What is a macular hole?
A macular hole is a small break or tear in the macula, the central part of the retina that provides the sharp, detailed vision required for tasks like reading and face recognition. The condition primarily affects central vision, resulting in blurriness and distortion. Macular holes can develop gradually, usually due to age-related changes, but they can also be caused by trauma, eye disorders, or other underlying health conditions. Early detection and appropriate management are critical for maintaining vision and preventing further deterioration.
Comprehensive Analysis of Macular Hole
Macular holes are a serious ocular condition that can have a negative impact on central vision, so it’s important to understand their causes, stages, symptoms, and risk factors.
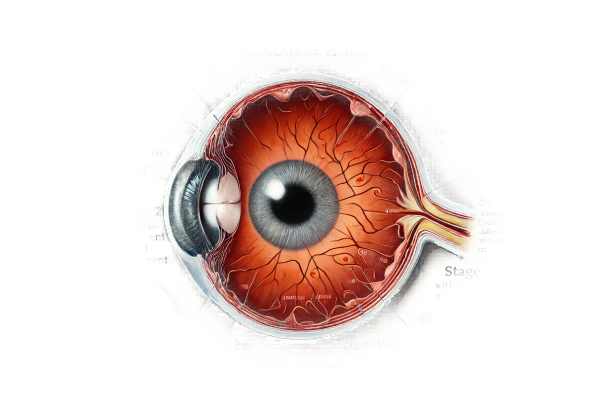
Anatomy and Function of the Macula
The macula is a small, central area of the retina that is approximately 5 millimeters in diameter and densely packed with photoreceptor cells, particularly cones. These cells are necessary for high-resolution vision, color discrimination, and the ability to detect fine details. The fovea, which is located in the center of the macula, is the focal point for clear central vision.
Causes and Risk Factors
Several factors may contribute to the development of macular holes:
- Age-Related Changes: Age-related vitreous shrinkage is the leading cause of macular holes. As people age, their vitreous humor, a gel-like substance that fills the eye, begins to liquefy and contract, causing traction on the retina. This can cause the formation of a macular hole.
- Trauma: Eye injuries can directly damage the macula, resulting in the formation of holes. This can result from either blunt force trauma or penetrating injuries.
- Retinal Disorders: Conditions like retinal detachment, diabetic retinopathy, and high myopia (severe nearsightedness) can all increase the risk of developing macular holes due to structural changes in the retina.
- Macular Edema: Swelling or thickening of the macula, which is commonly associated with inflammation or vascular conditions, can weaken retinal tissue and contribute to hole formation.
- Post-Surgical Complications: Macular holes can occur as a complication of eye surgeries, particularly those involving the vitreous or retina.
Stages of Macular Hole Development
Macular holes typically progress through distinct stages, each with its own unique features and visual implications:
- Stage 1 (Foveal Detachment). In the early stages, the vitreous pulls on the macula, resulting in a small detachment or pseudohole. Patients may notice slight visual distortions or blurriness.
- Stage 2 (Partial Thickness Hole): As traction increases, a small, full-thickness hole forms in the macula, causing more visible vision changes like central blurriness and difficulty reading or recognizing faces.
- Stage 3 (Full-Thickness Hole): The hole grows into a full-thickness macular hole, significantly impairing central vision. Patients frequently describe a central dark spot (scotoma) and more severe visual distortions.
- Stage 4 (Complete Hole and Vitreous Detachment): In the final stage, the vitreous separates completely from the retina, and the macular hole may continue to grow. Central vision is significantly impaired, and the surrounding retina may be compromised.
Symptoms and Clinical Presentation
The symptoms of a macular hole differ depending on the stage and severity of the condition.
- Blurry Vision: At first, patients may notice minor blurriness or distortion in their central vision, making it difficult to read or perform detailed tasks.
- Visual Distortion: Straight lines may appear bent or wavy (metamorphopsia), and objects may appear smaller or farther away than they actually are (mipsia).
