What is Lacrimal Duct Obstruction?
Lacrimal duct obstruction, also known as nasolacrimal duct obstruction, is a condition that occurs when the tear drainage system of the eye becomes clogged. This blockage prevents tears from draining properly, resulting in watery eyes, recurring eye infections, and inflammation. Lacrimal duct obstruction can affect both children and adults, with different causes and degrees of severity. Understanding the underlying mechanisms and symptoms is critical to accurate diagnosis and treatment.
Detailed Investigation of Lacrimal Duct Obstruction
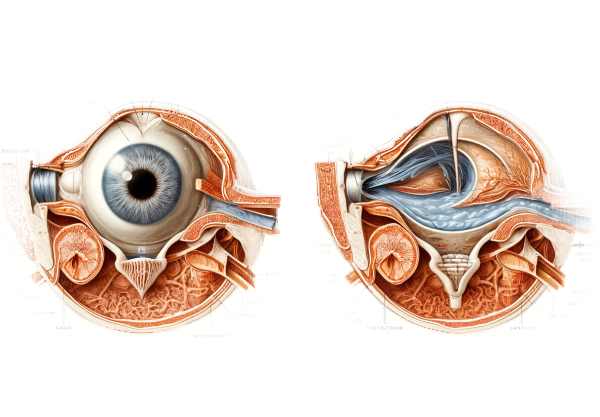
The nasolacrimal duct, which drains tears from the eye into the nasal cavity, becomes clogged with lacrimal duct obstruction. This condition can be congenital or acquired, affecting one or both eyes. The puncta, canaliculi, lacrimal sac, and nasolacrimal duct make up the normal tear drainage system. Any blockage in this pathway can cause the symptoms and complications associated with lacrimal duct obstruction.
Anatomy and Physiology of the Tear Drainage System
The tear drainage system begins with tears produced by the lacrimal glands, which are located above the outer corners of the eyes. Tears flow across the eye’s surface, providing lubrication, nourishment, and protection. Excess tears drain through puncta, which are small openings in the inner corners of the upper and lower eyelids. Tears exit the puncta and travel through tiny canals known as canaliculi before entering the lacrimal sac. The lacrimal sac drains into the nasolacrimal duct, which connects to the nasal cavity.
Types of Lacrimal Duct Obstruction
- Congenital Nasolacrimal Duct Obstruction (CNLDO): This type of obstruction occurs at birth and is most commonly caused by an incomplete nasolacrimal duct opening. CNLDO affects about 5-10% of newborns, but most cases resolve spontaneously within the first year of life.
- Acquired Nasolacrimal Duct Obstruction: This form appears later in life and can be caused by a variety of factors such as chronic inflammation, infection, trauma, or aging. Adults are more likely to develop acquired obstruction, which can be classified as primary or secondary.
• Primary Acquired Nasolacrimal Duct Obstruction (PANDO): This type is frequently idiopathic, meaning it occurs without apparent cause but is associated with age-related narrowing of the nasolacrimal duct.
- Secondary Acquired Nasolacrimal Duct Obstruction (SANDO): External factors affecting the lacrimal system, such as infections, injuries, tumors, or systemic diseases, cause this type.
Symptoms
The symptoms of lacrimal duct obstruction vary according to the severity and cause of the blockage. Common symptoms include:
- Epiphora (Excessive Tearing): Tears overflow onto the face rather than draining into the nasolacrimal duct.
- Recurrent Eye Infections: Stagnant tears can provide a breeding ground for bacteria, causing frequent infections such as conjunctivitis or dacryocystitis (lacrimal sac infection).
- Discharge: Mucous or pus-like discharge from the eye may indicate infection or inflammation.
- Redness and Swelling: Inflammation of the inner corner of the eye or the lacrimal sac area can result in redness and swelling.
- Pain and Discomfort: Blockage and infection may cause discomfort or pain in the affected area.
Pathophysiology
The pathophysiology of lacrimal duct obstruction involves the disruption of normal tear drainage, resulting in tear stasis and subsequent complications. In most congenital cases, the obstruction is caused by a membrane at the distal end of the nasolacrimal duct that fails to open. Chronic inflammation, infections, trauma, or neoplastic processes can all cause structural changes or scarring within the duct, resulting in an obstruction.
