Basal cell carcinoma (BCC) of the eyelid is the most frequent malignant tumor affecting the eyelids, responsible for over 90% of all eyelid cancers. While it rarely spreads to distant sites, BCC can be locally aggressive, threatening both vision and ocular structures if not managed promptly and appropriately. Early detection is critical, as eyelid BCC often presents as a painless, slow-growing lesion that can mimic benign conditions. This comprehensive guide explores the causes, risk factors, diagnostic methods, and a full spectrum of modern and emerging treatments, equipping patients and clinicians with current knowledge and practical steps for optimal care and outcomes.
Table of Contents
- Understanding Basal Cell Carcinoma of the Eyelid
- Standard Non-Surgical and Medical Therapies
- Operative Techniques and Local Interventions
- Cutting-Edge Innovations and Technological Advances
- Clinical Research and Future Directions
- Frequently Asked Questions
Understanding Basal Cell Carcinoma of the Eyelid
Basal cell carcinoma (BCC) of the eyelid is a malignant tumor originating from the basal cells in the epidermis. Unlike more aggressive skin cancers, BCC grows slowly and seldom metastasizes. However, its location near vital ocular structures makes early identification and management essential to prevent functional and cosmetic impairment.
Key Features and Pathophysiology:
- BCC most often develops on the lower eyelid (approximately 50–60%), followed by the medial canthus, upper eyelid, and lateral canthus.
- Sun exposure is the primary risk factor, especially in fair-skinned individuals.
- Other contributing factors include chronic inflammation, prior radiation, genetic syndromes (like basal cell nevus syndrome), and immunosuppression.
Common Clinical Presentations:
- Pearly, waxy nodule with telangiectasia (visible small blood vessels)
- Ulceration, crusting, or non-healing sore
- Loss of eyelashes (madarosis) if tumor affects the lid margin
- Scar-like (sclerosing/morpheaform) or pigmented forms can be mistaken for benign lesions
Epidemiology:
- BCC accounts for more than 90% of all eyelid malignancies
- Predominantly affects adults over 50, but younger cases do occur
- Slightly more common in men than women
Risk Factors:
- Cumulative ultraviolet (UV) light exposure, especially without sun protection
- Fair skin, light eyes, and hair
- History of previous skin cancers
- Genetic predisposition (e.g., xeroderma pigmentosum)
Diagnosis:
- Clinical examination with slit lamp or dermoscopy
- Biopsy (usually excisional or incisional) is required for definitive diagnosis
- Imaging (MRI or CT) may be used for suspected deep invasion or large tumors
Practical Advice:
- Regularly inspect eyelid skin, especially if you have a history of skin cancer or excessive sun exposure.
- Seek prompt evaluation for any persistent eyelid lesion, ulcer, or new growth.
Standard Non-Surgical and Medical Therapies
While surgery is the mainstay of treatment for most cases, several non-surgical options can play a valuable role—particularly for small, superficial tumors or in patients who are not surgical candidates.
Topical Therapies:
- Imiquimod cream: An immune response modifier used for superficial BCCs; applied 5–7 times per week for several weeks.
- 5-Fluorouracil (5-FU): A topical chemotherapeutic for certain superficial variants. Used less frequently on the eyelid due to sensitivity but may be considered in select cases.
Photodynamic Therapy (PDT):
- Involves applying a light-sensitive agent (such as aminolevulinic acid), followed by exposure to a specific light wavelength to destroy cancerous cells.
- Useful for superficial or thin BCCs; limited effectiveness for deeper tumors.
Radiation Therapy:
- Reserved for inoperable cases, recurrences, or elderly patients who cannot undergo surgery.
- Typically delivered as fractionated external beam radiation.
- Risks include skin atrophy, chronic dryness, pigment changes, and—rarely—induction of secondary tumors.
Systemic Medical Therapies:
- Hedgehog pathway inhibitors (e.g., vismodegib, sonidegib): Oral medications for advanced, inoperable, or metastatic BCCs, or tumors unsuitable for surgery/radiation.
