What is Gyrate Atrophy?
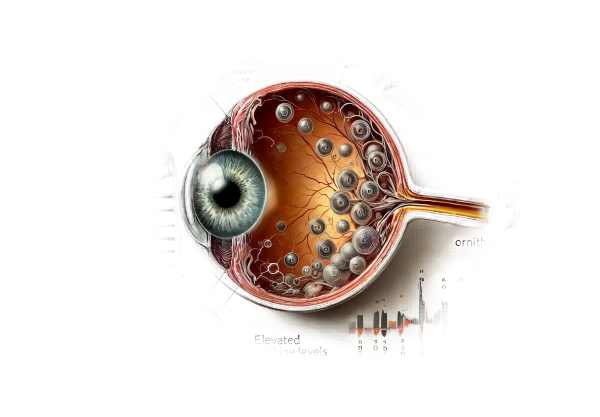
Gyrate atrophy of the choroid and retina is a rare inherited retinal dystrophy with progressive vision loss. It is caused by mutations in the OAT gene, which codes for the enzyme ornithine aminotransferase. This enzyme deficiency causes high levels of ornithine, which is toxic to the retinal pigment epithelium and choroid. The condition appears as patches of choroidal and retinal atrophy, primarily in the peripheral retina, resulting in a gradual loss of night vision, peripheral vision, and, eventually, central vision. Early diagnosis and treatment are critical for slowing the progression of this debilitating disease.
In-Depth Look at Gyrate Atrophy
Gyrate atrophy is an autosomal recessive disorder that causes progressive degeneration of the choroid and retina, resulting in severe visual impairment. It is a metabolic disorder caused by mutations in the ornithine aminotransferase (OAT) gene on chromosome 10q26. The enzyme deficiency causes hyperornithinemia, in which ornithine levels in the blood are significantly elevated, causing toxic effects on ocular tissues.
Pathophysiology
Gyrate atrophy is caused by the accumulation of ornithine in the body as a result of a lack of functional OAT enzyme. Ornithine is an amino acid that participates in the urea cycle. Excessive amounts cause the formation of ornithine ketoacids, which are toxic to the retinal pigment epithelium (RPE) and choroid. The damage begins in the peripheral retina and progresses to the central retina over time.
Clinical Manifestations
Gyrate atrophy patients usually exhibit symptoms in childhood or adolescence. The first symptom is usually night blindness (nyctalopia), which is followed by a progressive loss of peripheral vision. As the disease progresses, central vision is compromised, resulting in significant visual impairment by the third or fourth decade of life.
- Night Blindness: One of the earliest symptoms, frequently observed in childhood.
- Peripheral Vision Loss: Progressive narrowing of the visual field, resulting in tunnel vision.
- Central Vision Loss: Develops later and significantly impairs daily activities.
- Fundus Changes: Ophthalmoscopic examination reveals well-defined areas of chorioretinal atrophy with a scalloped border that begins in the mid-periphery and extends to the posterior pole.
- Electroretinography (ERG) reveals reduced rod and cone responses, indicating widespread retinal dysfunction.
Genetic Aspects
Gyrate atrophy is inherited in an autosomal recessive pattern, which means that affected individuals receive two copies of the mutated gene, one from each parent. Carriers of a single mutated gene do not usually exhibit symptoms. Affected families should seek genetic counseling to better understand their inheritance pattern and the risks associated with future offspring.
Disease Progression
The progression of gyrate atrophy is variable, but it generally follows this predictable pattern:
- Early Stage: Night blindness with peripheral field defects.
- Intermediate Stage: Atrophic areas expand toward the posterior pole, with more pronounced visual field constriction.
- Advanced Stage: Macula involvement, resulting in central vision loss that makes reading and recognizing faces difficult.
Effects on Quality of Life
Gyrate atrophy has a significant impact on the quality of life for those affected. The disease’s progressive nature makes it increasingly difficult to perform daily activities like reading, driving, and recognizing faces. Night blindness and peripheral vision loss impair mobility, making it difficult to navigate in low-light or crowded areas. The psychological effects of progressive vision loss can be severe, with patients experiencing anxiety, depression, and social isolation.