- Central Scotoma: As the hole grows, a dark or empty spot in the central vision may appear, obstructing direct vision and causing significant visual impairment.
- Difficulty with Close-Up Work: Activities requiring sharp, detailed vision, such as reading, sewing, or driving, become more difficult.
Effects on Quality of Life
Macular holes can cause significant visual impairment, reducing an individual’s quality of life. Daily tasks requiring fine vision, such as reading, writing, and recognizing faces, become difficult. This can lead to frustration, decreased independence, and an increased risk of accidents due to poor central vision.
Differential Diagnosis
Differentiating macular holes from other conditions with similar symptoms is critical for effective treatment. Conditions to consider are:
- Macular Degeneration: Age-related macular degeneration (AMD) is characterized by drusen (yellow deposits) and changes in the retinal pigment epithelium.
- Macular Pucker: Macular pucker, also known as epiretinal membrane, is characterized by the formation of a thin layer of scar tissue on the macula, resulting in similar visual distortions but without a full thickness hole.
- Central Serous Chorioretinopathy: This condition causes fluid accumulation beneath the retina, resulting in temporary central vision blurring and distortion that usually resolves without permanent damage.
Diagnostic methods
A comprehensive evaluation by an eye care professional is required to diagnose macular holes, which includes a combination of clinical examination and advanced imaging techniques to confirm the presence and stage of the hole.
Clinical Evaluation
- Patient History and Symptoms: A thorough patient history is required, with a focus on the onset and progression of visual symptoms, any history of eye trauma, previous surgeries, and underlying health conditions that may contribute to macular hole development.
- Visual Acuity Testing: This test assesses vision clarity and helps determine the severity of central vision impairment. A significant reduction in visual acuity may indicate the presence of a macular hole.
- Amsler Grid Test: Patients examine a grid of straight lines for areas of distortion or missing lines, which can aid in the detection of central vision problems caused by macular holes.
Imaging Techniques
- Optical Coherence Tomography (OCT): OCT is considered the gold standard for diagnosing macular holes. It produces high-resolution cross-sectional images of the retina, allowing for precise visualization of the macular anatomy. OCT can determine the presence, size, and stage of a macular hole, as well as any associated vitreomacular traction or retinal changes.
- Fundus Photography: This technique involves taking detailed images of the retina to help document the macula’s appearance and track changes over time. It is useful for identifying the macular hole and any other retinal abnormalities.
- Fluorescein Angiography: While not commonly used to diagnose macular holes, fluorescein angiography can help evaluate the retinal blood vessels and detect any leakage or abnormal blood flow that may be associated with the condition.
Specialized Tests
- Microperimetry: This test maps the retina’s visual sensitivity, allowing researchers to assess the functional impact of the macular hole on central vision. It can provide useful information about the severity of vision loss and the likelihood of visual recovery following treatment.
- Electroretinography (ERG): ERG measures the retina’s electrical responses to light stimuli, which helps to assess overall retinal function. Although not specific to macular holes, it can reveal additional information about the retina’s health.
Macular Hole Treatment
The primary goal of macular hole treatment is to improve or restore central vision by addressing underlying causes and facilitating the hole’s closure. The specific approach is determined by the stage and severity of the hole, as well as the patient’s overall health and visual requirements.
Surgical Treatment
- Vitrectomy: Vitrectomy is the most commonly used and effective treatment for macular holes. This surgical procedure removes the vitreous gel that is causing traction on the retina. Typically, the surgery involves several key steps:
- Vitreous Removal: Carefully remove the vitreous gel to relieve traction on the macula.
- Peeling the Internal Limiting Membrane (ILM): The ILM, a thin membrane on the retina’s surface, is peeled away to allow the macula to flatten and the hole to close.
- Gas or Air Bubble Insertion: A gas or air bubble is introduced into the vitreous cavity to press against the macula and help close the hole. The patient must remain face-down for several days after surgery to keep the bubble in place.
