Hypertensive retinopathy is a potentially vision-threatening condition caused by chronic high blood pressure damaging the delicate blood vessels in the retina—the light-sensitive tissue at the back of the eye. It often develops silently, but can signal both advanced eye disease and systemic cardiovascular risk. Early detection and proper management are essential for protecting eyesight and overall health. In this comprehensive guide, we’ll explore the science behind hypertensive retinopathy, established treatments, surgical options for severe cases, and the latest breakthroughs reshaping care and prevention—empowering you with practical knowledge to safeguard your vision and well-being.
Table of Contents
- Understanding Hypertensive Retinopathy and Its Prevalence
- Established Medical Therapies and Pharmacological Management
- Surgical and Interventional Procedures for Severe Cases
- Emerging Innovations and Advanced Technologies in Care
- Clinical Trials and Future Directions in Treatment
- Frequently Asked Questions
- Disclaimer
Understanding Hypertensive Retinopathy and Its Prevalence
Hypertensive retinopathy is a spectrum of changes seen in the retina as a direct result of persistently elevated blood pressure. The retina’s tiny arteries and veins are particularly vulnerable to chronic hypertension, which leads to narrowing, leakage, and even blockage of these vessels.
Pathophysiology: How High Blood Pressure Affects the Retina
- Vasoconstriction: Initial response of retinal arterioles to high pressure is narrowing (vasoconstriction), reducing blood flow.
- Vascular Damage: Ongoing pressure damages the vessel walls, causing leakage of fluid, blood, or fat (lipid) into the retinal layers.
- Ischemia and Infarcts: In advanced cases, parts of the retina may become deprived of blood (ischemic), leading to small strokes or swelling of the optic nerve.
Staging and Clinical Signs
- Mild: Subtle arteriolar narrowing, increased light reflex (“copper wiring”).
- Moderate: Hemorrhages, cotton wool spots (nerve fiber infarcts), hard exudates (lipid leakage), and microaneurysms.
- Severe/Malignant: Swelling of the optic disc (papilledema), widespread hemorrhages, and risk of sudden vision loss.
Prevalence and At-Risk Groups
- Hypertensive retinopathy can develop in anyone with long-standing, poorly controlled high blood pressure.
- Prevalence increases with age, duration of hypertension, and severity of blood pressure elevation.
- Coexisting diabetes, kidney disease, or other vascular conditions amplify risk and progression.
Symptoms and Detection
- Early stages are often symptom-free; many cases are found during routine eye exams.
- Blurred vision, sudden vision changes, or visual field defects may occur in advanced stages.
Risk Factors Beyond Blood Pressure
- Smoking, obesity, high cholesterol, and a sedentary lifestyle all worsen risk.
- Certain ethnic groups and those with a family history of hypertension are more susceptible.
Real-World Prevention Tips
- Regular blood pressure checks and eye exams—especially if you have hypertension or other cardiovascular risk factors.
- Adopt a heart-healthy lifestyle: reduce salt, exercise, manage weight, and avoid smoking.
Hypertensive retinopathy is both a warning sign and a call to action—for eye health and for cardiovascular protection.
Established Medical Therapies and Pharmacological Management
The backbone of hypertensive retinopathy treatment is optimal blood pressure control—both to halt progression and to prevent sight-threatening complications. Additional therapies target secondary issues within the eye.
Blood Pressure Management: The Foundation
- Antihypertensive Medications:
ACE inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, calcium channel blockers, and diuretics are tailored to individual health profiles. Consistent use and close monitoring are vital. - Lifestyle Modification:
- Dietary changes (DASH or Mediterranean diets)
- Regular physical activity
- Smoking cessation
- Weight management
- Limiting alcohol and sodium
Retinal-Specific Medical Management
- Observation and Monitoring:
In mild cases with stable blood pressure, regular eye exams track changes and guide management. - Treatment of Macular Edema or Retinal Swelling:
- Intravitreal anti-VEGF injections (e.g., ranibizumab, aflibercept) may be used if swelling threatens central vision.
- Steroid injections in select cases of inflammation-related swelling.
