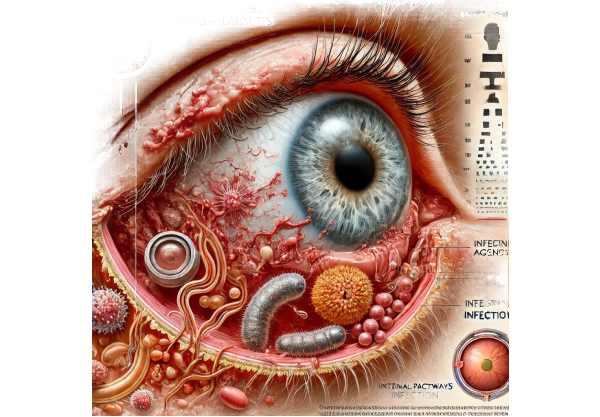
What is Infectious Endophthalmitis?
Infectious endophthalmitis is a severe, vision-threatening inflammation of the inside of the eye that is usually caused by infection. This condition can develop after eye surgery, penetrating ocular trauma, or systemic infections that spread to the eye. It affects both the vitreous and aqueous humors and can quickly lead to blindness if not diagnosed and treated right away. Severe eye pain, redness, decreased vision, and swelling are some of the symptoms. Understanding and early detection of infectious endophthalmitis are critical for maintaining vision and avoiding further complications.
Infectious Endophthalmitis: Detailed Insights
Infectious endophthalmitis is a medical emergency that causes inflammation in the eye due to a bacterial or fungal infection. This condition poses serious vision risks and, if left untreated, can lead to irreversible blindness. Infectious endophthalmitis has three causes: postoperative, post-traumatic, and endogenous.
Etiology and Risk Factors
- Postoperative Endophthalmitis: This is the most common type of endophthalmitis and develops following intraocular surgeries such as cataract extraction, vitrectomy, and other invasive procedures. The incidence varies according to the type of surgery and aseptic techniques used. Risk factors include inadequate sterilization of surgical instruments.
- A contaminated surgical environment.
- Prolonged surgery time.
- Patient characteristics such as diabetes, immunosuppression, and pre-existing ocular surface diseases.
- Post-Traumatic Endophthalmitis: This type develops after penetrating injuries to the eye, allowing external pathogens to enter. Risk factors include the nature and severity of the injury.
- Delay in seeking medical treatment.
- Contaminated foreign bodies inside the eye.
- Endogenous Endophthalmitis: This is a condition in which pathogens from a distant infection site spread hematogenously to the eye. Endocarditis, urinary tract infections, and systemic fungal infections are some common causes. Risk factors include an immunocompromised state.
- The use of intravenous drugs.
- Existence of indwelling catheters.
Pathogenesis
Infectious endophthalmitis pathogenesis involves pathogen invasion and proliferation within intraocular structures, resulting in a severe inflammatory response. The vitreous humor’s gel-like consistency makes it an ideal medium for microorganism growth. When an infection is established, inflammatory cells and cytokines are recruited to the site, resulting in:
- Vitreous Opacification: Inflammatory cells and pathogens cause the vitreous humor to become cloudy, significantly impairing vision.
- Retinal Damage: The inflammation may spread to the retina, resulting in retinal necrosis and detachment.
- Optic Nerve Involvement: The optic nerve may become inflamed (optic neuritis), resulting in permanent vision loss.
Clinical Presentation
Patients with infectious endophthalmitis typically present with a rapid onset of symptoms, such as:
- Severe Eye Pain: Typically described as deep and throbbing.
- Redness and Swelling: The eye appears red due to conjunctival injection and chemosis.
- Visual Disturbances: Sudden vision loss or blurring.
- Photophobia: Inflammation-induced light sensitivity.
- Hypopyon: An accumulation of inflammatory cells in the anterior chamber that appears as a white or yellow layer.
Microbiology
The microbiological profile of infectious endophthalmitis changes depending on the source of infection:
- Bacterial Pathogens: The most common bacterial causes are Staphylococcus epidermidis, Staphylococcus aureus, Streptococcus species, and Gram-negative bacilli such as Pseudomonas aeruginosa.