Associated Systemic Manifestations
While gyrate atrophy primarily affects the eyes, elevated ornithine levels can also cause other systemic symptoms, though these are less common. These could include muscle weakness and abnormalities in the central nervous system. However, these systemic effects are usually minor in comparison to the ocular symptoms.
Research and Future Directions
Gyrate atrophy research is ongoing, with the goal of better understanding the disease’s molecular mechanisms and developing targeted therapies. Advances in gene therapy and enzyme replacement therapy show promise in treating the underlying cause of the disease. Furthermore, dietary interventions to lower ornithine levels are being investigated as a potential management strategy.
Importance of Early Diagnosis
Early detection of gyrate atrophy is critical for implementing management strategies that will slow disease progression and preserve vision for as long as possible. Regular monitoring and timely interventions can help reduce the disease’s impact on a patient’s quality of life.
Methods for Detecting Gyrate Atrophy
Gyrate atrophy of the choroid and retina is diagnosed using a combination of clinical evaluation, imaging studies, and genetic tests. Early and accurate diagnosis is critical for managing the condition and developing effective interventions.
Clinical Evaluation
A thorough ophthalmic examination is the first step in diagnosing gyrate atrophy. Key components are:
- History Taking: Conduct a thorough patient history to document symptoms, onset, and progression of visual disturbances, particularly night blindness and peripheral vision loss.
- Visual Field Testing: To determine the extent of peripheral vision loss and the characteristic constriction of the visual field.
- Fundus Examination: Using ophthalmoscopy to detect the distinctive scalloped areas of chorioretinal atrophy in the peripheral retina.
Imaging Studies
Imaging studies are critical for confirming the diagnosis and determining the degree of retinal and choroidal involvement.
- Fundus Photography: Produces detailed images of the retinal surface, highlighting atrophic areas and their progression over time.
- Optical Coherence Tomography (OCT): Provides cross-sectional images of the retina that show structural changes and thinning caused by gyrate atrophy.
- Fluorescein Angiography: Visualizes the retinal vasculature and detects choroidal atrophy and leakage.
Electroretinography (ERG)
ERG is a valuable diagnostic tool that measures the retina’s electrical responses to light stimuli. Gyrate atrophy is characterized by reduced rod and cone responses on ERG, indicating widespread retinal dysfunction.
Lab Tests
Biochemical tests to determine plasma ornithine levels are critical for diagnosing gyrate atrophy. Elevated ornithine levels are indicative of the condition and support the diagnosis. Furthermore, enzymatic assays to determine ornithine aminotransferase activity can provide additional confirmation.
Genetic Testing
Genetic testing is definitive for diagnosing gyrate atrophy, which entails sequencing the OAT gene to identify pathogenic mutations. Confirming the genetic basis of the disease is critical for genetic counseling and determining the risk to family members. Genetic testing can also help distinguish gyrate atrophy from other retinal dystrophies that have similar clinical characteristics.
Differential Diagnosis
Differentiating gyrate atrophy from other retinal dystrophies and chorioretinal atrophies is critical for proper diagnosis and treatment. Consider the following conditions when making a differential diagnosis: – Retinitis Pigmentosa: Causes night blindness and peripheral vision loss, but has unique fundus changes and genetics.
- Choroideremia: Another inherited chorioretinal dystrophy with similar features but different genetic and clinical characteristics.
- Central Areolar Choroidal Dystrophy: Unlike gyrate atrophy, which affects the peripheral vision, this condition primarily affects the macula and central vision.
Treatment Options for Gyrate Atrophy
The primary goal of treating gyrate atrophy of the choroid and retina is to slow disease progression and manage symptoms. While there is no cure, a variety of therapeutic approaches can help affected people maintain their vision and improve their quality of life.
