What is eyelid basal cell carcinoma?
Eyelid basal cell carcinoma (BCC) is a skin cancer that develops from basal cells in the epidermis, the skin’s outermost layer. It is the most common malignant tumor of the eyelid, accounting for nearly 90% of all eyelid cancers. This cancer most commonly affects the lower eyelid and the inner corner (medial canthus) of the eye. While it grows slowly and rarely metastasizes, if not treated, it can cause significant local tissue destruction, potentially resulting in disfigurement and functional impairment of the eye. Early detection and treatment are critical for preventing severe damage and preserving vision.
Thorough Examination of Eyelid Basal Cell Carcinoma
Epidemiology
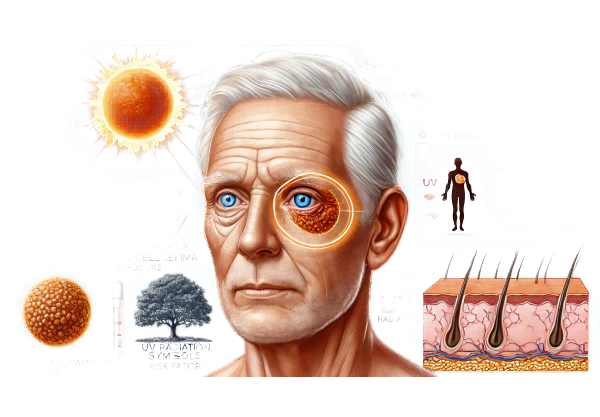
Basal cell carcinoma is the most common type of skin cancer, and the eyelid is a frequent site due to its exposure to ultraviolet (UV) radiation. Individuals over the age of 50 are more likely to develop eyelid BCC, which is more common in men than women. People with fair skin, light hair, and blue or green eyes are more vulnerable due to lower levels of melanin, which provides some protection from UV radiation. Furthermore, those with a history of prolonged sun exposure, tanning bed use, or a family history of skin cancer are more likely to develop this condition.
Risk Factors
Several factors influence the development of eyelid basal cell carcinoma, including:
The primary risk factor is chronic exposure to ultraviolet (UV) radiation from the sun. UV rays damage DNA in skin cells, resulting in mutations that can lead to cancer.
- Fair Skin: People with fair skin have lower melanin levels, making them more susceptible to UV damage.
- Age: The risk of developing eyelid BCC rises with age because cumulative UV exposure causes more DNA damage over time.
- Gender: Men have a higher incidence of eyelid BCC, most likely due to increased lifetime UV exposure.
- Genetic Factors: Genetic conditions like basal cell nevus syndrome (Gorlin syndrome) and a family history of skin cancer raise the risk.
- Immunosuppression: People with weakened immune systems, such as organ transplant recipients or HIV/AIDS patients, are at a higher risk.
Pathophysiology
Basal cell carcinoma develops from basal cells in the epidermis. UV radiation causes mutations in these cells’ DNA, specifically affecting genes involved in cell growth and repair, such as the PTCH1 gene in the Hedgehog signaling pathway. These mutations cause uncontrolled cell proliferation and the development of a tumor.
BCC is distinguished by its slow growth and localized invasiveness. Unlike other cancers, it rarely spreads to distant organs but can cause severe local damage if not treated promptly. The tumor can infiltrate surrounding tissues, including the eye and orbit, causing functional and cosmetic issues.
Clinical Presentation
Eyelid basal cell carcinoma typically appears as a small, pearly nodule with rolled edges and a central ulcer. It can also appear as a flat, scaly patch or a red, inflamed area that does not heal. Telangiectasias (small, visible blood vessels) are commonly found on the lesion’s surface. The tumor typically develops in the lower eyelid and medial canthus, but it can appear anywhere on the eyelid.
Symptoms vary according to the tumor’s size and location and may include:
- Lump or Nodule: A persistent lump or bump on the eyelid that can bleed, crust, or ulcer.
- Changes in Appearance: As the tumor grows, the shape and appearance of the eyelid may change noticeably.
- Loss of Eyelashes: Tumors near the eyelash line can cause loss of eyelashes.
- Discomfort or Pain: Although most tumors are painless, some can cause discomfort or pain, particularly if they ulcerate or become infected.
Histological Subtypes
Eyelid BCC can be classified into several histological subtypes, each with unique characteristics and clinical implications:
- Nodular BCC: The most common subtype, which appears as a shiny, pearly nodule with telangiectasias. It frequently ulcerates, resulting in the term “rodent ulcer.”
- Superficial BCC: A flat, scaly red patch that is commonly mistaken for eczema or psoriasis. It has a higher recurrence rate if not completely removed.
