settings, the cells proliferate, forming colonies that expand until there are enough viable cells to treat multiple patients.
Minimally Invasive Injection Procedure
Once sufficient cells have been generated, these can be delivered to a patient’s diseased cornea via a minimally invasive technique:
- Preparation of the Cornea: The surgeon may perform a very small incision in the peripheral cornea. In some protocols, any severely compromised Descemet membrane (the basement layer for the endothelium) is gently peeled or debulked to create an optimal surface for the injected cells.
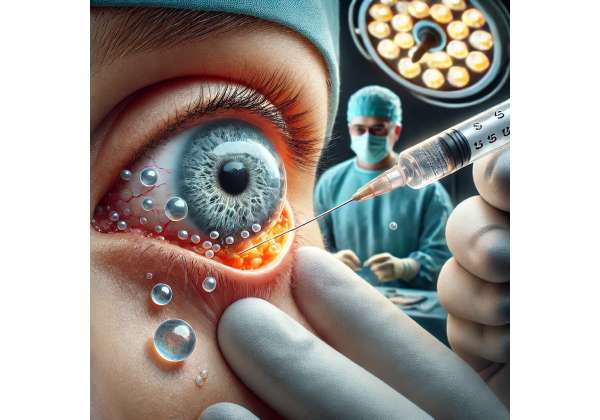
- Injection of Cell Suspension: The lab-cultured endothelial cells, often suspended in a solution containing vital nutrients, are carefully injected into the anterior chamber. This injection typically involves a micro-needle or cannula.
- Positioning and Attachment: The patient is placed in a specific posture—often face-up—so that gravity helps distribute the cells across the inner surface of the cornea. In some methods, an air or gas bubble is injected to gently press these cells against the posterior corneal surface.
- Postoperative Considerations: Patients are commonly asked to maintain a face-up position for several hours to ensure the cells attach properly. Afterward, normal activities can resume gradually, with monitoring for any signs of elevated intraocular pressure or fluid imbalance.
Advantages Over Conventional Transplantation
- Reduced Risk of Rejection: Since the therapy introduces only endothelial cells, rather than a full-thickness corneal graft, the body is less likely to mount a robust immune response.
- Smaller Tissue Demand: A single donor cornea can yield enough cells for multiple patients. This approach helps address donor shortages worldwide.
- Less Surgical Trauma: Traditional endothelial keratoplasty (e.g., DMEK, Descemet Membrane Endothelial Keratoplasty) still requires partial insertion of donor tissue. Endothelial Cell Injection Therapy only needs a small needle or cannula insertion, making it potentially more comfortable and more efficient in both operating room time and recovery.
By focusing on the underlying cellular deficit—defective corneal endothelium—this method directly addresses the root cause of Fuchs’ corneal dystrophy. As research in cell biology expands, it is likely that the refining of culture techniques, improved injection systems, and safer postoperative regimens will further enhance both the success rate and accessibility of this promising therapy.
From Lab to Eye: Protocols and Practical Applications of Endothelial Cell Injection
Implementing Endothelial Cell Injection Therapy requires a multidisciplinary collaboration, merging the expertise of corneal surgeons, cell biologists, and specialized lab technicians. The objective is a smooth transition of healthy cells from a Petri dish to a patient’s diseased cornea—ensuring robust cell survival and integration. To accomplish this, clinicians follow a structured series of steps, each vital for a successful outcome.
Screening and Patient Selection
- Confirming the Diagnosis: A thorough ophthalmic exam using slit-lamp biomicroscopy, specular microscopy, and optical coherence tomography (OCT) verifies FECD severity. Specular microscopy helps gauge endothelial cell density and morphological changes characteristic of FECD.
- Medical History Review: Since this therapy involves potentially fragile cultured cells, complicating factors like uncontrolled glaucoma, severe ocular surface disease, or advanced macular pathology might reduce the likelihood of success.
- Detailed Corneal Topography: To ensure that the patient’s cornea doesn’t have concomitant issues (e.g., keratoconus), a precise topographic analysis is often performed.