Complications
Untreated lacrimal duct obstruction can cause a variety of complications, including
- Chronic Dacryocystitis is a persistent infection of the lacrimal sac that causes pain, swelling, and purulent discharge.
- Acute Dacryocystitis: A severe, painful infection that can spread to adjacent tissues, resulting in cellulitis or abscess formation.
- Mucocele: Mucus accumulation within the lacrimal sac as a result of chronic obstruction, causing swelling and potential rupture.
- Keratitis: Corneal inflammation caused by persistent tearing and infection that compromises the protective function of the tear film.
- Orbital Cellulitis: A rare but serious complication in which infection spreads to the tissues surrounding the eye, potentially resulting in vision loss if not treated immediately.
Epidemiology
Lacrimal duct obstruction affects people of all ages, and the prevalence varies depending on the type of obstruction. Congenital nasolacrimal duct obstruction is relatively common, affecting 5-10% of newborns, and it often resolves spontaneously. Acquired obstruction is more common in adults, especially those over the age of 50. Women are more likely to suffer from acquired obstruction, possibly due to hormonal influences and narrower nasolacrimal ducts.
Risk Factors
Several factors can raise the risk of developing lacrimal duct obstruction.
- Age: Older adults are more likely to develop obstructions due to age-related changes in the lacrimal system.
- Gender: Women have a higher risk of PANDO.
- Chronic Sinusitis: Inflammation in the nasal passages can spread to the nasolacrimal duct, causing obstruction.
- Facial Trauma: Injuries to the face or nose can impair the lacrimal drainage system.
- Systemic Diseases: Sarcoidosis, Wegener’s granulomatosis, and certain infections can all affect the lacrimal ducts.
Approaches for Diagnosing Lacrimal Duct Obstruction
Lacrimal duct obstruction requires a thorough examination by an eye care professional. A detailed history, clinical examination, and a variety of diagnostic tests are used to determine the location and cause of the obstruction.
Clinical Examination
- History and Symptom Assessment: The evaluation begins with a thorough history to determine the patient’s symptoms, duration, and previous treatments or surgeries. Questions about the frequency and nature of tearing, discharge, and infections are critical.
- External Examination: The eyelids, puncta, and periorbital area are examined for signs of swelling, redness, or discharge. Gentle palpation of the lacrimal sac area can reveal tenderness or pus expression, which indicate infection.
Diagnostic Tests
- The Fluorescein Dye Disappearance Test (FDDT): A small amount of fluorescein dye is injected into the conjunctival sac, and the tear film is examined using a cobalt blue light. Within 5-10 minutes of normal tear drainage, the dye should have disappeared. The dye’s persistence indicates that there may be an obstruction.
- Primary Dye Test (Jones Test I): Fluorescein dye is instilled into the eye, and a cotton-tipped applicator is inserted into the same nostril. The presence of dye on the applicator is indicative of a patent nasolacrimal duct.
- Secondary Dye Test (Jones Test II): If the primary dye test is negative, saline is irrigated into the nasolacrimal duct, and the patient is instructed to blow their nose. The presence of fluorescein-stained saline indicates a partial obstruction or narrowing of the duct.
- Nasolacrimal Duct Irrigation: A small cannula injects a saline solution through the puncta. Difficulty irrigating or refluxing fluid through the opposite punctum indicates an obstruction.
Imaging Studies
- Dacryocystography (DCG): This imaging technique involves injecting a contrast medium into the lacrimal drainage system and then imaging with X-rays. DCG aids in the visualization of the anatomy and determining the location and extent of the obstruction.
- Dacryoscintigraphy: A gamma camera tracks the passage of a radioactive tracer through the lacrimal system. This method provides dynamic data on tear drainage.
- Computed Tomography (CT) and Magnetic Resonance Imaging (MRI): These imaging modalities can evaluate the surrounding structures and detect any anatomical abnormalities, tumors, or inflammation of the lacrimal system.
- Endoscopic Examination: Nasal endoscopy provides direct visualization of the nasolacrimal duct opening in the nasal cavity. It is especially useful in detecting anatomical obstructions or inflammation near the duct’s distal end.
Lacrimal Duct Obstruction Treatment
The goal of treating lacrimal duct obstruction is to restore normal tear drainage, relieve symptoms, and avoid complications like infections. Treatment options vary according to the cause, severity, and patient age. Here, we look at both traditional and novel treatments for lacrimal duct obstruction.