- Morpheaform (Sclerosing) BCC: It appears as a scar-like, indurated lesion with ill-defined borders. This subtype is more aggressive and may infiltrate deeper tissues, making surgical removal difficult.
- Basosquamous Carcinoma: A rare variant that resembles both basal and squamous cell carcinoma. It has a higher risk of metastasis than other BCC subtypes.
Differential Diagnosis
Several conditions can mimic the appearance of eyelid BCC, so differential diagnosis is critical.
- Unlike BCC, SCC can metastasize. It typically manifests as a scaly, red, and crusted lesion.
- Sebaceous Gland Carcinoma: A rare but aggressive malignancy of the sebaceous glands that typically appears as a painless nodule.
- Chalazion: A benign, inflammatory lesion of the eyelid’s meibomian glands that is frequently mistaken for BCC in its early stages.
- Melanoma: Though uncommon on the eyelid, melanoma can appear as a pigmented lesion with irregular borders and color variations.
- Benign Lesions: Actinic keratosis, keratoacanthoma, and benign nevi may resemble BCC but have different prognoses and treatment options.
Complications
If left untreated, eyelid BCC can cause a number of complications, including:
- Local Tissue Destruction: The tumor can invade nearby structures, such as the orbit, eye, and surrounding facial tissues, resulting in significant disfigurement and functional impairment.
- Recurrence: Incomplete removal may result in recurrence, necessitating additional surgery and reconstruction.
- Secondary Infections: Ulcerated tumors may become infected, resulting in additional pain and complications.
Psychological and Social Impact
Living with eyelid BCC can have serious psychological and social consequences, especially if the tumor causes obvious disfigurement. Patients may experience anxiety, depression, and social withdrawal as a result of their appearance concerns. It is critical that healthcare providers address these concerns and offer support throughout the treatment process.
Methods for Eyelid BCC Diagnosis
Clinical Examination
Diagnosing eyelid BCC begins with a thorough clinical examination by an ophthalmologist or dermatologist. Important components of the clinical evaluation include:
- Visual Inspection: Examine the lesion’s size, shape, color, and surface characteristics. BCC frequently presents as a pearly nodule with rolled edges and central ulceration.
- Palpation: Feeling the lesion to check for consistency and any underlying induration or fixation to deeper tissues.
- Dermatoscopy: A dermatoscope, a specialized magnifying device, is used to examine the lesion in greater detail. Dermatoscopy can reveal BCC-specific features such as arborizing blood vessels, blue-gray ovoid nests, and ulcers.
Biopsy
Eyelid BCC can only be diagnosed definitively through histopathological examination via biopsy. Depending on the size and location of the lesion, various biopsy techniques are used.
- Punch Biopsy: A small, circular section of tissue is removed with a punch tool. This method is useful for sampling small lesions or taking a representative tissue section from larger lesions.
- Shave Biopsy: The lesion is removed with a blade. This technique is commonly used for superficial lesions, but it may not be appropriate for deeper or infiltrative tumours.
- Excisional Biopsy: The entire lesion is removed; this is commonly used for small tumors where complete excision is possible. This method provides a comprehensive histological evaluation and can be used for both diagnostic and therapeutic purposes.
Imaging Studies
Imaging studies are essential for determining the size of the tumor and planning surgical intervention. Common imaging modalities are:
- High-Frequency Ultrasound: Produces detailed images of the lesion’s depth and the involvement of nearby structures. It is especially useful for determining tumor thickness and preparing excision margins.
- CT Scan: A CT scan can aid in determining deeper invasion of the orbit or adjacent facial bones, particularly in larger or more aggressive tumors.
- MRI: MRI is useful for evaluating soft tissue involvement and orbital extension. It has higher contrast resolution than CT, making it suitable for detailed anatomical evaluation.
Histopathologic Examination
A pathologist examines the biopsy specimen through a microscope to confirm the diagnosis of BCC. Key histopathological characteristics include:
- Basaloid Cells: The presence of basaloid cells with large nuclei but little cytoplasm. These cells form nests or cords that penetrate the dermis.
- Peripheral Palisading: Tumor cells at the nest’s periphery exhibit a palisading pattern, indicating BCC.
- Stromal Reaction: The surrounding stroma may exhibit a desmoplastic reaction, especially in the morpheaform subtype.
Differential Diagnosis
Additional diagnostic tests, such as immunohistochemical staining, may be used to distinguish BCC from other skin cancers and benign conditions. These tests help to confirm the diagnosis and guide the appropriate treatment.
