What is lagophthalmos?
Lagophthalmos is an ocular condition that causes the eyelids to remain partially closed. This incomplete closure can expose the cornea and conjunctiva, causing dryness, irritation, and potentially damaging the eye. Lagophthalmos can result from a variety of underlying causes, including facial nerve paralysis, trauma, or congenital defects. Early detection and appropriate management are critical for avoiding complications and maintaining ocular health.
Detailed Study of Lagophthalmos
Lagophthalmos is a condition that impairs the normal function of the eyelids, particularly their ability to completely close. The term comes from the Greek words “lagos,” meaning hare, and “ophthalmos,” meaning eye, because hares frequently sleep with their eyes partially open. Understanding the anatomy, causes, symptoms, and complications associated with lagophthalmos is critical for accurate diagnosis and treatment.
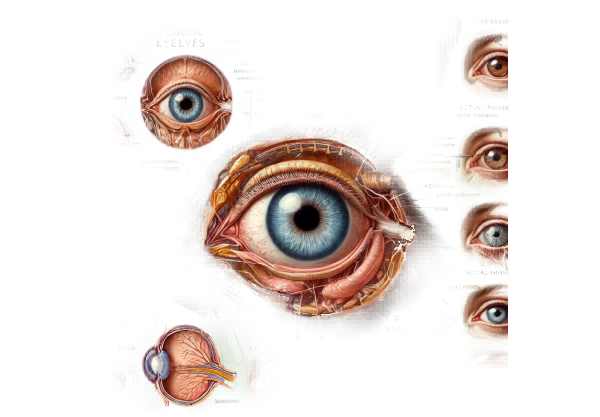
Structure and Function of the Eyelids
The eyelids are essential for protecting the eyes and maintaining ocular health. They serve as a barrier against foreign bodies, evenly distribute the tear film across the surface of the eye, and aid in the removal of debris through blinking. The main muscles involved in eyelid movement are the orbicularis oculi, which helps with eyelid closure, and the levator palpebrae superioris, which helps with eyelid elevation.
Causes of Lagophthalmos
Lagophthalmos can be caused by a variety of factors, which are broadly classified as neurogenic, mechanical, or myogenic.
Neurogenic Causes
- Facial Nerve Paralysis (Bell’s Palsy) is the most common cause of lagophthalmos. It affects the muscles that control eyelid closure. Bell’s palsy, a sudden onset of facial paralysis, frequently causes lagophthalmos on the affected side.
- Stroke: A cerebrovascular accident or stroke can injure the facial nerve or its central pathways, causing lagophthalmos.
- Neuromuscular Disorders: Conditions like myasthenia gravis can impair the function of the muscles and nerves that control eyelid closure, resulting in lagophthalmos.
Mechanical Causes
- Eyelid Scarring (Cicatricial Lagophthalmos): Trauma, burns, or surgery can all result in scarring of the eyelid tissues, preventing complete closure.
- Proptosis: Conditions that cause the eyeball to protrude, such as Graves’ disease or orbital tumors, can mechanically prevent eyelid closure, resulting in lagophthalmos.
- Eyelid Malpositions: Ectropion (outward turning of the eyelid) and entropion (inward turning of the eyelid) can impair normal eyelid function and cause lagophthalmos.
Myogenic Causes
- Muscle Weakness: Aging and systemic diseases like muscular dystrophy can weaken the muscles that control eyelid closure, resulting in lagophthalmos.
- Congenital Defects: Some people are born with abnormalities in their eyelid muscles or structures, resulting in lagophthalmos from birth.
Symptoms of Lagophthalmos
The inability to fully close the eyelids can cause a variety of symptoms, primarily due to exposure of the cornea and conjunctiva. Common symptoms include:
- Dryness and Irritation: The exposed ocular surface may become dry and irritated, resulting in discomfort and redness.
- Excessive Tearing (Epiphora): When exposed to dryness, the lacrimal glands may produce excessive tears, resulting in persistent tearing.
- Foreign Body Sensation: Patients frequently report feeling grit or sand in their eyes as a result of exposure and irritation.
- Blurred Vision: Chronic dryness and irritation can damage the tear film, causing intermittent blurred vision.
- Redness and Inflammation: Prolonged exposure may cause inflammation of the conjunctiva (conjunctivitis) and cornea (keratitis).
Complications of Lagophthalmos
If left untreated, lagophthalmos can cause a number of serious complications, including:
- Exposure Keratopathy: Prolonged exposure to the cornea can cause keratopathy, which is characterized by epithelial breakdown, corneal ulcers, and potential vision loss.
- Corneal Ulceration: Severe dryness and exposure can result in painful corneal ulcers, scarring, and vision impairment.
- Infection: The compromised ocular surface is more prone to bacterial, viral, and fungal infections.
