Eyelid basal cell carcinoma (BCC) is the most common malignant tumor of the eyelid, making up more than 90% of all eyelid cancers. Early identification and timely intervention are crucial to prevent local tissue destruction and protect both vision and cosmetic function. This comprehensive, patient-centered guide covers everything from understanding the risk factors, warning signs, and progression of eyelid BCC, to evidence-based treatment pathways. We’ll explore mainstream non-surgical options, surgical and reconstructive strategies, and highlight the latest advances in diagnostics, targeted therapies, and clinical research. Our goal is to empower you with practical knowledge and guidance to support optimal outcomes and peace of mind.
Table of Contents
- Condition Background and Risk Profile
- Mainstream Medical and Drug Therapies
- Surgical Procedures and Local Interventions
- Cutting-Edge Therapies and Advanced Technologies
- Ongoing Clinical Research and What Lies Ahead
- Frequently Asked Questions
- Disclaimer
Condition Background and Risk Profile
Basal cell carcinoma (BCC) is a slow-growing, locally invasive skin cancer originating from the basal cells in the epidermis. When it affects the eyelid, BCC can threaten both vision and appearance, due to the delicate structures and functional importance of this region.
What is Eyelid Basal Cell Carcinoma?
- A malignant tumor that arises from the basal cells, typically on the lower eyelid but can occur anywhere on the lid margin.
- While BCC rarely spreads to distant organs, it can aggressively invade local tissues, including the eye, orbit, and bone if untreated.
Common Subtypes:
- Nodular: Most prevalent; appears as a pearly nodule with visible blood vessels.
- Morpheaform (sclerosing): Flat, scar-like lesion; more aggressive, harder to define edges.
- Superficial: Thin, erythematous patches, sometimes resembling eczema.
- Pigmented: Contains melanin, mimicking melanoma.
Epidemiology and Prevalence:
- Over 90% of eyelid malignancies are BCC, with the lower eyelid and medial canthus (inner corner) being most affected.
- Most common in fair-skinned individuals, especially those over 50.
- Higher risk with cumulative sun exposure, immunosuppression, prior radiation, or certain genetic syndromes.
Risk Factors:
- Chronic sun or UV exposure (including tanning beds)
- Fair complexion, light eyes, and hair
- Age over 50
- Male gender (slightly higher risk)
- Family or personal history of skin cancer
- Immunosuppression (e.g., organ transplant, HIV)
- Certain genetic conditions (Gorlin syndrome)
Clinical Features and Symptoms:
- Slow-growing, painless nodule or ulcer on the eyelid margin
- Loss of eyelashes (madarosis) in the affected area
- Bleeding, crusting, or non-healing “sore”
- Rolled or raised edges; central ulceration
- Distortion of the eyelid or lash line
- May mimic benign lesions (chalazion, stye), making diagnosis challenging
Pathophysiology:
- DNA damage from UV radiation leads to uncontrolled proliferation of basal cells.
- BCC invades locally and destroys surrounding tissue but very rarely metastasizes.
Prevention and Early Detection:
- Wear broad-spectrum sunscreen, sunglasses, and hats outdoors.
- Avoid peak sunlight hours and tanning beds.
- Perform regular self-exams for new or changing eyelid lesions.
- Promptly report non-healing, bleeding, or suspicious growths to an eye doctor or dermatologist.
Practical Tips:
- Take clear photos of any suspicious eyelid spot to track changes.
- Don’t ignore persistent eyelid “bumps” or sores, especially if you’re at higher risk.
Mainstream Medical and Drug Therapies
While surgery is the gold standard for most eyelid BCCs, medical therapies can play a key role in certain scenarios—such as superficial or inoperable tumors, palliative care, or as an adjunct to surgery.
Topical Medications:
- Imiquimod (Aldara): Immune response modifier, sometimes used off-label for superficial BCC on the eyelid. Applied as a cream 5–7 times per week for several weeks.
- 5-Fluorouracil (5-FU): Topical chemotherapy for very superficial tumors. May cause local irritation; rarely first-line for the eyelid due to sensitivity.
Systemic Therapies:
- Hedgehog Pathway Inhibitors: (e.g., vismodegib, sonidegib) Target molecular pathways driving BCC growth. Indicated for advanced, recurrent, or metastatic BCC not suitable for surgery or radiotherapy.