Eyelid BCC Therapy Methods
Standard Treatment Options
- Surgical excision:
Surgical excision is the most common and effective way to treat eyelid basal cell carcinoma. The tumor is removed along with a margin of healthy tissue to ensure complete excision. This method is particularly effective for small, well-defined tumors. - Mohs Micrographic Surgery:
- Mohs surgery is a specialized surgical procedure used to treat BCC, particularly in cosmetically sensitive areas such as the eyelids. It entails the sequential removal and examination of tissue layers until no cancerous cells remain. This method ensures that the tumor is completely removed while leaving as much healthy tissue as possible.
- Curettage and electrodessication:
- This procedure involves scraping away the tumor tissue (curettage) and then applying an electric current to kill any remaining cancer cells (electrodessication). It is appropriate for small, superficial BCCs, but less effective for aggressive or recurring tumors.
- Cryotherapy:
- Cryotherapy freezes and destroys cancerous tissues by using extremely cold temperatures. Liquid nitrogen is applied to the tumor, killing the cells. The delicate nature of the surrounding tissues makes this method less commonly used for eyelid BCC.
- Radiation Therapy:
- Radiation therapy uses high-energy radiation to target and destroy cancer cells. It is usually reserved for patients who are not good candidates for surgery or who have tumors in hard-to-reach areas. Radiation therapy may require multiple sessions and can result in side effects such as skin irritation and pigmentation changes.
Innovative and Emerging Therapies
- Photodynamic Treatment (PDT):
- PDT is a new treatment that uses a photosensitizing agent and a specific wavelength of light to kill cancer cells. The agent is applied to the tumor and activated by light, resulting in reactive oxygen species that kill cancer cells. PDT is a minimally invasive procedure that has shown promise in treating superficial BCCs.
- Topical Treatment:
- Topical medications, such as imiquimod and 5-fluorouracil, can be applied directly to the tumour to boost the immune system or inhibit cancer cell growth. These treatments are most commonly used for superficial BCCs and are less effective for deeper or more aggressive tumors.
- Target Therapy:
- Targeted therapy entails using drugs to specifically target molecular pathways involved in cancer progression. Vismodegib and sonidegib inhibit the Hedgehog signaling pathway, which is frequently mutated in BCCs. These oral medications are prescribed for advanced or metastatic BCCs that cannot be treated surgically or with radiation.
- Immune checkpoint inhibitors:
- Immune checkpoint inhibitors, such as pembrolizumab, are being studied for their ability to treat advanced BCC by boosting the body’s immune response to cancer cells. These medications block proteins that inhibit immune cells, allowing the immune system to attack the tumor.
- Laser therapy:
- Laser therapy employs focused light to remove or destroy cancerous tissues. This method is less invasive and suitable for small, superficial tumors. It has the advantage of leaving minimal scarring and allowing for quick recovery times.
Best Practices for Avoiding Eyelid Basal Cell Carcinoma
- Protect Your Skin From UV Radiation:
- When outdoors, wear UV-protective sunglasses and a wide-brimmed hat. Apply broad-spectrum sunscreen with an SPF of 30 or higher to your face and eyelids, even on cloudy days.
- Avoid tanning beds.
Tanning beds emit UV radiation, which increases the risk of developing BCC. Avoid using them to protect your skin. - Conduct regular skin self-examinations:
- Check your skin on a regular basis for new growths, changes in existing moles, and unusual lesions. Pay close attention to the areas surrounding your eyes and eyelids.
- Plan Routine Dermatological Check-ups:
- See a dermatologist once a year or as recommended for professional skin examinations. Early detection of any suspicious lesions allows for prompt treatment.
- Be aware of sun exposure:
- Limit your sun exposure, particularly during peak hours (10 a.m. to 4 p.m.). Seek shade whenever possible and dress in protective clothing.
- Lead a Healthy Lifestyle:
- A healthy diet high in antioxidants, regular exercise, and adequate hydration can improve skin health and immune function.
- Avoid smoking and limit your alcohol consumption:
- Smoking and excessive alcohol consumption can weaken the immune system, increasing the risk of skin cancer.
- Educate Yourself On Skin Cancer Risks:
- Stay informed about the risks and symptoms of skin cancer. Knowledge can empower you to take preventive measures and, if necessary, seek medical attention right away.
Trusted Resources
Books
- “Skin Cancer: Recognition and Management” by Robert A. Schwartz
- “Clinical Guide to Skin Diseases” by David Buckley and John R. Horton
- “Cutaneous Malignancy of the Head and Neck: A Multidisciplinary Approach” by Randal S. Weber and Francis B. Quinn
- “Dermatologic Surgery: A Focus on Oncologic Surgery” by Randall K. Roenigk and Henry H. Roenigk