- Patient Counseling: The surgical team discusses the experimental or cutting-edge status of the procedure, the expected outcomes, the necessity for follow-up visits, and the possible requirement for further interventions if cell repopulation is suboptimal.
Preoperative Preparation
- Medication Optimization: Patients may be advised to discontinue certain glaucoma medications or undertake prophylactic antibiotic eye drops to reduce infection risk.
- Systemic Health Assessment: A brief evaluation of cardiovascular stability and relevant systemic conditions ensures the patient can safely undergo sedation or local anesthesia.
- Donor Cell Quality Control: The cultured cells, tested for viability and free of contamination, must meet strict release criteria before being declared ready for injection. Some laboratories examine the cell culture for morphological uniformity and consistent expression of endothelial markers.
Intraoperative Techniques
During the actual procedure, surgeons frequently employ one of two main techniques for injecting cells:
- Aqueous Suspension Injection: The majority of protocols use a fluid suspension of endothelial cells. After creating a small incision in the cornea’s periphery, a micro-catheter or cannula is inserted into the anterior chamber. The fluid containing endothelial cells is gently released, often accompanied by low volumes of balanced salt solution or specialized mediums that promote cell viability.
- Gel Matrix Support: Some research proposes suspending cells within a gentle gel matrix or hydrogel. This concept aims to protect the cells from shear forces during injection and maintain localized distribution against the cornea.
Surgeons are careful to maintain stable intraocular pressures, employing fine control over infusion and aspiration if any fluid exchange is necessary. The presence of a cohesive viscoelastic solution is sometimes used to preserve the shape of the anterior chamber and reduce unintentional cell loss.
Postoperative Support and Follow-Up
- Positioning: Similar to DMEK, patients are often instructed to lie on their backs for a period so gravity can help the new cells adhere to the posterior corneal surface.
- Medications: Topical antibiotics, corticosteroids, and nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to lessen inflammation and minimize infection risk.
- IOP Checks: Certain injection protocols incorporate an air or gas bubble to press cells into place. A watchful eye on intraocular pressure is crucial, as gas expansion can spike IOP if left unchecked.
- Cell Survival Monitoring: Regular specular microscopy or confocal imaging over the weeks to months following the procedure helps document endothelial cell density and distribution. Real success is indicated by stable or improved visual acuity and the resolution of corneal edema.
Emerging Protocol Variations
As clinical trials expand, variations in technique continue to emerge:
- Refinement of Culture Media: Different labs experiment with growth factors or co-culture systems to enhance cell proliferation and resilience.
- Biocompatible Carriers: Polymers or scaffolds that preserve cell orientation might be integrated to reduce migration or clumping during the injection process.
- Automated Delivery Systems: Efforts are underway to automate cell injection to boost reproducibility and minimize surgeon variability.
Putting it all together, the success of Endothelial Cell Injection Therapy hinges on tightly controlled steps—from initial cell harvest to postoperative care. Patients undergoing this therapy can benefit from a gentler procedure that targets only the diseased layer, bypassing many risks associated with full corneal transplants. As techniques mature, an ever-growing portion of those with Fuchs’ corneal dystrophy can look forward to a treatment that not only restores vision but also spares precious donor resources.
Insight from the Lab: Latest Research and Clinical Investigations
Endothelial Cell Injection Therapy stands at the crossroads of regenerative medicine, cell-based therapeutics, and innovative surgical technique. Over the last decade, the field has witnessed leaps in both preclinical and clinical studies as investigators strive to refine protocols, boost cell survival, and ensure stable long-term outcomes.
Preclinical Models and Proof-of-Concept
Animal studies have played a pivotal role in validating the feasibility of injecting lab-grown endothelial cells into diseased corneas. Researchers using primate or rabbit models consistently report:
- Successful Endothelial Regeneration: After a standardized injury to the corneal endothelium, injected cells integrated into the posterior cornea, restored transparency, and improved corneal thickness.
- Low Rejection Rates: Animals demonstrated minimal immune response, likely because the transplanted cell population was relatively small and localized compared to a full donor graft.
