What is Optic Nerve Glioma?
Optic nerve glioma, also known as optic pathway glioma, is a rare, slow-growing brain tumor that develops from glial cells in the optic nerve. These tumors primarily affect children, with the majority of cases diagnosed before the age of ten. Optic nerve gliomas are frequently associated with neurofibromatosis type 1 (NF1), a genetic disorder that predisposes people to a variety of tumors. This condition can cause vision loss and other neurological symptoms, making early detection and monitoring critical.
In-Depth Look at Optic Nerve Glioma
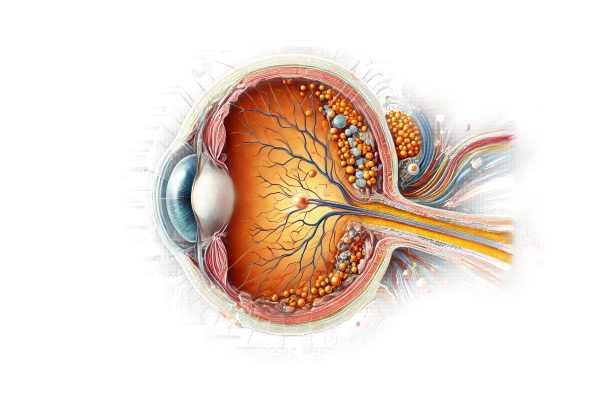
Anatomy and Pathophysiology
The optic nerve, which is made up of nerve fibers that carry visual information from the retina to the brain, is necessary for vision. Glial cells, which support and insulate neurons, can form gliomas. Optic nerve gliomas can affect any part of the optic pathway, such as the optic nerve, chiasm, or optic tract.
Epidemiology
Optic nerve gliomas make up approximately 1-5% of all brain tumors in children. They are most commonly diagnosed in young children, with the peak incidence occurring between ages 2 and 8. The condition has no significant gender bias. A significant proportion of optic nerve gliomas are associated with neurofibromatosis type 1 (NF1), which affects up to 20% of people with the genetic disorder.
Causes and Risk Factors
- Neurofibromatosis Type 1 (NF1): – The most important risk factor for optic nerve glioma is NF1, a genetic disorder caused by mutations in the NF1 gene. This gene normally produces neurofibromin, a protein that regulates cell growth. Mutations in the NF1 gene cause uncontrolled cell proliferation, which raises the risk of tumors, including optic nerve gliomas.
- Genetic Predisposition: – In addition to NF1, other genetic mutations and predispositions can contribute to the development of optic nerve gliomas, but their impact is unclear.
Clinical Presentation
The symptoms of optic nerve glioma vary according to the tumor’s location and size. Common clinical characteristics include:
- Visual Symptoms: – Progressive Vision Loss: Gradual vision loss in one or both eyes is a common symptom. Depending on the location and size of the tumor, this can range from subtle blurring to complete blindness.
- Proptosis: The tumor mass causes the eye to protrude forward.
- Strabismus: Misalignment of the eyes, commonly referred to as a “crossed eye” look.
- Neurological Symptoms: – Headaches: Caused by increased intracranial pressure or tumor mass effect.
- Hormonal Imbalances: If the tumor affects the hypothalamus or pituitary gland, it can cause hormonal imbalances, resulting in symptoms like growth delays or premature puberty.
- Seizures: Seizures are less common, but they can occur if the tumor spreads to adjacent brain areas.
Pathophysiology
Optic nerve gliomas are typically low-grade astrocytomas called pilocytic astrocytomas (WHO Grade I). These tumors form from astrocytes, a type of glial cell, and grow slowly. The presence of these tumors along the optic pathway can cause progressive damage to the optic nerve fibers, resulting in vision loss. Tumors associated with NF1 may be more aggressive and affect multiple segments of the optic pathway.
Complications
If left untreated, optic nerve gliomas can cause a number of complications:
- Severe Vision Loss: Progressive damage to the optic nerve fibers can lead to permanent vision loss.
