Definition of Mucoepidermoid Carcinoma of the Lacrimal Gland
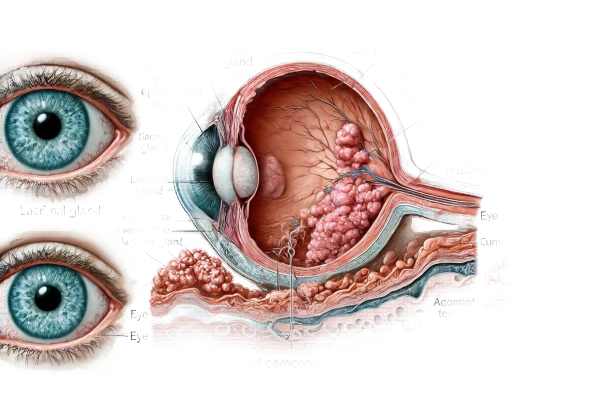
Mucoepidermoid carcinoma of the lacrimal gland is a rare and aggressive malignant tumor that develops from the epithelial cells of the lacrimal gland. The lacrimal gland, which is located in the upper outer region of the orbit, is responsible for tear production. The presence of both mucous and epidermal cells distinguishes this carcinoma. Because of its rarity and aggressive nature, early detection and treatment are critical to improving patient outcomes.
Detailed Investigation of Mucoepidermoid Carcinoma of the Lacrimal Gland
Mucoepidermoid carcinoma of the lacrimal gland is a rare malignancy that affects the gland responsible for tear production. Understanding the pathology, clinical presentation, and potential complications of this condition is critical for both healthcare providers and patients.
Pathophysiology
Mucoepidermoid carcinoma develops from epithelial cells that line the ducts of the lacrimal gland. These tumors contain varying amounts of mucous-secreting cells, squamous (epidermoid) cells, and intermediate cells. The proportion of these cell types, degree of cellular atypia, and presence of cystic spaces determine the histological grade of mucoepidermoid carcinoma.
- Low-grade tumors: These tumors have well-differentiated cells, including prominent mucous cells, minimal cellular atypia, and numerous cystic spaces. They typically grow slowly and have a better prognosis.
- Intermediate-grade tumors: These tumors have characteristics that are similar to both low and high-grade tumors. They exhibit moderate atypia, fewer cystic spaces, and a higher number of epidermoid cells.
- High-grade tumors have poor differentiation, a predominance of epidermoid cells, significant cellular atypia, and fewer cystic spaces. They are extremely aggressive, frequently invade surrounding tissues, and have a high risk of metastasis.
Clinical Presentation
The clinical symptoms of mucoepidermoid carcinoma of the lacrimal gland vary according to the tumor’s size and location. Typical presenting symptoms include:
- Pain and Swelling: Patients frequently report painful swelling in the upper outer quadrant of their orbit, near the lacrimal gland.
- Proptosis: A tumor can cause the eye to protrude forward, which is known as proptosis.
- Diplopia: Double vision can occur as a result of eye displacement or extraocular muscle involvement.
- Epiphora: Excessive tearing, also known as epiphora, is a common result of lacrimal duct obstruction.
- Reduced Visual Acuity: Tumor growth can compress the optic nerve or other ocular structures, resulting in vision loss.
Epidemiology
Mucoepidermoid carcinoma of the lacrimal gland is extremely rare, with only a few cases described in the medical literature. It affects adults more frequently than children, with no discernible gender bias. The condition’s rarity frequently complicates diagnosis and the development of standardized treatment protocols.
Risk Factors
While the exact cause of mucoepidermoid carcinoma is unknown, several risk factors have been identified:
- Radiation Exposure: Previous radiation therapy to the head and neck region may increase the risk of developing this malignancy.
- Genetic Predisposition: These tumors may develop due to genetic mutations or chromosomal abnormalities.
- Chronic Inflammation: Long-term inflammatory conditions of the lacrimal gland may predispose people to cancer.
Complications
Mucoepidermoid carcinoma of the lacrimal gland can cause a number of serious complications if not diagnosed and treated promptly:
- Local Invasion: The tumor may invade nearby structures such as the orbit, sinuses, and brain, resulting in significant morbidity.
- Metastasis: High-grade tumors are more likely to spread to regional lymph nodes and distant organs, such as the lungs and liver.
- Vision Loss: Compression or invasion of ocular structures can cause permanent vision loss.
- Recurrence: Even after treatment, tumors can recur, especially in high-grade malignancies.
Differential Diagnosis
When assessing a patient with suspected mucoepidermoid carcinoma of the lacrimal gland, it is critical to consider other conditions that may cause similar symptoms. Differential diagnosis includes:
- Benign Lacrimal Gland Tumors: Pleomorphic adenomas and other benign tumors can cause similar orbital swelling and discomfort, but they typically have a slower progression.