Adjunct Therapies
- Management of Associated Conditions:
Control of diabetes, high cholesterol, and kidney disease reduces cumulative retinal risk. - Nutritional Support:
Diets rich in antioxidants, omega-3s, and leafy greens may support overall retinal health.
Practical Home Advice
- Maintain a daily log of blood pressure readings.
- Take medications at the same time each day to form a healthy habit.
- Use home blood pressure cuffs and mobile apps for real-time tracking.
When to Seek Urgent Help
- Sudden or severe vision loss
- Visual field defects, flashing lights, or floaters
- Eye pain or redness in the context of hypertension
Early and aggressive management of systemic blood pressure is the single most important step for protecting vision in hypertensive retinopathy.
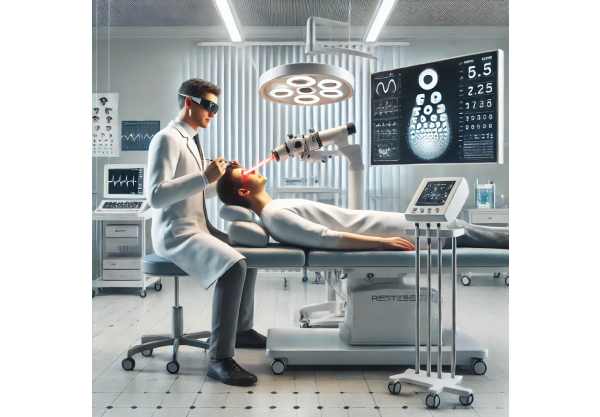
Surgical and Interventional Procedures for Severe Cases
While most cases are managed medically, severe hypertensive retinopathy with complications such as retinal vein occlusion, persistent macular edema, or non-resolving hemorrhages may require surgical or procedural intervention.
Key Surgical and Interventional Approaches
- Intravitreal Injections:
- Anti-VEGF drugs for macular edema or neovascularization.
- Corticosteroids for inflammatory complications.
- Laser Photocoagulation:
- Focal or grid laser may seal leaking blood vessels or reduce swelling in chronic macular edema.
- Pan-retinal photocoagulation (PRP) in eyes with widespread ischemia or abnormal vessel growth.
Vitrectomy Surgery
- Pars Plana Vitrectomy:
- Removes blood or scar tissue from the vitreous cavity in cases of non-clearing vitreous hemorrhage or severe retinal traction.
- Allows direct repair of retinal detachment or macular holes.
Management of Retinal Vascular Occlusions
- Thrombolytic Therapy:
- Rarely, direct injection of clot-busting medication may be attempted for acute vein or artery occlusion, though evidence remains limited.
- Retinal Vein Decompression Procedures:
- Experimental surgeries to relieve pressure in blocked veins, primarily in research settings.
Adjunctive Procedures
- Anti-inflammatory and Neuroprotective Interventions:
Research into retinal implants and neuroprotective drugs is ongoing for irreversible ischemic injury.
Recovery and Aftercare Tips
- Avoid strenuous activity or heavy lifting for at least several days after procedures.
- Adhere to post-procedure drop regimens and follow-up appointments.
- Monitor for signs of infection or sudden vision loss.
Prompt recognition and treatment of severe retinal complications can preserve vision, even in advanced hypertensive retinopathy.
Emerging Innovations and Advanced Technologies in Care
Cutting-edge research is transforming the management of hypertensive retinopathy, with the goal of earlier detection, better risk stratification, and safer, more effective treatments.
AI-Powered Screening and Diagnosis
- Automated Retinal Imaging:
Artificial intelligence is being used to analyze retinal photographs, detect early microvascular changes, and predict progression with remarkable accuracy. - Teleophthalmology:
Remote eye exams are making early detection more accessible, especially in underserved areas.
Next-Generation Drug Delivery
- Sustained-Release Implants:
Tiny, slow-release devices deliver anti-VEGF or steroid medication over months, reducing the need for frequent injections. - Gene and Cell Therapies:
In early clinical trials, aimed at repairing or replacing damaged retinal cells and restoring lost vision in severe cases.
