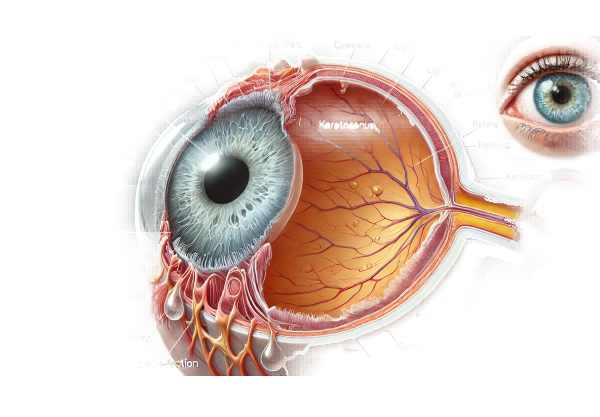
What is keratoconus?
Keratoconus is a progressive eye disorder in which the cornea, or clear front surface of the eye, thins and bulges outward into a cone-like shape. This abnormal shape prevents light entering the eye from properly focusing on the retina, resulting in distorted vision. Keratoconus typically begins in adolescence or early adulthood and progresses for 10-20 years before slowing down. Early detection and management are critical for preserving vision and quality of life.
Detailed Investigation of Keratoconus
Keratoconus is a complex condition that alters the structure and function of the cornea. The cornea’s function is to refract light onto the retina, which is necessary for clear vision. In keratoconus, the cornea thins and weakens, bulging outward in a cone-like shape. This deformation causes irregular astigmatism and myopia, resulting in significant visual impairment.
Causes and Risk Factors
The exact cause of keratoconus is unknown, but it is thought to be a combination of genetic, environmental, and biomechanical factors. There are a number of risk factors:
- Genetics: A family history of keratoconus raises the risk, indicating a hereditary factor. Certain genetic mutations have been associated with the condition.
- Eye Rubbing: Severe or chronic eye rubbing has been linked to the progression of keratoconus, possibly due to mechanical trauma to the cornea.
- Inflammation: Allergic or other irritant-induced chronic eye inflammation can contribute to corneal weakening and keratoconus development.
- Systemic Conditions: Certain systemic diseases, such as Down syndrome, Marfan syndrome, and Ehlers-Danlos syndrome, are associated with an increased risk of keratoconus.
Symptoms
Keratoconus symptoms usually appear in adolescence or early adulthood and progress with time. Common symptoms include:
- Blurred or Distorted Vision: The cornea’s irregular shape scatters light, resulting in blurred and distorted vision.
- Increased Sensitivity to Light and Glare: Patients frequently feel discomfort in bright light conditions.
- Rapid Changes in Prescription: Rapid changes in eyeglass or contact lens prescriptions can be an early indicator of keratoconus.
- Difficulty with Night Vision: Night driving and other low-light activities become difficult due to halos and glare around lights.
Pathophysiology
Keratoconus pathophysiology involves the breakdown of collagen fibers in the cornea, which are necessary for maintaining its shape and strength. Enzymatic activity in the cornea increases, resulting in the breakdown of collagen and extracellular matrix proteins. This weakening of the corneal structure causes it to thin and protrude outward, resulting in the distinctive conical shape.
According to research, oxidative stress and inflammatory mediators contribute to the pathogenesis of keratoconus. Keratoconus patients’ corneal tissue contains higher levels of oxidative stress markers and pro-inflammatory cytokines, which may contribute to corneal thinning and deformation over time.
Stages of Keratoconus
Keratoconus develops in stages, each marked by increasing severity of corneal deformation and visual impairment:
- Early Stage: Mild corneal thinning and minor visual distortion, often treatable with glasses.
- Moderate Stage: More pronounced thinning and irregular astigmatism necessitate the use of rigid gas permeable (RGP) contact lenses for vision correction.
- Advanced Stage: Severe thinning and scarring, significant visual distortion, and the potential for surgical intervention.