- Other Malignant Tumors: Adenoid cystic carcinoma, lymphoma, and metastatic lesions to the lacrimal gland should be considered.
- Inflammatory Conditions: Dacryoadenitis (inflammation of the lacrimal gland) caused by an infectious or autoimmune process can mimic the appearance of mucoepidermoid carcinoma.
Histopathological Features
Histopathology remains the gold standard for detecting mucoepidermoid carcinoma. Biopsy samples usually contain a mix of mucous, epidermoid, and intermediate cells. The level of cellular differentiation and the presence of cystic spaces aid in grading the tumor and predicting its prognosis. Immunohistochemical staining can help distinguish mucoepidermoid carcinoma from other lacrimal gland tumors.
Molecular and Genetic Studies
Recent advances in molecular genetics have shed light on the pathogenesis of mucoepidermoid carcinoma. Some cases have shown chromosomal translocations involving the MECT1 and MAML2 genes. These genetic changes may contribute to tumor development and progression, and their presence can have diagnostic and prognostic significance.
Imaging Studies
Imaging studies are critical to the diagnosis and staging of mucoepidermoid carcinoma. Modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) aid in determining the extent of the tumor and its involvement in adjacent structures. These imaging techniques are extremely useful for surgical planning and monitoring for recurrence.
Prognosis
Several factors influence the prognosis of mucoepidermoid carcinoma of the lacrimal gland, including the tumor’s histological grade, size, and presence of metastasis. Low-grade tumors typically have a better prognosis with appropriate treatment, whereas high-grade tumors have a worse prognosis due to their aggressive nature and increased risk of metastasis.
Diagnostic methods
An accurate and timely diagnosis of mucoepidermoid carcinoma of the lacrimal gland is critical for effective treatment. The diagnostic process combines clinical evaluation, imaging studies, and histopathological examination.
Clinical Evaluation
The first step in diagnosing mucoepidermoid carcinoma is a thorough clinical examination by an ophthalmologist or oculoplastic specialist. This includes a thorough medical history, with emphasis on the onset and progression of symptoms, as well as any relevant risk factors. A thorough eye examination is performed to determine visual acuity, ocular motility, and the presence of proptosis or swelling in the lacrimal gland area.
Imaging Studies
- Computed Tomography (CT) Scan: A CT scan of the orbits can reveal detailed information about the tumor’s size, shape, and extent. It aids in the identification of bony involvement, calcifications, and the tumor’s relationship to surrounding structures. CT scans are especially useful for surgical planning.
- Magnetic Resonance Imaging (MRI): MRI provides superior soft tissue contrast and is invaluable for determining the extent of the tumor’s soft tissue involvement. It shows detailed images of the lacrimal gland, optic nerve, and other orbital structures. MRI is also useful for detecting intracranial extension and evaluating treatment outcomes.
- Ultrasound: Although ultrasound is less commonly used, it can be useful in evaluating the lacrimal gland and distinguishing solid tumors from cystic lesions. It is a non-invasive and cost-effective imaging method.
Histopathologic Examination
Histopathological examination of a biopsy sample is still the most reliable way to diagnose mucoepidermoid carcinoma. A fine-needle aspiration (FNA) or an incisional biopsy is usually used to obtain the biopsy sample. Pathological analysis encompasses:
- Histological Staining: Routine hematoxylin and eosin (H&E) staining aids in identifying the distinct cellular composition of mucoepidermoid carcinoma, which includes mucous, epidermoid and intermediate cells.
- Immunohistochemistry: Immunohistochemical staining can help distinguish mucoepidermoid carcinoma from other lacrimal gland tumors and metastatic lesions. The diagnosis is confirmed using markers such as cytokeratins, mucin stains, and specific epithelial markers.
Molecular and Genetic Testing
In cases where the diagnosis is unclear, molecular and genetic testing can provide additional information. FISH and PCR techniques can detect chromosomal translocations and genetic mutations linked to mucoepidermoid carcinoma. These tests can also aid in prognosis and guiding targeted treatments.
Differential Diagnosis
A thorough differential diagnosis is required to rule out other conditions that might present similarly. This includes benign tumors, malignant tumors of the lacrimal gland, and inflammatory diseases. Accurate differentiation is critical for effective treatment planning.
Treatment for Mucoepidermoid Carcinoma in the Lacrimal Gland
The treatment of mucoepidermoid carcinoma of the lacrimal gland usually consists of surgical intervention, radiation therapy, and, in some cases, chemotherapy. The grade, size, and location of the tumor, as well as the patient’s overall health, all influence treatment decisions. In this article, we will look at both traditional and emerging treatments for this rare cancer.