- Fungal Pathogens: Candida and Aspergillus species are the most common fungal pathogens in endogenous endophthalmitis, especially in immunocompromised individuals.
Complications
If not treated promptly, infectious endophthalmitis can cause a variety of complications.
- Retinal Detachment: The inflammatory response can exert tractional forces on the retina, resulting in detachment.
- Phthisis Bulbi: A shrunken, non-functioning eye caused by severe, uncontrolled inflammation.
- Secondary Glaucoma: Elevated intraocular pressure caused by inflammatory debris clogging the trabecular meshwork.
- Optic Atrophy: Permanent damage to the optic nerve, which causes blindness.
Prognosis
The prognosis of infectious endophthalmitis is determined by several factors, including the causative organism, the speed of diagnosis and treatment, and the patient’s overall health. Gram-negative infections and fungal endophthalmitis have a poorer prognosis than Gram-positive infections. Prompt and aggressive treatment is critical for maintaining vision and achieving a positive outcome.
Methods for Diagnosing Infectious Endophthalmitis
To confirm the presence of infection and determine the causative pathogen, infectious endophthalmitis requires a combination of clinical evaluation, microbiological testing, and imaging studies. Here are the main diagnostic methods used:
Clinical Evaluation
A thorough clinical examination by an ophthalmologist is required. This includes a Visual Acuity Test to assess the level of vision loss.
- Slit-Lamp Examination: A thorough examination of the anterior segment of the eye for signs of inflammation, such as conjunctival injection, corneal edema, and hypopyon.
- Indirect Ophthalmoscopy: Examines the vitreous and retina for signs of infection, such as opacities and lesions.
Microbiological Testing
Microbiological testing is critical for determining the causative pathogen and guiding appropriate antimicrobial therapy. This involves:
- Vitrectomy and Vitreous Tap: A sample of vitreous humor is obtained through vitrectomy or vitreous tap for microbiological analysis. This sample is cultured to detect bacterial or fungal pathogens.
- Anterior Chamber Paracentesis: Aqueous humor is collected from the anterior chamber and sent for culture and sensitivity testing.
- Gram Stain and Culture: A direct microscopic examination with Gram stain can provide immediate information about the type of organism. The results of the culture help identify the pathogen and its antibiotic susceptibility.
Imaging Studies
Imaging studies are used to determine the extent of intraocular inflammation and rule out other possible causes of symptoms.
- Ultrasound B-Scan: When media opacity obscures the fundus, an ultrasound B-scan can detect vitreous opacities, retinal detachment, and other intraocular abnormalities.
- Optical Coherence Tomography (OCT): OCT uses high-resolution images of the retina to detect macular edema, retinal detachment, and other structural changes.
Additional Lab Tests
Endogenous endophthalmitis may necessitate additional laboratory tests to determine the primary source of infection:
- Blood Cultures: To identify systemic bacteremia or fungemia.
- Urine Cultures: To diagnose urinary tract infections that may have spread to the eye.
- Echocardiography: To rule out infectious endocarditis as the cause of endogenous endophthalmitis.
Infectious Endophthalmitis Treatment Options
Infectious endophthalmitis is a medical emergency that requires immediate and aggressive treatment to avoid permanent vision loss. The primary goals of treatment are to eliminate the infection, reduce inflammation, and maintain as much visual function as possible. Here are the standard treatment options, as well as some novel and emerging therapies:
Standard Treatment Options
- Intravitreal Antibiotics: The use of intravitreal antibiotics is essential for treating infectious endophthalmitis. These antibiotics are injected directly into the vitreous cavity, resulting in high local concentrations and rapid infection control. Common antibiotics include vancomycin, which is effective against Gram-positive bacteria, including methicillin-resistant Staphylococcus aureus (MRSA).
- Ceftazidime or Amikacin is effective against Gram-negative bacteria.
- Systemic Antibiotics: In addition to intravitreal antibiotics, systemic antibiotics are frequently used to provide more comprehensive coverage and treat any potential systemic source of infection. Microbiological testing results guide the selection of systemic antibiotics, which may include
- Fluoroquinolones include moxifloxacin and ciprofloxacin.
