Understanding Melanocytoma of the Optic Disc
Melanocytoma of the optic disc is a rare, benign tumor that develops from melanocytes, the cells that produce pigment in the body. These tumors are typically found on or near the optic disc, which is the region of the eye where the optic nerve connects to the retina. Melanocytomas are pigmented lesions that appear dark and elevated on the optic disc. These tumors are usually benign and slow-growing, but they can cause complications such as vision changes and, in rare cases, malignant transformation.
Patients with optic disc melanocytoma are frequently asymptomatic, with the tumor discovered incidentally during routine eye exams. Some people may experience visual symptoms such as blurred vision, visual field defects, or even sudden vision loss if the tumor impinges on nearby ocular structures or causes secondary complications like optic disc edema or retinal detachment.
The exact cause of optic disc melanocytoma is unknown, but it is thought to be caused by melanocyte proliferation in the optic nerve head. The condition can occur at any age, but it is most commonly diagnosed in adults. Because of the possibility of visual impairment and the rare risk of malignant transformation, this condition requires close monitoring and appropriate management.
Standard Treatments for Optic Disc Melanocytoma
Given the benign nature of optic disc melanocytomas, traditional management focuses on regular monitoring and symptomatic treatment. Here are the main traditional approaches:
Observation and Monitoring
The most common approach to treating optic disc melanocytoma is to monitor the patient closely and follow up on a regular basis. Because these tumors are usually benign and slow-growing, most ophthalmologists recommend routine eye exams every 6 to 12 months to check for changes in the size, appearance, or associated symptoms of the tumor. This method enables early detection of potential complications such as growth, malignant transformation, or secondary effects like retinal detachment or optic nerve compression.
Visual Field Testing
Regular visual field testing is frequently used to monitor any changes in the patient’s vision that may be due to the melanocytoma. This testing aids in the early detection of visual field loss or other visual disturbances, guiding the need for additional intervention. Any significant changes in the visual field may necessitate further diagnostic imaging or consideration of treatment options.
Fundus Photography and Optical Coherence Tomography (OCT)
Fundus photography and optical coherence tomography (OCT) are important tools for monitoring optic disc melanocytoma. Fundus photography produces a detailed, color image of the retina and optic disc, allowing for accurate documentation of tumor size and appearance over time. OCT provides high-resolution cross-sectional images of the retina and optic nerve head, allowing for the detection of subtle structural changes as well as secondary complications like retinal edema or detachment.
Symptomatic Treatment
If melanocytoma of the optic disc causes significant visual symptoms or complications, symptomatic treatment may be required. For example, if the tumor causes high intraocular pressure or optic disc edema, medications like intraocular pressure-lowering agents or corticosteroids may be prescribed to relieve symptoms and prevent further visual deterioration.
Surgical Intervention
Because optic disc melanocytomas are typically benign, surgical intervention is rarely required. However, in rare cases where the tumor is rapidly growing, causes significant visual impairment, or has malignant transformation, surgical options such as vitrectomy or optic nerve sheath fenestration may be considered. These procedures aim to relieve optic nerve compression, minimize complications, and preserve vision.
Cutting-Edge Solutions for Optic Disc Melanocytoma
Advances in medical technology and a better understanding of ocular tumors have resulted in significant improvements in the treatment and management of optic disc melanocytoma. These cutting-edge approaches improve diagnostic accuracy, target therapies, and monitoring capabilities, radically altering the landscape of care for this rare condition.
Advanced Imaging Techniques
Recent advances in imaging technology have made it much easier to diagnose and monitor optic disc melanocytoma. High-resolution imaging modalities, such as enhanced depth imaging optical coherence tomography (EDI-OCT) and swept-source OCT, enable detailed visualization of the optic nerve head and surrounding structures. These methods enable precise measurement of tumor dimensions, detection of subtle changes over time, and identification of secondary complications.
Fundus Autofluorescence (FAF)
Fundus autofluorescence (FAF) imaging is a non-invasive method for detecting the presence of lipofuscin, a pigment that accumulates in retina cells. FAF imaging can help distinguish melanocytoma from other pigmented lesions of the optic disc and detect changes that may indicate malignant transformation. This advanced imaging modality improves diagnostic accuracy and allows for long-term monitoring of these tumors.
Optical Coherence Tomography Angiography(OCTA)
Optical coherence tomography angiography (OCTA) is a novel imaging technique that produces detailed images of the retinal and choroidal vasculature without the use of dye injection. OCTA can help detect vascular changes caused by optic disc melanocytoma, such as abnormal blood vessel growth or vascular compromise. This information can help assess the risk of complications and guide treatment decisions.