Surgical Treatment
- Complete Surgical Excision: The primary treatment for mucoepidermoid carcinoma is surgical removal of the entire tumor. This frequently involves a dacryoadenectomy, which involves the removal of the entire lacrimal gland. Complete excision is required to avoid local recurrence and achieve clean margins.
- Orbital Exenteration: If the tumor has spread to adjacent structures, an orbital exenteration may be required. This radical surgery removes the entire contents of the orbit, including the eye, to ensure complete tumor removal. Although it is aesthetically unpleasant, it may be the only option for aggressive, high-grade tumors.
Radiation Therapy
Radiation therapy is frequently used as an adjunct to surgery, especially when surgical margins are positive or there are inoperable tumors. It can help control local disease and lower the likelihood of recurrence. Intensity-modulated radiation therapy (IMRT) allows for precise tumor targeting while sparing healthy tissue.
Chemotherapy
Chemotherapy is typically reserved for high-grade cancers or metastatic disease. While its role in treating mucoepidermoid carcinoma of the lacrimal gland is not well established, it may be considered when other treatments are unavailable. Cisplatin, carboplatin, and 5-fluorouracil are common chemotherapy agents that are frequently used in combination.
Emerging Therapies
- Targeted Therapy: Advances in molecular biology have resulted in the creation of targeted therapies that attack cancer cells based on their genetic makeup. Mucoepidermoid carcinoma research is currently underway to identify potential targets such as the EGFR (epidermal growth factor receptor) and other molecular markers that may be overexpressed in these tumors. EGFR inhibitors, such as cetuximab and gefitinib, are being studied for efficacy.
- Immunotherapy: Immunotherapy, which uses the body’s immune system to combat cancer, is a promising field of study. Immune checkpoint inhibitors, including pembrolizumab and nivolumab, have shown promise in treating a variety of cancers. Their potential role in treating mucoepidermoid carcinoma of the lacrimal gland is being investigated, particularly for tumors that express PD-L1 (programmed death-ligand 1).
- Gene Therapy: The goal of gene therapy is to correct or introduce genetic material in order to treat or prevent disease. Although still in the experimental stage, gene therapy has the potential to treat mucoepidermoid carcinoma by targeting specific genetic mutations that cause tumour growth and progression.
- Advanced Surgical Techniques: Advancements in surgical techniques, such as minimally invasive and robotic-assisted surgeries, are improving the accuracy and outcomes of tumor removal. These advancements enable more accurate tumor removal, shorter recovery times, and fewer complications.
Palliative Care
Palliative care focuses on improving quality of life for patients with advanced disease who cannot receive curative treatment. This could include pain management, radiation therapy, and supportive care services.
Effective Ways to Improve and Prevent Mucoepidermoid Carcinoma of the Lacrimal Gland
- Regular Eye Exams: Early detection of abnormalities in the lacrimal gland can significantly improve results. Routine eye exams, especially for those with risk factors, can help detect potential problems before they worsen.
- Awareness of Symptoms: Recognizing the signs and symptoms of mucoepidermoid carcinoma, such as swelling, pain, and vision changes, can help with early diagnosis and treatment. Patients who experience these symptoms should seek medical attention right away.
- Protective Measures: Limiting exposure to known risk factors, such as radiation, can help reduce the risk of developing mucoepidermoid carcinoma. Individuals undergoing radiation therapy for other conditions should take precautions to avoid exposure to the lacrimal gland.
- Genetic Counseling: For people who have a family history of ocular cancers or genetic predispositions, genetic counseling can provide valuable information and help guide monitoring and prevention strategies.
- Healthy Lifestyle: Living a healthy lifestyle, which includes a balanced diet, regular exercise, and quitting smoking, can benefit overall eye health and potentially lower the risk of certain cancers.
- Recurrence Monitoring: Patients who have received treatment for mucoepidermoid carcinoma must attend regular follow-up appointments to look for signs of recurrence. Early intervention can help manage recurrent disease more effectively.
- Multidisciplinary Care: Bringing together a team of specialists, including ophthalmologists, oncologists, and radiologists, ensures that individuals at risk or diagnosed with mucoepidermoid carcinoma receive comprehensive care and optimal treatment planning.
- Patient Education: Educating patients about their condition, treatment options, and the importance of following-up care can help them take an active role in their health and achieve better results.
Trusted Resources
Books
- “Ocular Tumors in Animals and Humans” by Robert L. Peiffer and Simon M. Peterson-Jones
- “Orbital Tumors: Diagnosis and Treatment” by Zeynel A. Karcioglu
- “Clinical Ophthalmic Oncology: Lacrimal Gland, Eyelid, and Conjunctival Tumors” by Arun D. Singh