- Intracranial Pressure: Large tumors can elevate intracranial pressure, resulting in headaches, nausea, and vomiting.
- Hormonal Dysfunction: Tumors of the hypothalamus or pituitary gland can impair hormonal regulation, resulting in a variety of systemic symptoms.
- Neurological Deficits: Depending on the tumor’s location and size, patients may experience a variety of neurological deficits, such as motor and cognitive impairment.
Prognosis
The prognosis for people with optic nerve glioma varies greatly. The tumor’s size, location, growth rate, and association with NF1 all have an impact on prognosis. In general, isolated optic nerve gliomas without NF1 have a better prognosis, with a lower risk of malignant transformation and a better response to therapy. However, gliomas associated with NF1 may be more aggressive and have a higher risk of complications. Early diagnosis and appropriate management are critical for better outcomes.
Diagnosing Optic Nerve Glioma: Tools and Techniques
Diagnosing optic nerve glioma requires a combination of clinical evaluation, imaging studies, and, in some cases, genetic testing to confirm the presence of NF1. Early and accurate diagnosis is critical for effective treatment and monitoring of the condition.
Clinical Evaluation
- Patient History: – A thorough history can identify symptoms like progressive vision loss, proptosis, headaches, and neurological signs. A family history of NF1 or other genetic disorders should also be considered.
- Ophthalmic Examination: – Visual Acuity Test: Detects visual acuity reduction.
- **Fundoscopy: Direct examination of the retina and optic nerve head may reveal signs of papilledema or atrophy.
- Pupil Examination: Looking for an afferent pupillary defect (Marcus Gunn pupil) may indicate optic nerve dysfunction.
Imaging Studies
- MRI is the preferred imaging modality for diagnosing optic nerve gliomas. It provides detailed images of the optic nerve and surrounding structures, allowing for the determination of the tumor’s size, location, and extent. Gadolinium-enhanced MRI can reveal areas with active tumor growth and vascular involvement.
- Computerized Tomography (CT) Scan: CT scans, while less detailed than MRIs, can detect bony changes in the orbit and evaluate tumor calcification. When an MRI is contraindicated or unavailable, CT is frequently used instead.
- Ultrasound: – Orbital ultrasound can help evaluate the optic nerve and detect masses within the orbit.
Genetic Testing
- NF1 Genetic Testing: – Genetic testing can confirm an NF1 diagnosis by identifying mutations in the NF1 gene. This is especially useful for patients with a family history of NF1 or who exhibit multiple symptoms suggestive of the disorder.
Differential Diagnosis
Differentiating optic nerve glioma from other conditions with similar clinical presentations is necessary for accurate diagnosis:
- Optic Neuritis: Inflammation of the optic nerve can cause sudden vision loss and pain with eye movement. MRI and clinical history can help distinguish optic neuritis from optic nerve glioma.
- Orbital Tumors: Other tumors, such as meningiomas or lymphomas, can produce similar symptoms. Imaging studies and, if necessary, biopsy can help differentiate between these conditions.
- Papilledema: Increased intracranial pressure can cause swelling of the optic nerve, giving the appearance of an optic nerve tumor. Neuroimaging and lumbar puncture can help diagnose the underlying cause of papilledema.
Monitoring and Follow-up
Patients with optic nerve glioma must have regular check-ups with ophthalmologists and neurologists to monitor tumor progression and manage symptoms. Periodic imaging studies, visual acuity tests, and comprehensive ophthalmic examinations are critical for monitoring changes and adjusting treatment plans as needed.
Optic Nerve Glioma Treatment
Standard Treatment Options
The size, location, rate of growth, and presence of symptoms all influence the treatment of optic nerve glioma. The primary goals are to preserve vision, relieve symptoms, and prevent tumor progression.
- Observation: – For small, asymptomatic tumors or slow progression, a watch-and-wait approach with regular monitoring through MRI scans and ophthalmic examinations may be advised. This strategy is commonly used for NF1-associated tumors because these gliomas can be indolent.