- Oral medication taken daily, can shrink or stabilize tumors.
- Side effects: muscle cramps, hair loss, altered taste, weight loss.
Radiation Therapy:
- Reserved for patients who are poor surgical candidates or have unresectable tumors.
- Fractionated radiotherapy, often 5 days/week for several weeks.
- Not suitable for all cases, especially in younger patients due to long-term risks.
Observation:
- In select, frail, or elderly patients, slow-growing lesions may be observed if the risks of intervention outweigh the benefits.
Adjunctive Measures:
- Good eyelid hygiene, gentle cleansing, and moisturizing can support healing during medical treatments.
Limitations:
- Medical therapies are less effective for deep, nodular, or morpheaform subtypes.
- They may be used as neoadjuvant therapy (to shrink tumors before surgery) in select cases.
Practical Advice:
- Strictly follow application instructions for topical treatments—overuse can damage surrounding skin.
- Communicate any new symptoms, pain, or swelling promptly to your care team.
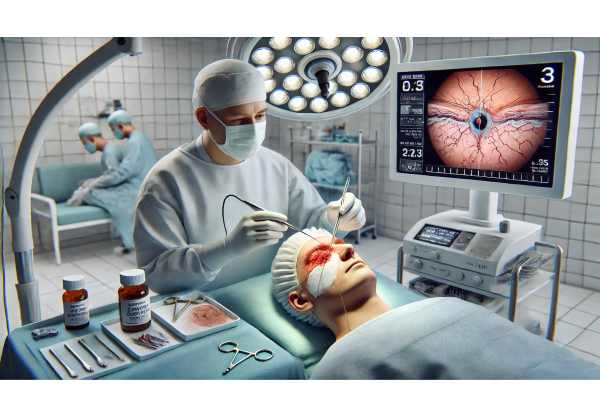
Surgical Procedures and Local Interventions
Surgical excision remains the cornerstone of eyelid BCC management. The aim is complete tumor removal with the best possible cosmetic and functional outcome.
Standard Surgical Techniques:
- Excisional Biopsy: Entire lesion removed with a margin of healthy tissue; sent for histopathological analysis.
- Mohs Micrographic Surgery: Gold standard for high-risk, recurrent, or poorly defined BCCs. Involves staged excision and real-time microscopic examination, maximizing tissue preservation and cure rates.
- Curettage and Electrodessication: Reserved for small, superficial tumors away from vital structures.
- Cryosurgery: Rarely used for eyelids due to risk of scarring and tissue damage.
Reconstructive Techniques:
- Eyelid reconstruction is often necessary, especially for large tumors.
- Options include direct closure, local flaps, skin grafts, or composite grafts—tailored to defect size and location.
- Goals are to restore lid margin, protect the eye, and maintain eyelid mobility and appearance.
Sentinel Lymph Node Biopsy:
- Rarely indicated for eyelid BCC, as metastatic spread is extremely uncommon.
Perioperative Considerations:
- Pre-surgical mapping and marking to define tumor margins.
- Use of local or general anesthesia, based on patient and lesion characteristics.
- Collaboration between oculoplastic surgeons, dermatologists, and pathologists.
Postoperative Care:
- Ice packs to reduce swelling
- Antibiotic ointments to prevent infection
- Suture removal in 5–14 days, depending on repair
- Scar massage and sun protection to optimize healing
Risks and Complications:
- Incomplete removal (requiring re-excision)
- Infection, bleeding, poor wound healing
- Eyelid malposition (ectropion, entropion), notching, or lid retraction
- Need for secondary reconstructive procedures
Practical Tips:
- Ask your surgeon about Mohs surgery if your BCC is near the eye or has ill-defined borders.
- Follow post-op instructions meticulously to prevent complications and scarring.
Cutting-Edge Therapies and Advanced Technologies
Rapid progress in the understanding and management of eyelid BCC is improving outcomes and patient experiences.
Non-Invasive Diagnostics:
- Reflectance Confocal Microscopy (RCM): In-office, real-time imaging to assess lesion margins without biopsy.
- Optical Coherence Tomography (OCT): High-resolution, non-invasive imaging to guide diagnosis and monitor response to therapy.
Targeted Therapies:
- Ongoing trials of next-generation Hedgehog pathway inhibitors with improved efficacy and fewer side effects.
- Development of topical agents with deeper penetration and better tolerability for periocular use.