- Side effects include muscle cramps, taste changes, hair loss, and weight loss. Close monitoring is necessary.
Advantages and Limitations:
- Non-surgical therapies may offer excellent cosmetic outcomes for superficial lesions.
- Not suitable for aggressive, infiltrative, or deeply invasive tumors.
- Compliance with treatment regimen and close follow-up is essential.
Practical Advice:
- Discuss all options with your provider, including benefits, risks, and likely cosmetic results.
- Report any skin changes, redness, or ulceration during therapy promptly.
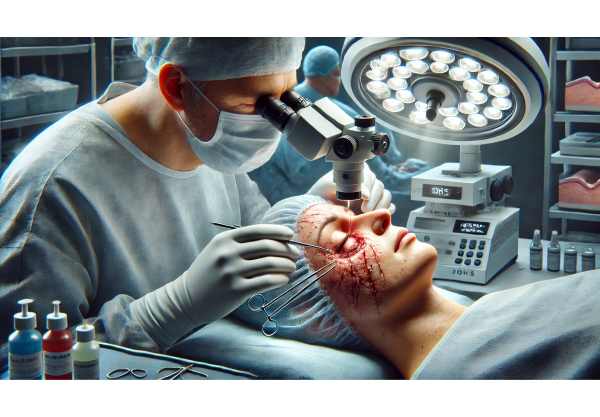
Operative Techniques and Local Interventions
Surgical excision is the gold standard for most eyelid BCCs, aiming for complete tumor removal while preserving function and appearance. Recent advances have improved cure rates, minimized tissue loss, and enhanced cosmetic outcomes.
Standard Excision with Margin Control:
- Tumor is excised with a margin of healthy tissue, followed by histopathological examination to confirm clear edges.
- Reconstruction of the eyelid is performed using local flaps or grafts as needed.
Mohs Micrographic Surgery:
- A staged excision technique, removing the tumor in thin layers with immediate microscopic evaluation.
- Highest cure rates (>98%) and best tissue preservation—especially critical in the eyelid where anatomy is delicate.
Cryosurgery:
- Involves freezing the tumor using liquid nitrogen or nitrous oxide.
- Less commonly used for eyelid BCC due to the risk of damage to adjacent ocular structures.
Laser Therapy:
- CO2 lasers or other ablative lasers may be employed for select, small superficial tumors.
- Requires specialist expertise to avoid collateral damage.
Reconstructive Approaches:
- Depending on tumor size and location, may require direct closure, local tissue flaps, or free skin grafts.
- Oculoplastic surgeons are highly skilled in restoring both function and appearance.
Intraoperative Imaging and Margin Assessment:
- Newer techniques include frozen section analysis and confocal microscopy for real-time margin assessment.
Risks and Considerations:
- Complications may include scarring, eyelid malposition, dry eye, or—in rare cases—tumor recurrence.
- Lifelong monitoring is recommended due to the risk of new or recurrent lesions.
Practical Advice:
- Select a surgeon experienced in eyelid oncology and reconstruction.
- Ask about reconstructive options and expected recovery timeline.
Cutting-Edge Innovations and Technological Advances
The management of eyelid BCC has rapidly evolved, integrating novel techniques and technologies that improve detection, treatment, and patient outcomes.
Advanced Diagnostic Imaging:
- High-frequency ultrasound, optical coherence tomography (OCT), and in vivo confocal microscopy enhance preoperative tumor mapping and margin definition.
- AI-powered diagnostic platforms now assist in image interpretation and early lesion detection.
Targeted Therapies and Molecular Medicine:
- Ongoing development of hedgehog pathway inhibitors and other targeted agents offers hope for advanced and recurrent BCC.
- Immunotherapies, such as immune checkpoint inhibitors, are under investigation for select aggressive cases.
Enhanced Surgical Tools:
- Femtosecond lasers and radiofrequency devices allow more precise excision and tissue handling.