Complications
Untreated or advanced keratoconus can result in a variety of complications, including:
- Corneal Scarring: Progressive thinning can result in scarring, further impairing vision.
- Hydrops: A sudden influx of fluid into the cornea due to a tear in Descemet’s membrane can result in severe pain and vision loss.
- Keratoglobus is a rare type of keratoconus in which the entire cornea becomes globular and extremely thin.
Epidemiology
Keratoconus affects roughly one in every 2,000 people worldwide, with some studies indicating higher prevalence rates in specific populations. It typically begins in adolescence and continues into the third or fourth decade of life. Males and females are both affected, though the severity varies by individual.
Quality of Life Impact
Keratoconus has a significant impact on a patient’s quality of life. The condition’s progressive nature often causes frustration and anxiety due to frequent changes in vision and corrective lenses. Difficulties with daily activities like reading, driving, and using digital devices can have an impact on both work performance and social interactions. Individuals with keratoconus require emotional and psychological support, as well as effective management strategies, to improve their quality of life.
Approaches for Diagnosing Keratoconus
A comprehensive eye examination is required to diagnose keratoconus, which includes a detailed assessment of the cornea’s shape and thickness. Early and accurate diagnosis is critical for effective treatment and slowing the progression of the condition.
Clinical Examination
- Visual Acuity Test: Determines the sharpness of vision at various distances, aiding in the diagnosis of visual impairment.
- Refraction Test: This test determines the correct prescription for eyeglasses or contact lenses by measuring how light rays bend as they pass through the cornea and lens.
Corneal Topography
Corneal topography is an important diagnostic tool for determining the surface curvature of the cornea. This non-invasive imaging technique generates a detailed three-dimensional map that highlights the keratoconus-specific thinning and protrusion. Common topography systems used include the following:
- Placido Disk-Based Topography measures corneal curvature using concentric light rings.
- Scheimpflug Imaging: Produces cross-sectional images of the cornea, allowing for precise measurement of its shape and thickness.
Corneal Pachymetry
Corneal pachymetry measures corneal thickness, which is critical for diagnosing and monitoring keratoconus progression. The condition is characterized by corneal thinning, and pachymetry allows for precise measurements to determine the severity.
Slit Lamp Examination
Slit-lamp examinations use a microscope and a bright light to examine the cornea, lens, and other eye structures. This examination aids in detecting signs of keratoconus, such as:
- Vogt’s Striae: Stress on the thinned cornea causes fine, vertical lines in the corneal stroma.
- Fleischer Ring: Iron deposits form a yellow-brown ring around the cone’s base.
Keratometry
Keratometry is a technique for measuring the curvature of the cornea’s anterior surface. It is useful for detecting irregular astigmatism and corneal shape changes that indicate keratoconus. This test is frequently used in conjunction with corneal topography to provide a more comprehensive assessment.
Optical Coherence Tomography(OCT)
OCT is a non-invasive imaging technique that produces high-resolution cross-sections of the cornea. It is effective for detecting early signs of keratoconus and tracking changes in corneal thickness and structure over time. OCT can also aid in the design and evaluation of treatment interventions.
Genetic Testing
In some cases, genetic testing may be recommended to identify keratoconus-related mutations. This is especially beneficial for people with a family history of the condition or those who have other systemic diseases.
Keratoconus Treatment
Keratoconus treatment aims to improve vision while also halting the disease’s progression. The severity of the condition and the patient’s visual needs determine the treatment option. Here, we look at different treatment options and highlight innovative and emerging therapies.
Non-surgical Treatments
- Eyeglasses and Soft Contact Lenses: In the early stages of keratoconus, eyeglasses or soft contact lenses can help with mild myopia and astigmatism. However, as the condition worsens, these options may become ineffective.
- Rigid Gas Permeable (RGP) Contact Lenses: RGP lenses improve vision correction for keratoconus patients by keeping a consistent shape on the irregular cornea, allowing light to be focused more precisely on the retina.