Personalized Medicine Approaches
- Risk Profiling:
Use of genetic, proteomic, and imaging data to personalize treatment intensity and frequency. - Machine Learning for Prognosis:
Predictive models help identify patients most likely to benefit from aggressive therapy or close monitoring.
Home-Based and Wearable Technologies
- Retinal Function Apps:
Smartphone-based tests allow patients to monitor vision changes at home and alert doctors to early signs of deterioration. - Blood Pressure Wearables:
Smartwatches and wireless cuffs help patients maintain better BP control—critical for both eye and overall health.
Practical Steps to Embrace Innovation
- Ask your eye doctor if your clinic uses AI screening or advanced imaging.
- Consider enrolling in clinical trials if you have advanced disease or are interested in cutting-edge therapies.
- Use available home tools for blood pressure and vision tracking.
These innovations aim to catch retinopathy earlier, treat it more effectively, and improve the lives of those living with high blood pressure.
Clinical Trials and Future Directions in Treatment
Ongoing research is focused on halting and even reversing the effects of hypertensive retinopathy, using a blend of pharmaceutical, technological, and surgical advances.
Active and Upcoming Clinical Trials
- Novel Drug Therapies:
Testing new classes of anti-angiogenic, anti-inflammatory, and neuroprotective drugs designed to minimize retinal injury and preserve vision. - Advanced Laser and Implant Devices:
Development of less-damaging, more targeted laser treatments and longer-lasting drug delivery implants. - Gene Editing and Regenerative Medicine:
Exploring CRISPR and stem cell approaches to repair damaged retinal blood vessels and neurons.
Research Priorities and Trends
- Early Detection:
Using AI and digital biomarkers for population screening. - Integrated Cardiovascular-Eye Health Programs:
Combining medical, lifestyle, and digital interventions to reduce both eye and heart disease risks. - Patient-Centered Care:
Engaging patients in self-monitoring, shared decision-making, and home-based care.
How to Stay Informed and Involved
- Join patient registries or advocacy groups focused on retinal and vascular eye health.
- Subscribe to newsletters from major eye research institutions for clinical trial opportunities.
- Participate in surveys or trials if you meet eligibility criteria.
Looking ahead, the convergence of technology, personalized care, and patient empowerment promises even better outcomes for those with hypertensive retinopathy.
Frequently Asked Questions
What is hypertensive retinopathy and how does it affect vision?
Hypertensive retinopathy refers to damage in the retina caused by high blood pressure, which can lead to vision changes, blurred vision, or, in severe cases, permanent vision loss if left untreated.
How is hypertensive retinopathy diagnosed?
Diagnosis involves a comprehensive eye exam, including retinal imaging and dilation. Eye doctors look for characteristic vessel changes, hemorrhages, or swelling that signal blood pressure-related injury.
What are the best treatments for hypertensive retinopathy?
Optimal blood pressure control is crucial. Additional treatments, such as anti-VEGF injections or laser therapy, may be used for complications like macular edema or retinal hemorrhage.
Can hypertensive retinopathy be reversed?
Early changes can often be halted or improved with strict blood pressure control. However, advanced damage—especially to retinal nerves or the optic disc—may be permanent.
What lifestyle changes help manage hypertensive retinopathy?
Adopting a low-sodium, heart-healthy diet, regular exercise, quitting smoking, and managing stress are all essential for controlling blood pressure and protecting vision.
When should I see a doctor about vision changes?
See an eye doctor promptly if you have high blood pressure and notice new visual symptoms, such as blurred vision, floaters, or vision loss. Early care makes a difference.
Are there new treatments for hypertensive retinopathy?
Yes, new options include long-acting drug implants, gene and cell therapies, and AI-powered monitoring tools. Ask your provider about the latest advancements.
Disclaimer
This article is for informational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider with any questions or concerns about your vision or blood pressure.
If you found this guide useful, please share it on Facebook, X (formerly Twitter), or your favorite platform. Your support helps us continue creating high-quality, accessible health resources. Follow us for the latest in eye health and disease prevention—thank you for helping others stay informed and healthy!