Standard Treatment Options:
- Vitamin B6 Supplementation: Some patients with gyrate atrophy benefit from high doses of vitamin B6 (pyridoxine). This is because certain OAT gene mutations respond to vitamin B6, which can increase residual enzyme activity while decreasing plasma ornithine levels. For best results, ornithine levels should be monitored on a regular basis, and vitamin B6 dosage should be adjusted accordingly.
- Ornithine-Restricted Diet: Following a diet low in arginine, a precursor to ornithine, can help lower plasma ornithine levels. This diet entails limiting high-protein foods while ensuring adequate nutrition through specialized dietary plans designed in consultation with a nutritionist.
- Amino Acid Supplementation: Taking specific amino acids, such as lysine, can help balance your amino acid profile and reduce the formation of ornithine.
Innovative and Emerging Therapies
- Gene Therapy: As we gain a better understanding of the genetic basis of gyrate atrophy, gene therapy shows great promise. Gene therapy works by delivering a functional copy of the OAT gene to retinal cells, restoring enzyme activity and preventing further degeneration. While still in the experimental stage, this approach has the potential to provide a long-term solution for patients with gyrate atrophy.
- Enzyme Replacement Therapy: This novel therapy directly supplements the deficient enzyme ornithine aminotransferase. Researchers are investigating various delivery methods, such as intravitreal injections and systemic administration, to determine the most effective approach to enzyme replacement.
- Pharmacological Chaperones: These small molecules can stabilize and improve the function of the mutant OAT enzyme, potentially lowering ornithine levels and slowing disease progression. Ongoing research focuses on identifying and optimizing these chaperones for clinical applications.
- Retinal Prosthetics and Implants: In advanced cases where significant vision loss has occurred, retinal prosthetics and implants, such as the Argus II retinal prosthesis system, can help restore visual function. These devices convert visual information into electrical signals, which stimulate the remaining retinal cells, resulting in artificial vision.
Supportive treatments for gyrate atrophy include using magnifying glasses, special lighting, and other low vision aids to improve daily activities and quality of life.
- Psychosocial Support: Counseling and support groups can offer patients and their families emotional support as well as practical advice to help them cope with the challenges of living with progressive vision loss.
Combining these treatment approaches can effectively manage gyrate atrophy, preserving vision and improving the quality of life for those affected.
Prevention Tips for Gyrate Atrophy
While gyrate atrophy is a genetic condition that cannot be completely avoided, certain practices can help reduce the risk and lessen its impact:
- Genetic Counseling: People with a family history of gyrate atrophy should get genetic counseling to better understand their risk and consider genetic testing. This can help with early detection and timely intervention.
- Regular Eye Examinations: Routine eye exams can detect early signs of gyrate atrophy, allowing for timely treatment. Individuals at risk should have comprehensive eye exams once a year, or as recommended by their ophthalmologist.
- Maintain a Healthy Diet: Following an ornithine-restricted diet under the supervision of a nutritionist can help manage ornithine levels while slowing disease progression.
- Avoid High-Protein Foods: Eating fewer high-protein foods can help reduce ornithine production. Consult a nutritionist to create a balanced diet that meets nutritional requirements while avoiding excessive protein consumption.
- Vitamin B6 Supplementation: For people with B6-responsive mutations, taking high doses of vitamin B6 as directed by a doctor can help lower ornithine levels and slow disease progression.
- Stay Informed: Staying up to date on the latest research and developments in the treatment of gyrate atrophy can help patients and their families make informed decisions about their care.
- Protect Your Eyes: Wearing sunglasses to protect your eyes from UV rays and avoiding environmental stressors that can worsen vision loss.
Individuals at risk for gyrate atrophy can take proactive steps to manage their condition and improve their eye health by implementing these preventive measures.
Trusted Resources
Books
- “Inherited Retinal Diseases: A Diagnostic and Therapeutic Approach” by Stephen H. Tsang
- “Retinal Degenerative Diseases: Mechanisms and Experimental Therapy” by Catherine Bowes Rickman, Matthew M. LaVail, and Christine Grimm
- “Retina” by Stephen J. Ryan