- Surgery: – Surgical intervention may be necessary for tumors that cause significant vision loss, proptosis, or other complications. Complete resection is difficult due to the delicate nature of the optic nerve and surrounding structures. Partial resection or biopsy may be used to reduce tumor burden or confirm a diagnosis.
- Radiation Therapy: – Radiation therapy is a treatment option for tumors that cannot be surgically removed or have progressed after observation. Conventional fractionated radiation or stereotactic radiosurgery (e.g., Gamma Knife) can be used to target the tumor while minimizing tissue damage. The decision to use radiation therapy, particularly in children, must take into account possible long-term side effects such as cognitive impairment and secondary malignancies.
- Chemotherapy: – Chemotherapy is typically used for younger patients or those with NF1-associated gliomas. Carboplatin and vincristine have been shown to be effective in stabilizing or reducing tumor size. Chemotherapy can be used as a primary treatment or in combination with other modalities to control tumor progression.
Emerging and Innovative Therapeutics
- Targeted Therapies: – Researchers are investigating targeted therapies that block specific molecular pathways that contribute to tumor growth. For example, MEK inhibitors (such as selumetinib) have shown promise in clinical trials for treating NF1-associated optic nerve gliomas by targeting the MAPK/ERK pathway, which is frequently dysregulated in these tumors.
- Immunotherapy: – Immunotherapy, which uses the body’s immune system to fight cancer, is an active research area. Checkpoint inhibitors and other immune-modulating agents are being studied for their ability to treat gliomas, including those that affect the optic pathway.
- Gene Therapy: – Gene therapy aims to correct genetic mutations that cause optic nerve gliomas, especially in NF1 individuals. While still in the experimental phase, these therapies have the potential to provide more effective and less toxic treatments.
- Precision Medicine: – Advances in genetic and molecular profiling of tumors allow for personalized treatment plans tailored to the specific characteristics of gliomas. This approach can improve therapeutic outcomes while minimizing side effects.
Supportive Care
- Vision Rehabilitation: – Patients with significant vision loss can benefit from vision rehabilitation services such as low vision aids, orientation and mobility training, and adaptive techniques to improve their quality of life.
- Psychological Support: – Living with a chronic condition, such as optic nerve glioma, can be challenging for patients and their families. Psychological support and counseling can help with emotional and mental health issues.
Monitoring and Follow-up
Regular follow-up with a multidisciplinary team, which includes ophthalmologists, neurologists, and oncologists, is required to monitor the tumor and manage any complications. Periodic imaging, visual acuity tests, and comprehensive eye exams are essential for monitoring changes and adjusting treatment plans as necessary.
Effective Methods for Improving and Avoiding Optic Nerve Gliomas
- Genetic Counseling: – Genetic counseling can help families with a history of NF1 or other genetic predispositions understand their risk of optic nerve glioma and make informed family planning decisions.
- Early Detection: – Routine eye examinations for children, particularly those with known risk factors like NF1, can detect optic nerve gliomas at an early stage, making them more manageable.
- Maintaining a healthy lifestyle, such as eating a balanced diet with antioxidants, engaging in regular physical activity, and avoiding smoking, can improve overall health and lower the risk of developing tumors.
- Awareness and Education: – Educating parents and healthcare providers on the signs and symptoms of optic nerve glioma can lead to early diagnosis and intervention.
- Regular monitoring is crucial for patients with NF1 to detect changes in the optic nerve and initiate treatment promptly. This includes MRI and ophthalmic exams.
- Stress Management: – Techniques like meditation, yoga, and counseling can improve overall well-being and help the body cope with chronic conditions.
- Limiting exposure to environmental risk factors like radiation and chemicals can reduce the risk of developing tumors.
- Join support groups for patients and families affected by optic nerve glioma or NF1. These groups can offer emotional support, share experiences, and practical advice for managing the condition.
Trusted Resources
Books
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakravarty
- “Neurofibromatosis Type 1: From Diagnosis to Treatment” by Bruce R. Korf and Allan E. Rubenstein
- “Optic Nerve Disorders: Diagnosis and Management” by Jane W. Chan