- Vision Loss: If not properly managed, persistent corneal damage and scarring can lead to permanent vision loss.
- Cosmetic Concerns: The inability to fully close the eyes can cause cosmetic issues such as asymmetric eyelid appearance and visible corneal exposure.
Pathophysiology
The pathophysiology of lagophthalmos includes disruptions in the normal anatomy and function of the eyelids. The facial nerve innervates the orbicularis oculi muscle, which is important for eyelid closure. When the facial nerve is damaged, as in Bell’s palsy or a stroke, the muscle’s ability to contract is compromised, resulting in incomplete eyelid closure. Mechanical factors such as scarring, proptosis, or eyelid malposition physically keep the eyelids apart, whereas myogenic factors such as muscle weakness or congenital defects have a direct impact on muscle function.
Epidemiology
Lagophthalmos is a condition that can affect people of any age or background. It is commonly associated with facial nerve paralysis, which affects around 40,000 Americans each year. The prevalence of lagophthalmos rises with age, owing to age-related muscle weakness and systemic diseases. This condition affects both males and females equally.
Risk Factors
Several factors can raise the risk of developing lagophthalmos.
- Facial Nerve Injury: Any condition or event that can harm the facial nerve, such as Bell’s palsy, a stroke, or trauma, raises the risk.
- Ocular Surface Disorders: Pre-existing conditions such as dry eye disease or conjunctivitis can worsen the symptoms of lagophthalmos.
- Systemic Diseases: Diabetes, which can cause nerve damage, and autoimmune diseases such as myasthenia gravis raise the risk.
- Surgical History: Previous surgeries on the eyelids or orbit can cause scarring and subsequent lagophthalmos.
- Thyroid Eye Disease: Patients with thyroid eye disease frequently develop proptosis, which raises the risk of lagophthalmos.
Understanding the specific anatomy, causes, symptoms, and potential complications of lagophthalmos is essential for accurate diagnosis and treatment. Early intervention can prevent serious complications and maintain ocular health.
Diagnostic methods
A thorough clinical evaluation, including patient history, physical examination, and specialized tests to assess eyelid function and ocular surface health, is required to diagnose lagophthalmos. Accurate diagnosis is critical for determining the best treatment and avoiding complications.
Clinical Examination
- Patient History: A complete patient history is essential for determining the onset, duration, and progression of symptoms. The key questions include:
- When did the symptoms begin?
- Are there any related conditions, such as facial nerve paralysis or thyroid eye disease?
- Has there been any recent surgery or trauma?
- What symptoms are you experiencing (e.g., dryness, tearing, blurred vision)?
- Visual Inspection: The clinician will thoroughly examine the eyes and eyelids for signs of incomplete closure, swelling, redness, and any visible corneal exposure. Observing the blink reflex and the ability to completely close the eyes is critical.
- Palpation and Assessment: Gently palpating the eyelids can aid in determining muscle tone and the presence of scarring or deformities. The clinician may also look for proptosis and other anatomical abnormalities.
Specialized Tests
- Slit-Lamp Examination: A slit-lamp examination provides a thorough evaluation of the ocular surface, including the cornea, conjunctiva, and tear film. This test detects signs of dryness, inflammation, and epithelial defects.
- Fluorescein Staining: A fluorescein dye is applied to the ocular surface to highlight epithelial damage or dryness. Under blue light, the dye illuminates damaged areas, revealing the full extent of exposure keratopathy.
- Schirmer Test: To measure tear production, place a small strip of filter paper under the lower eyelid. The amount of moisture absorbed by the paper over a given time period indicates tear production levels, which aids in diagnosing dry eye caused by lagophthalmos.
- Blink Reflex Assessment: Evaluating the blink reflex and frequency of blinking can reveal information about eyelid function and lagophthalmos. Reduced blink rate or incomplete blinking can worsen symptoms.
Imaging Studies
- MRI or CT Scans: When neurogenic causes, such as facial nerve paralysis, are suspected, imaging studies such as MRI or CT scans of the brain and orbit may be conducted. These tests help to determine the underlying cause of nerve damage or structural abnormalities.
- Ultrasound: High-frequency ultrasound can visualize the eyelid structures and lacrimal gland, allowing for the assessment of any anatomical changes or abnormalities that contribute to lagophthalmos.
Lagophthalmos Treatment
The treatment for lagophthalmos focuses on identifying the underlying cause, protecting the ocular surface, and improving eyelid closure. The severity of the condition, the underlying cause, and the presence of any complications all influence treatment decisions. The following are the available treatment options, as well as some innovative and emerging therapies.
Conservative Treatments
- Artificial Tears and Lubricating Ointments: Regular use of artificial tears can help keep the eyes moist and prevent dryness. Lubricating ointments, particularly those used at night, provide the cornea with long-lasting moisture and protection.