- Scleral Lenses: These large-diameter lenses vault over the cornea to rest on the sclera. Scleral lenses are especially helpful for advanced keratoconus because they provide a smooth optical surface and are more comfortable for patients with severe corneal irregularities.
- Hybrid Contact Lenses: Hybrid lenses combine the characteristics of RGP and soft lenses, with a rigid center and a soft peripheral skirt. They provide the clarity of RGP lenses while maintaining the comfort of soft lenses.
Surgical Treatments
- Corneal Cross-Linking (CXL): This minimally invasive procedure strengthens the cornea by increasing collagen cross-links. CXL involves applying riboflavin (vitamin B2) drops to the cornea and activating them with ultraviolet A (UVA) light. CXL has been demonstrated to slow the progression of keratoconus and, in some cases, improve corneal shape and vision.
- Intacs (intrastromal corneal ring segments): Intacs are small, arc-shaped plastic inserts that are placed in the cornea to flatten its cone-like shape and improve vision. This procedure is most commonly used for moderate keratoconus and can postpone or reduce the need for corneal transplantation.
- Corneal Transplantation: In severe cases where other treatments fail, corneal transplantation (keratoplasty) may be required. There are two primary types:
- Penetrating Keratoplasty (PK) is a full-thickness corneal transplant that replaces the entire cornea with a donor cornea.
• Deep Anterior Lamellar Keratoplasty (DALK): The diseased outer layers of the cornea are replaced, leaving the healthy inner layers intact.
Emerging and Innovative Therapeutics
- Topography-Guided Photorefractive Keratectomy (TG-PRK): This procedure reshapes the cornea and improves vision by using custom laser treatments based on detailed corneal topography maps. TG-PRK is frequently combined with CXL to improve results.
- Customized Contact Lenses: Advances in contact lens technology, such as 3D printing and computer-aided design, have enabled the creation of highly customized lenses tailored to the specific corneal shape of keratoconus patients, resulting in improved comfort and vision.
- Gene Therapy: Research into the genetic basis of keratoconus is currently underway, with the goal of developing gene therapies that could potentially prevent or treat the condition by targeting specific genetic mutations.
- Stem Cell Therapy: Experiments with stem cells aim to regenerate damaged corneal tissue and restore normal function. While still in the research stage, stem cell therapy shows promise for future keratoconus treatments.
Healthcare providers hope to improve keratoconus patients’ outcomes and quality of life by combining established treatments and emerging therapies.
Effective Ways to Improve and Avoid Keratoconus
- Regular Eye Examinations: Have comprehensive eye exams to detect early signs of keratoconus and track its progression. Early intervention can slow or stop the condition’s progression.
- Avoid Eye Rubbing: Avoid rubbing your eyes because it can cause corneal trauma and worsen keratoconus. If you have allergies, treat them properly to avoid eye irritation and rubbing.
- Manage Allergies: Use antihistamines and other allergy medications to alleviate symptoms and reduce the desire to rub your eyes.
- Protect Your Eyes: Wear protective eyewear when participating in activities that could cause eye injury, such as sports or working with hazardous materials.
- Proper Contact Lens Hygiene: Follow the recommended guidelines for cleaning and storing contact lenses to avoid infections and complications that can worsen keratoconus.
- Eat a Healthy Diet: To support overall eye health, consume a well-balanced diet high in antioxidants, vitamins, and minerals. Vitamins C, E, and omega-3 fatty acids are good for the eyes.
- Stay Hydrated: Drink plenty of water to keep your body and eyes hydrated, which can benefit corneal health.
- Avoid UV Exposure: When outdoors, protect your eyes from harmful UV rays by wearing UV-protective sunglasses. UV exposure can harm the cornea and exacerbate keratoconus.
- Follow Treatment Plans: To effectively manage keratoconus, adhere to prescribed treatments and schedule regular appointments with your eye care provider.
Trusted Resources
Book recommendations: Adel Barbara’s “Keratoconus: Diagnosis and Treatment” and Mazen M. Sinjab’s “Corneal Topography in Clinical Practice (Pentacam System)”.