Gene and Molecular Profiling
Advances in genetic and molecular profiling have opened up new avenues for studying the underlying biology of optic disc melanocytomas. Next-generation sequencing (NGS) and gene expression profiling are two techniques that can identify genetic mutations and molecular markers linked to tumor behavior and malignancy risk. This data can help guide personalized treatment plans and improve prognosis.
Targeted Therapies
Targeted therapies represent a significant advancement in the treatment of ocular tumors, such as optic disc melanocytoma. These therapies aim to selectively target specific molecular pathways involved in tumor growth and progression while minimizing damage to healthy tissues in the surrounding area. Possible targeted therapies for melanocytoma are:
- BRAF Inhibitors: Mutations in the BRAF gene are common in many melanocytic tumors. BRAF inhibitors, such as vemurafenib and dabrafenib, can block the activity of the mutated BRAF protein, thereby inhibiting tumor growth. Clinical trials are underway to determine the efficacy of these inhibitors in treating ocular melanocytic tumors.
- MEK Inhibitors: Trametinib and other MEK inhibitors target the BRAF signaling pathway’s downstream components. These inhibitors can complement the effects of BRAF inhibitors, resulting in a more effective treatment strategy. Combining BRAF and MEK inhibitors has shown promising results in the treatment of melanoma and may have the potential to treat optic disc melanocytomas.
Immunotherapy
Immunotherapy has transformed the treatment of many cancers, and its potential for treating ocular tumours is being investigated. Checkpoint inhibitors, like pembrolizumab and nivolumab, inhibit proteins that prevent the immune system from attacking cancer cells. These inhibitors have demonstrated remarkable efficacy in the treatment of metastatic melanoma and are being studied for their potential use in the management of malignant optic disc melanocytoma.
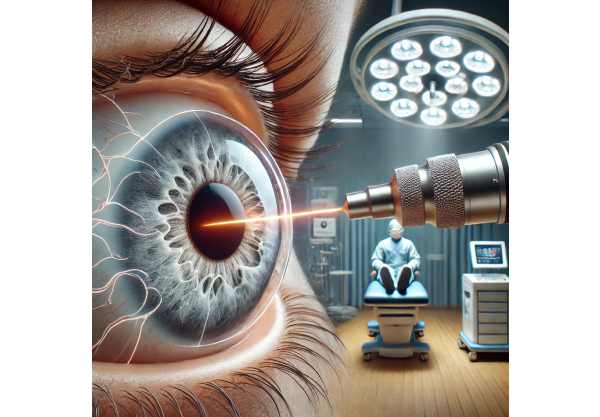
Laser Therapy
Laser therapy provides a minimally invasive treatment option for optic disc melanocytoma. Transpupillary thermotherapy (TTT) and photodynamic therapy (PDT) are two techniques that use laser energy to selectively target and destroy tumor cells while preserving healthy tissue around them. These treatments can shrink tumors, relieve symptoms, and prevent further complications.
Artificial Intelligence, Machine Learning
Artificial intelligence (AI) and machine learning (ML) are revolutionizing the field of ophthalmology by improving diagnostic accuracy and treatment planning. AI algorithms can identify patterns and predict tumour behavior from large datasets of imaging and clinical data. These technologies allow for early detection of changes in melanocytoma, personalized treatment plans, and improved patient outcomes.
Robotic Assisted Surgery
Robotic-assisted surgery is a new technology that improves precision and control during complicated ophthalmic procedures. Robotic systems give surgeons more dexterity and visualization, allowing them to remove tumors more accurately and manage associated complications. This technology lowers the risk of surgical errors while improving overall surgical outcomes.
Liquid Biopsy
A liquid biopsy is a non-invasive diagnostic tool that examines circulating tumor DNA (ctDNA) in the blood to detect genetic mutations and track treatment response. Liquid biopsy is a less invasive alternative to traditional tissue biopsies and provides real-time information about tumor dynamics. This technique has a high potential for early detection of malignant transformation and monitoring the efficacy of targeted treatments.
Combination Therapies
Multiple treatment modalities are becoming more popular in the management of optic disc melanocytoma. For example, combining targeted therapies with immunotherapy or laser therapy can improve treatment efficacy while lowering the risk of recurrence. Personalized combination therapies tailored to individual patient profiles show great promise for achieving long-term tumor control while preserving vision.