Immunotherapies:
- Early-phase studies exploring immune checkpoint inhibitors for advanced, refractory BCC.
- Combining immunotherapy with radiation or surgery to enhance tumor control.
AI and Digital Pathology:
- Artificial intelligence to assist in early detection and delineation of tumor margins.
- Computer-assisted Mohs mapping and reconstructive planning for more precise outcomes.
Personalized Medicine:
- Genomic profiling to predict aggressiveness and tailor therapy.
- Use of patient-derived organoids (mini-tumors grown from individual patients) to test drugs in the lab.
Wearable and App-Based Monitoring:
- Smartphone apps enabling remote monitoring and tracking of lesion changes over time.
- Digital reminders for medication application and post-surgical care.
Practical Advice:
- Inquire about eligibility for clinical trials, especially for recurrent, aggressive, or inoperable BCC.
- Use technology to document lesion changes and share with your care team for timely advice.
Ongoing Clinical Research and What Lies Ahead
Research into eyelid BCC is focused on improving cure rates, minimizing invasiveness, and enhancing quality of life.
Current Clinical Trials:
- New Hedgehog pathway inhibitors and combination regimens for advanced BCC.
- Immunotherapy trials, particularly for BCC resistant to conventional therapies.
- Innovations in reconstructive surgery, including biomaterials and 3D-printed scaffolds.
Prevention and Early Detection:
- Studies on wearable UV sensors and apps to monitor sun exposure.
- Genetic and molecular risk stratification to identify high-risk individuals for more frequent surveillance.
Minimally Invasive Diagnostics:
- Validation of RCM, OCT, and AI-assisted tools for earlier, less invasive diagnosis and margin mapping.
- Trials evaluating the accuracy and impact of teledermatology for remote assessment.
Quality of Life and Cosmetic Outcomes:
- Long-term studies of patient satisfaction, vision, and psychosocial adjustment after eyelid BCC treatment.
- Research into interventions that minimize scarring and optimize eyelid function.
Future Directions:
- Increased integration of digital health tools for monitoring and follow-up.
- Personalized, risk-based algorithms for selecting treatment modalities.
- Combination therapies to further reduce recurrence and enhance healing.
Patient Participation:
- Many research centers offer opportunities for patients to participate in trials—ask your specialist about options.
Practical Tips:
- Stay informed about new therapies if you have recurrent or high-risk BCC.
- Ask about reconstructive options and support services for emotional adjustment.
Frequently Asked Questions
What is the most effective treatment for eyelid basal cell carcinoma?
The most effective treatment is usually complete surgical excision, ideally with Mohs micrographic surgery for high-risk or cosmetically sensitive areas. This provides the highest cure rates while preserving healthy tissue.
Can basal cell carcinoma on the eyelid spread to other parts of the body?
Basal cell carcinoma very rarely spreads (metastasizes) to distant organs. However, it can cause significant local tissue destruction and invade surrounding structures if not treated early.
What are the signs of basal cell carcinoma on the eyelid?
Common signs include a persistent, painless nodule or sore, ulceration, loss of eyelashes, bleeding, or a pearly, rolled-edge lesion. Any non-healing or changing eyelid lesion should be evaluated by a specialist.
Is radiation therapy safe for eyelid basal cell carcinoma?
Radiation therapy can be safe and effective for select patients who are not surgical candidates. It is less commonly used for younger patients due to long-term risks and the potential for skin changes.
How long does it take to recover from eyelid BCC surgery?
Most patients recover from eyelid surgery within 1–2 weeks, with stitches removed in 5–14 days. Healing and scar maturation continue over months. Postoperative care is crucial for the best outcome.
Are there non-surgical treatments for eyelid basal cell carcinoma?
Yes, topical medications and systemic therapies exist for superficial or inoperable BCC, but surgery remains the gold standard. Non-surgical options may be used in select cases or as adjuncts.
Can eyelid basal cell carcinoma come back after treatment?
Recurrence is possible, especially with aggressive subtypes or incomplete removal. Regular follow-up and prompt treatment of any new lesions are essential for ongoing health.
Disclaimer
The information in this article is provided for educational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider or an eye specialist for questions about your health. Never disregard medical advice or delay seeking treatment based on information here.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media. Your support helps us continue to provide trusted, expert health content to readers everywhere.