Conservative Treatments
- Observation: In infants with congenital nasolacrimal duct obstruction, spontaneous resolution usually occurs within the first year of life. Regular monitoring is necessary to ensure that the condition improves naturally and without complications.
- Massage: In congenital cases, a gentle massage of the lacrimal sac (Crigler massage) can aid in opening the nasolacrimal duct. This technique entails applying gentle pressure to the area between the eyes and the nose several times daily.
- Antibiotics: If an associated infection, such as dacryocystitis, exists, topical or systemic antibiotics may be prescribed. Antibiotic eye drops and oral antibiotics can help treat the infection and reduce inflammation.
Minimal Invasive Procedures
- Dilation and Probing: This is a common procedure for children with congenital obstruction. A thin probe is inserted through the punctum and canaliculi to clear the clogged nasolacrimal duct. Before probing, the tear duct opening may be dilatable.
- Balloon Catheter Dilation: A small balloon catheter is inserted into the nasolacrimal duct and inflated to relieve the obstruction. This technique is frequently used when initial probing fails or for recurring obstructions.
- Stent or Intubation: A silicone tube or stent is temporarily inserted into the nasolacrimal duct to keep it open. This procedure is most commonly used when probing and dilation are insufficient.
Surgical Treatments
- Dacryocystorhinostomy (DCR): This is the most commonly performed surgical procedure for treating lacrimal duct obstruction, especially in adults. DCR opens a new drainage path between the lacrimal sac and the nasal cavity, bypassing the clogged nasolacrimal duct. Endoscopically (through the nasal passage) or externally (through a small incision on the side of the nose). Endoscopic DCR is less invasive and doesn’t leave an external scar.
- Conjunctivodacryocystorhinostomy (CDCR): When the upper and lower canaliculi become clogged, CDCR involves creating a new drainage channel from the conjunctiva to the nasal cavity with a glass tube (Jones tube).
Innovative and Emerging Therapies
- Laser-Assisted Dacryocystorhinostomy: This minimally invasive technique in DCR surgery creates a new tear drainage pathway using a laser. The laser’s precision minimizes tissue trauma and promotes faster healing.
- Microendoscopic Surgery: Advanced microendoscopic techniques enable precise visualization and treatment of the lacrimal drainage system. This method increases the accuracy of procedures such as DCR and stenting.
- Drug-Eluting Stents: New research looks into the use of drug-eluting stents, which release anti-inflammatory or antimicrobial agents to prevent infection and promote healing during stent placement.
- Gene Therapy and Regenerative Medicine: Investigational therapies seek to address the genetic causes of congenital obstructions and promote the regeneration of lacrimal duct tissue. These innovative approaches show promise for long-term solutions.
By combining established and innovative treatments, healthcare providers can effectively manage lacrimal duct obstruction and improve patients’ quality of life.
Effective Ways to Improve and Prevent Lacrimal Duct Obstruction
- Maintain Eye Hygiene: Always wash your hands before touching your face or eyes. Avoid sharing towels and personal items that may come into contact with your eyes.
- Proper Contact Lens Care: Clean and disinfect contact lenses on a regular basis, and adhere to the recommended guidelines for use. Unless specifically prescribed, avoid wearing contact lenses while sleeping.
- Manage Allergies: Treat allergies right away to avoid eye irritation and inflammation, which can lead to lacrimal duct blockage.
- Protect Your Eyes: Wear protective eyewear when participating in activities that increase the risk of eye injury, such as sports or working with hazardous materials.
- Avoid Smoking: Smoking can irritate the eyes and cause chronic inflammation, which raises the risk of lacrimal duct obstruction.
- Stay Hydrated: Stay hydrated to maintain good eye health and tear production.
- Treat Sinus Infections: Treat sinus infections right away to prevent inflammation from spreading to the lacrimal ducts.
- Regular Eye Exams: Have regular eye exams to detect early signs of lacrimal duct obstruction and other ocular conditions.
- Avoid Eye Rubbing: Do not rub your eyes, especially if they are irritated or inflamed, as this can worsen blockage and infection.
- Use Humidifiers: In dry areas, use a humidifier to keep moisture in the air and prevent dryness of the eyes and nasal passages.
Trusted Resources
Books
- “Diseases of the Lacrimal System” by John D. Dartt
- “Principles and Practice of Lacrimal Surgery” by Mohammad Javed Ali