Non-surgical Treatments
- Ocriplasmin Injection: For some patients with early-stage macular holes, injecting ocriplasmin (Jetrea) into the eye may be an option. Ocriplasmin is an enzyme that aids in the dissolution of the proteins responsible for vitreomacular adhesion, potentially leading to the spontaneous closure of the macular hole. This treatment is less invasive than surgery, but it is only appropriate for a specific group of patients.
Post-operative Care and Recovery
- Face-Down Positioning: Following vitrectomy, patients are usually required to remain in a face-down position for several days. This positioning allows the gas or air bubble to press against the macula, facilitating hole closure and retinal healing.
- Monitoring and Follow-Up: Regular follow-up visits are essential for monitoring the healing process, identifying complications, and assessing visual improvement. Depending on the progress of the recovery, additional treatments or care adjustments may be required.
Complications and Prognoses
- Complications: As with any surgical procedure, vitrectomy carries risks such as infection, retinal detachment, cataract formation, and increased intraocular pressure (IOP). However, modern surgical techniques and meticulous postoperative care have significantly reduced these risks.
- Prognosis: The outlook for macular hole surgery is generally positive, with a high success rate for hole closure and significant visual improvement in many patients. The size and duration of the hole, as well as the patient’s adherence to postoperative care instructions, determine the extent of vision recovery.
Innovative and Emerging Therapies
- Advanced Imaging and Diagnostics: Advancements in imaging technologies, such as adaptive optics and high-resolution OCT, are improving the ability to detect macular holes earlier and track treatment response more accurately.
- Minimally Invasive Techniques: Researchers are looking into less invasive surgical techniques and novel therapeutic agents to improve the treatment of macular holes. These approaches seek to shorten recovery time and improve outcomes while minimizing complications.
- Stem Cell Therapy: Research into stem cell therapy has the potential to regenerate retinal tissue and restore vision in patients with macular holes, though this area of study is still in its early stages.
- Gene Therapy: Advances in gene therapy may provide future treatment options for macular holes, particularly those associated with genetic retinal disorders. These treatments seek to correct underlying genetic defects and promote retinal healing.
Effective Ways to Improve and Prevent Macular Hole
- Regular Eye Examinations: Schedule regular eye exams to detect early signs of macular holes or other retinal conditions. Early detection can result in timely intervention and better outcomes.
- Monitor Vision Changes: Be aware of any changes in vision, such as blurriness, distortion, or dark spots in the central vision. Report these symptoms to an eye care professional right away.
- Protect Eyes from Trauma: Wear protective eyewear when participating in activities that may result in eye injury, such as sports or hazardous work environments. Trauma can cause or worsen macular holes.
- Manage Systemic Health Conditions: Keep systemic conditions like diabetes and hypertension under control, as they can have an impact on eye health and increase the risk of retinal disorders, including macular holes.
- Healthy Lifestyle: Eat a well-balanced diet high in antioxidants, vitamins, and minerals to promote overall eye health. Leafy greens, fish, and fruits are all good sources of nutrition.
- Avoid Smoking: Smoking increases the risk of many eye diseases, such as macular degeneration and retinal disorders. Quitting smoking can help protect your eyesight.
- Follow Postoperative Instructions: If you have surgery for a macular hole, follow all postoperative care instructions, including face-down positioning and medication use, to ensure a full recovery.
- Regular Monitoring Post-Surgery: After treatment, continue to have regular eye exams and follow-up visits to monitor for any recurrence or new issues, as well as to ensure your eye health.
- Stay Current on New Treatments: Keep up with new developments in the treatment of macular holes. Advances in medical research may provide additional management and prevention options.
Trusted Resources
Books
- “Retina” by Stephen J. Ryan
- “Macular Surgery” by Jorge G. Arroyo
- “Age-Related Macular Degeneration” by Jennifer I. Lim
Online Resources
- American Academy of Ophthalmology (AAO) – aao.org
- National Eye Institute (NEI) – nei.nih.gov
- American Society of Retina Specialists (ASRS) – asrs.org
- Macular Society – macularsociety.org