- Cephalosporins, including ceftriaxone.
- Topical and Periocular Antibiotics: In addition to intravitreal and systemic therapy, topical antibiotics (e.g., fortified vancomycin and tobramycin) and subconjunctival injections can be used to reduce external microbial load.
- Corticosteroids: Corticosteroids can be administered intravitreally, periocularly, or systemically to reduce inflammation and tissue damage. However, their use is controversial and usually avoided until the infection is under control due to the risk of suppressing the immune response.
- Vitrectomy: In severe cases, surgical intervention may be required, such as pars plana vitrectomy (PPV). Vitrectomy is the removal of infected vitreous gel and any intraocular debris, which aids in the clearance of the infection, reduction of the inflammatory load, and improved antibiotic penetration. Indications for vitrectomy include severe or rapidly worsening endophthalmitis.
- A poor initial response to intravitreal antibiotics.
- Evidence of significant vitreous opacities or retinal detachment.
Innovative and Emerging Therapies
- Antimicrobial Peptides: Antimicrobial peptides, which have broad-spectrum activity against bacteria and fungi, are currently under investigation. These peptides may offer an alternative to traditional antibiotics, particularly in cases of antibiotic resistance.
- Nanotechnology: The use of nanotechnology in drug delivery systems is being investigated to improve antibiotic efficacy and bioavailability. Nanoparticles can be engineered to release antibiotics in a controlled manner, resulting in sustained therapeutic levels in the vitreous cavity.
- Gene Therapy: Although still experimental, gene therapy approaches seek to deliver genes encoding antimicrobial proteins directly to the eye. This strategy may offer a long-term solution for recurring or chronic infections.
- Immune Modulation: Targeting the immune response to reduce inflammation while maintaining antimicrobial activity is a growing area of interest. Drugs that selectively modulate immune pathways may aid in controlling inflammation and preventing tissue damage in infectious endophthalmitis.
Integrating these treatment options allows healthcare providers to effectively manage infectious endophthalmitis, reduce complications, and improve visual outcomes for patients.
Best Practices to Prevent Infectious Endophthalmitis
- Aseptic Techniques in Surgery: Use strict aseptic techniques during all intraocular surgeries to reduce the risk of infection.
- Preoperative Antisepsis: Prior to surgery, reduce the microbial load on the ocular surface with antiseptic agents such as povidone-iodine.
- Sterile Surgical Environment: Maintain a sterile surgical environment by properly sterilizing instruments and using sterile drapes and gloves.
- Postoperative Care: Educate patients on the importance of postoperative care, such as using prescribed antibiotic eye drops correctly and not touching or rubbing their eyes.
- Prompt Treatment of Ocular Injuries: Seek emergency medical attention for any ocular trauma, and ensure proper wound care and prophylactic antibiotic administration if necessary.
- Management of Systemic Infections: Treat systemic infections immediately to prevent hematogenous spread to the eye. Closely monitor patients with risk factors such as endocarditis or immunosuppression.
- Regular Follow-Up: After ocular surgery or trauma, schedule regular follow-up appointments to monitor for signs of infection and provide timely intervention if necessary.
- Patient Education: Teach patients how to recognize early signs of endophthalmitis, such as severe eye pain, redness, and vision changes, and encourage them to seek immediate medical attention if these symptoms appear.
- Use of Protective Eyewear: Encourage the use of protective eyewear in high-risk environments to avoid ocular injuries.
- Vaccination: Make sure your vaccinations are up to date, particularly for conditions that can cause systemic infections and spread to the eye.
Individuals who follow these preventive measures can significantly lower their risk of developing infectious endophthalmitis while also maintaining good overall eye health.
Trusted Resources
Books
- “Endophthalmitis: Diagnosis and Management” by Alastair K. Denniston and Philip I. Murray
- “Intraocular Inflammation” by Manfred Zierhut, Hiroshi Mizuki, and Wayne Streilein
- “Ocular Infection: Investigation and Treatment in Practice” by David BenEzra