- Moisture Chambers: Wearing moisture chamber goggles or patches while sleeping creates a humid environment around the eye, reducing evaporation and keeping the ocular surface hydrated.
- Taping the Eyelids: Taping the eyelids closed can provide temporary relief, particularly during sleep, by preventing exposure and protecting the cornea from drying.
Medical Treatments
- Botulinum Toxin (Botox) Injections: In cases of temporary facial nerve paralysis, Botox injections can be used to temporarily paralyze the levator palpebrae superioris muscle, allowing the eyelid to remain closed.
- Anti-Inflammatory Medications: Topical corticosteroids or non-steroidal anti-inflammatory drugs (NSAIDs) can be used to reduce inflammation on the ocular surface and relieve symptoms.
Surgical Treatments
- Tarsorrhaphy is a surgical procedure in which the eyelids are partially or completely sewn together to reduce the size of the palpebral fissure and protect the cornea. Temporary tarsorrhaphy can be used for short-term protection, whereas permanent tarsorrhaphy is recommended for more severe or chronic cases.
- Gold or Platinum Weight Implants: Inserting a small gold or platinum weight into the upper eyelid can assist gravity in closing the eyelid. This procedure is especially effective in cases of facial nerve paralysis.
- Lateral Canthoplasty: This procedure tightens the lower eyelid by shortening the lateral canthal tendon, increasing support and reducing lagophthalmos. It is frequently combined with other surgical techniques for the best results.
- Eyelid Reconstruction: Patients with severe scarring or deformities may require reconstructive surgery to restore normal eyelid anatomy and function.
Innovative and Emerging Therapies
- Stem Cell Therapy: Studies on stem cell therapy for ocular surface reconstruction show promise for treating lagophthalmos. Stem cells have the potential to regenerate damaged tissues and restore eyelid function.
- Gene Therapy: Gene therapy seeks to correct genetic abnormalities that cause nerve or muscle dysfunction. Although still in the experimental stage, this approach has the potential to provide a long-term solution to neurogenic lagophthalmos.
- Minimally Invasive Procedures: Improvements in minimally invasive surgical techniques, such as endoscopic procedures, provide less traumatic alternatives to traditional surgeries. These techniques aim to improve outcomes while shortening recovery times.
- Neurostimulation Devices: Researchers are investigating emerging neurostimulation devices capable of stimulating or mimicking the function of the facial nerve. These devices may help restore eyelid movement and improve closure.
By combining traditional treatments with innovative therapies, healthcare providers can provide a comprehensive approach to lagophthalmos management that is tailored to the specific needs of each patient. Early intervention and appropriate management are critical for avoiding complications and maintaining good ocular health.
Effective Methods for Improving and Avoiding Lagophthalmos
- Protect Your Eyes: Wear protective eyewear when participating in activities that pose a risk of facial or ocular trauma, such as sports or construction work, to avoid injuries that could result in lagophthalmos.
- Maintain Good Eye Hygiene: Keep your eyelids and surrounding area clean to avoid infections that can worsen lagophthalmos. Use gentle cleansers and refrain from rubbing your eyes.
- Manage Underlying Conditions: If you have Bell’s palsy or thyroid eye disease, stick to your treatment plan to minimize your risk of developing lagophthalmos.
- Use Humidifiers: In dry environments, use a humidifier to keep the air moist, which can help prevent dry eyes and lower the risk of complications from lagophthalmos.
- Stay Hydrated: Drink plenty of water to keep your skin and eyes hydrated. Proper hydration is essential for keeping a healthy tear film and avoiding dryness.
- Regular Eye Examinations: Have regular eye exams to monitor your ocular health and detect early signs of lagophthalmos or other eye conditions. Early detection enables prompt intervention and management.
- Avoid Excessive Eye Rubbing: Do not vigorously rub your eyes, as this can cause eyelid trauma and worsen lagophthalmos symptoms.
- Follow Post-Surgical Care Instructions: If you have surgery for any reason, follow your postoperative care instructions carefully to ensure proper healing and avoid complications like lagophthalmos.
- Use Lubricating Eye Drops: Applying lubricating eye drops on a regular basis can help keep the ocular surface moist and reduce symptoms of dryness and irritation caused by lagophthalmos.
- Protect Your Eyes from Wind and Sun: When going outside, wear UV-protected sunglasses to protect your eyes from wind and sun exposure, which can exacerbate dryness and irritation.
Individuals who follow these preventive measures and tips can lower their risk of developing lagophthalmos while also improving their overall eye health.
Trusted Resources
Books
- “Diseases of the Lacrimal System” by John D. Dartt
- “Principles and Practice of Lacrimal Surgery” by Mohammad Javed Ali