- Fluorescence-guided surgery enables real-time identification of tumor margins.
3D Printing and Custom Implants:
- Used in complex eyelid reconstruction, patient-specific implants crafted from biocompatible materials optimize both form and function.
Telemedicine and Digital Follow-up:
- Secure digital platforms enable remote monitoring of post-operative sites and prompt intervention for recurrences, improving long-term outcomes.
Patient-Centered Cosmetic Solutions:
- Advances in makeup camouflage and prosthetic devices offer psychological support and improved self-esteem during and after treatment.
Practical Advice:
- Inquire about eligibility for clinical trials or advanced imaging if you have recurrent or complex tumors.
- Leverage digital follow-up tools for easy access to care and peace of mind.
Clinical Research and Future Directions
The future of eyelid BCC management lies in personalized, less invasive, and more effective strategies, supported by robust research and collaboration across specialties.
Key Clinical Trials:
- Studies evaluating new topical immunomodulators and systemic inhibitors for locally advanced and metastatic BCC.
- Comparative trials of Mohs surgery vs. advanced excision techniques for optimal cosmetic and functional results.
- Trials of non-invasive diagnostic imaging for early, accurate lesion detection.
Translational and Basic Science Research:
- Exploration of genetic and molecular markers for high-risk BCC.
- Bioengineering research focused on regenerative techniques for eyelid reconstruction.
Emerging Technologies:
- Development of point-of-care diagnostics, such as rapid molecular tests for BCC subtyping.
- AI-based decision support for risk stratification and treatment planning.
Preventive Strategies:
- Research into UV-protective compounds and genetic screening for individuals at high risk.
- Public health initiatives promoting sun safety and early skin checks.
Patient-Centered Outcomes:
- Focus on quality of life measures, psychological support, and patient-reported satisfaction.
- Inclusion of patients’ values and preferences in treatment decisions.
Practical Advice:
- If you have a history of BCC, enroll in registries or studies to contribute to ongoing research.
- Stay engaged with patient advocacy organizations to learn about new advances and resources.
Frequently Asked Questions
What are the first signs of basal cell carcinoma of the eyelid?
The earliest signs include a painless bump, nodule, or sore that does not heal. Other symptoms may include eyelash loss, ulceration, or changes in eyelid appearance. Any persistent lesion should be evaluated by a specialist.
How is basal cell carcinoma of the eyelid diagnosed?
Diagnosis involves a clinical eye exam and biopsy of the lesion. Additional imaging may be used to determine the tumor’s size and depth, especially in larger or recurrent cases.
What is the best treatment for eyelid basal cell carcinoma?
Mohs micrographic surgery is the gold standard for most cases, offering the highest cure rates and best cosmetic outcomes. Small, superficial tumors may be managed with topical treatments or radiation if surgery is not possible.
Can eyelid basal cell carcinoma come back after treatment?
Recurrence is possible, especially if the tumor was large or incompletely excised. Lifelong follow-up is important, as new or recurrent tumors can occur even years after treatment.
Are non-surgical treatments effective for eyelid BCC?
Topical therapies, photodynamic therapy, and radiation can be effective for small, superficial tumors or when surgery is not an option. However, surgery remains preferred for deeper or aggressive cancers.
How can I reduce my risk of eyelid basal cell carcinoma?
Protect your eyes and face from sun exposure by wearing sunglasses, wide-brimmed hats, and sunscreen. Early evaluation of suspicious lesions and regular skin checks are vital preventive measures.
Is eyelid basal cell carcinoma life-threatening?
Eyelid BCC is rarely life-threatening but can cause significant local tissue destruction if untreated. Prompt diagnosis and management prevent complications and preserve vision.
Disclaimer:
This guide is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult an eye care professional for individual concerns.
If you found this article useful, please consider sharing it on Facebook, X (formerly Twitter), or your preferred social media platform. Your support helps us continue providing trusted, high-quality health information to all!