- Importance of Donor Cell Quality: Across studies, the viability and consistency of the cultured cells correlated strongly with visual improvements.
These foundational results paved the way for human trials, giving surgeons the confidence to transition from bench to bedside.
Early Clinical Trials in Humans
While large-scale randomized controlled trials are still developing, initial clinical findings are encouraging:
- Phase I/II Trials: Various research teams in Asia and Europe have published results demonstrating that Endothelial Cell Injection Therapy can lead to measurable improvements in central corneal thickness, reduced edema, and better visual acuity. Follow-ups ranging from six months to three years indicate a majority of patients maintain stable or enhanced endothelial cell density compared to baseline.
- Safety Markers: Adverse events such as significant inflammation or rejection episodes remain low. A small percentage of patients experience IOP spikes or partial cell detachment that require additional interventions, but these episodes are relatively rare.
- Visual Recovery Timeline: Many patients notice initial improvements in clarity within weeks, with further enhancements over subsequent months as the endothelial monolayer fully stabilizes and matures. This trajectory often surpasses the healing timeframe for standard corneal graft surgeries, which can stretch many months or longer for vision to fully stabilize.
Comparative Effectiveness Research
Though Endothelial Cell Injection Therapy is not yet as widespread as DMEK or DSAEK (Descemet Stripping Automated Endothelial Keratoplasty), studies contrasting these approaches are emerging:
- Graft-Free Advantage: Traditional keratoplasty procedures carry a known risk of graft rejection or partial detachment, whereas cell injection omits the presence of foreign tissue sheets or flaps.
- Faster Rehabilitation: Preliminary data suggest that because the procedure is less invasive, patients might require fewer follow-up visits, experience less medication load, and resume normal activities quicker.
- Long-Term Stability: The question of cell longevity remains a subject of ongoing trials. Some experts hypothesize that if transplanted cells properly integrate and self-renew to some degree, Endothelial Cell Injection Therapy could offer stable clarity for many years, possibly comparable to the best endothelial keratoplasty outcomes.
Exploring New Frontiers
Innovations on the research horizon promise even greater possibilities:
- Gene Editing Approaches: Techniques like CRISPR/Cas9 may be used to correct genetic mutations in donor or patient cells before injection, opening avenues for a personalized therapy free of hereditary flaws.
- Stem Cell Sources: Instead of relying on cadaveric donor tissue, some teams are investigating embryonic or induced pluripotent stem cells (iPSCs) to generate corneal endothelial cells. This approach could potentially sidestep donor limitations altogether.
- Scaffold-Free Cultures: Fully standardized protocols that allow consistent mass production of endothelial cells without requiring specialized scaffolds or supports are under development. Achieving uniform, high-density cultures at scale will be instrumental in meeting global demand.
Collectively, these lines of inquiry underscore the momentum behind Endothelial Cell Injection Therapy. While further research is essential—particularly larger trials with extended follow-ups—current evidence consistently points to a high safety profile, meaningful visual gains, and an enhanced quality of life for patients with Fuchs’ corneal dystrophy.
Regenerative Potential: Evaluating Efficacy and Safety of Endothelial Cell Injection
Every medical breakthrough demands thorough validation of its risk-benefit balance. Endothelial Cell Injection Therapy is no exception, especially given that the cornea is the eye’s main refractive surface, crucial for clear vision. The technique’s success boils down to two main yardsticks: how effectively it improves corneal function and how safely it can be administered in a real-world patient population.
Markers of Clinical Success
- Improved Visual Acuity: Ultimately, any corneal procedure’s success hinges on restoring or enhancing visual clarity. Many patients with Fuchs’ corneal dystrophy suffer from morning blur, halos, and glare that hamper daily life. Post-injection, a significant segment of patients report less corneal haze, sharper focus, and a reduction in light sensitivity.
- Sustained Endothelial Cell Density: Specular microscopy or in vivo confocal imaging offers quantitative proof that transplanted cells are surviving and forming a functional monolayer. A notable rise or stabilization in endothelial cell count—coupled with lower corneal thickness—stands as a reliable indicator of therapy success.
- Corneal Thickness and Clarity: Swelling in FECD leads to an increase in pachymetry readings (the thickness of the cornea). After injection therapy, a gradual decline in thickness strongly correlates with improved function of the newly grafted cells.
Short-Term and Long-Term Safety Considerations
- Immunologic Tolerance: Because this approach involves only cells (rather than a large swath of donor tissue), the risk of a robust immune rejection is deemed lower. However, mild rejection episodes are still possible, necessitating vigilance and steroid coverage.
- Infectious Risks: Any surgical manipulation of the anterior chamber opens the door to a small but non-negligible infection risk. Strict aseptic protocols and prophylactic antibiotics are crucial to mitigate endophthalmitis or keratitis.
- Intraocular Pressure Fluctuations: Some protocols include an intracameral gas bubble to press the cells into place. If this bubble expands or is miscalculated, IOP can spike, jeopardizing the optic nerve. Postoperative IOP checks and appropriate interventions (needle decompression or medication) often circumvent lasting damage.
- Inflammation Control: Corticosteroid eye drops or other immunomodulatory agents typically keep inflammation in check. Should patients develop uveitis or other inflammatory complications, prompt treatment reduces the likelihood of permanent corneal scarring.
- Potential Repeat Procedures: A subset of patients might not achieve the desired effect after a single injection due to insufficient cell adherence or suboptimal cell survival. Follow-up injections or switching to a more traditional keratoplasty can be fallback options.
Patient Profiles with High Benefit Potential
Endothelial Cell Injection Therapy can be particularly advantageous for:
- Early-Stage FECD Patients: Those not yet severely debilitated might enjoy quick vision restoration without the rigors of a transplant.
- Individuals with Moderate Corneal Changes: The therapy might preempt more advanced disease progression, potentially halting or reversing endothelial decline.
- Patients with Coexisting Ocular Issues: Because the procedure is minimally invasive, it may fit well into the overall ophthalmic management of individuals who also have mild cataracts or stable glaucoma.
- Those Seeking Low-Risk Alternatives: Not every patient is comfortable with the idea of a full or partial corneal graft. Minimally invasive cell injection might better align with personal or medical preferences.
Real-World Validation
Despite encouraging data, real-world clinical success also hinges on a robust infrastructure: experienced lab technicians for cell culture, highly trained surgeons adept in microinjection, and reliable postoperative care. Early adopters and specialized centers already report high patient satisfaction scores, citing quicker return to daily tasks, minimal complications, and good synergy with other corneal procedures.
Because the technique is evolving, prospective patients should engage in detailed discussions with their corneal specialists, balancing potential gains against still-emerging knowledge. While Endothelial Cell Injection Therapy is not yet considered an across-the-board replacement for DMEK or full-thickness keratoplasty, its compelling clinical profile suggests it could soon become a mainstream solution—particularly as labs become more adept at mass-producing endothelial cells and surgical protocols become standardized worldwide.
Therapy Price: Exploring Costs for Endothelial Cell Injection
Costs for Endothelial Cell Injection Therapy vary by country, clinic, and whether the procedure is still classified as experimental. Fees often reflect cell culture expenses, lab overhead, surgeon expertise, and specialized surgical equipment. Although some centers charge between \$4,000 and \$8,000 per eye, these figures can fluctuate widely depending on facility tiers and insurance agreements. Certain insurance plans may partially cover the procedure if deemed medically necessary, but eligibility varies. Financing options like monthly payment plans or medical loans might be available, offering greater access to those facing higher out-of-pocket costs.
Disclaimer: This article is for informational purposes only and does not substitute professional medical advice, diagnosis, or treatment. Always consult a qualified ophthalmologist or healthcare provider for personalized recommendations regarding Fuchs’ corneal dystrophy or any other eye health concerns.
We encourage you to share this article with friends, family, or online communities interested in Fuchs’ corneal dystrophy and cutting-edge corneal treatments. Use our Facebook and X (formerly Twitter) share buttons, or spread the word through your preferred social platforms. Every share helps raise awareness and brings us one step closer to better eye health for all.