What is Exfoliative Glaucoma?
Exfoliative glaucoma (XFG), also known as pseudoexfoliative glaucoma, is a type of secondary open-angle glaucoma that occurs when extracellular material accumulates in the anterior segment of the eye. This condition is linked to exfoliation syndrome (XFS), in which flaky, dandruff-like material accumulates on the lens, iris, and other ocular structures. Exfoliative glaucoma is a major cause of blindness worldwide, especially among older adults. Understanding the causes, symptoms, and diagnostic methods of XFG is critical for its successful management and treatment.
Detailed Investigation of Exfoliative Glaucoma
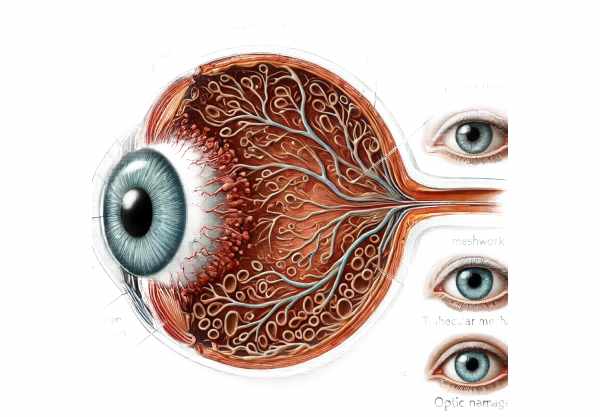
Exfoliative glaucoma is a complex condition caused by the abnormal accumulation of fibrillar material in the eye’s anterior segment. This material prevents the normal outflow of aqueous humor through the trabecular meshwork, resulting in increased intraocular pressure (IOP) and subsequent optic nerve damage.
Pathophysiology
Exfoliative glaucoma is distinguished by the presence of pseudoexfoliative material (PXM), which is produced by abnormal basement membrane components and the extracellular matrix. This material can be found on the lens capsule, zonules, ciliary body, iris, and corneal endothelium. The deposition of PXM alters the normal architecture and function of the trabecular meshwork, increasing resistance to aqueous humor outflow.
Causes and Risk Factors
Exfoliative glaucoma is primarily associated with exfoliation syndrome; however, several other factors can contribute to its development.
- Genetic Predisposition: Genetic factors play an important role in XFG, with specific gene polymorphisms, such as LOXL1, being strongly linked to the condition.
- Age: The prevalence of XFG increases with age, with most cases affecting people over the age of 60.
- Geographic and Ethnic Factors: XFG is more prevalent in certain populations, such as those of Scandinavian, Greek, and South African descent. Environmental factors, such as UV exposure, may also contribute to regional variation in prevalence.
- Gender: According to some studies, women have a higher prevalence of XFG than men.
- Other Ocular Conditions: High myopia and previous ocular trauma can increase the likelihood of developing XFG.
Symptoms
Exfoliative glaucoma typically progresses slowly and can be asymptomatic in its early stages. As the condition progresses, the following symptoms may appear:
- Elevated Intraocular Pressure: Increased IOP is a primary feature of XFG and can cause significant optic nerve damage if not treated.
- Vision Loss: Progressive optic nerve damage causes peripheral vision loss, which can progress to central vision loss if not treated appropriately.
- Eye Pain: Elevated IOP may cause discomfort or pain in the affected eye.
Patients may experience halos around lights and intermittent blurred vision as a result of fluctuating IOP levels. - Light Sensitivity: The presence of PXM and iris atrophy may cause increased light sensitivity.
Clinical Features
The presence of pseudoexfoliative material is an important clinical feature of XFG that can be seen with slit-lamp biomicroscopy. The material appears as white, flaky deposits on the lens capsule that form a distinctive bull’s-eye pattern. Additional clinical features include:
- Iris Transillumination Defects: PXM deposition can cause patchy iris atrophy, resulting in transillumination defects.
- Anterior Chamber Changes: The anterior chamber may become more pigmented as a result of iris pigment release.
- Trabecular Meshwork Pigmentation: PXM and liberated pigment granules accumulate in the trabecular meshwork, making it appear heavily pigmented.
Complications
Exfoliative glaucoma can cause a number of serious complications if not treated:
- Optic Nerve Damage: Elevated IOP causes progressive damage to the optic nerve, resulting in permanent vision loss.
- Cataract Formation: PXM can hasten cataract formation, resulting in decreased visual acuity.
- Angle Closure: Because of synechiae formation and iris atrophy, XFG can occasionally cause secondary angle-closure glaucoma.
Epidemiology
Exfoliative glaucoma is a leading cause of glaucoma worldwide, accounting for a sizable proportion of secondary open-angle glaucoma cases. The prevalence of XFG varies greatly across populations, with higher rates found in Scandinavian countries as well as certain African and Mediterranean regions. The condition is typically diagnosed in people over the age of 60, with a higher prevalence in women.
Patient Education and Support
Patients must be educated about exfoliative glaucoma in order to receive effective treatment. Patients should be educated on the importance of regular eye exams, adhering to prescribed treatments, and monitoring for signs of elevated IOP. Individuals dealing with XFG can benefit from support groups and educational resources that provide additional assistance and encouragement.
Diagnostic Approaches for Exfoliative Glaucoma
Exfoliative glaucoma is diagnosed through a comprehensive eye examination and specialized tests to determine the presence of pseudoexfoliative material, intraocular pressure, and optic nerve health.
Clinical Examination
Diagnosing XFG begins with a thorough clinical examination by an ophthalmologist. The key components of the examination are:
- Slit-Lamp Biomicroscopy: This procedure allows the ophthalmologist to examine the anterior segment of the eye in detail. The presence of pseudoexfoliative material on the lens capsule, iris, and other structures can be determined. The material typically appears as white, flaky deposits on the lens capsule, with a distinct bull’s-eye pattern.
- Intraocular Pressure Measurement: Determining intraocular pressure (IOP) is critical for diagnosing glaucoma. Tonometry can detect elevated IOP, which is a defining feature of XFG. Multiple measurements may be required to confirm consistently high IOP levels.
Diagnostic Tests
Several diagnostic tests are used to assess the extent of glaucoma damage and track disease progression.
- Gonioscopy: This test uses a specialized lens to examine the drainage angle of the eye. Gonioscopy determines whether the angle is open or closed, as well as the extent of pigmentation in the trabecular meshwork and the formation of synechiae.
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the optic nerve head and retinal nerve fiber layer. This imaging technique detects and monitors glaucomatous damage by measuring the thickness of the retinal nerve fiber layer as well as the optic nerve head parameters.
Visual field testing, also known as perimetry, evaluates the patient’s peripheral vision. This test detects early functional damage to the optic nerve caused by high IOP. Patterns of visual field loss are common in glaucoma and can help distinguish XFG from other types of glaucoma.
- Pachymetry: This test determines the thickness of the cornea. Corneal thickness can affect IOP readings, and thin corneas are associated with an increased risk of glaucoma progression.
Advanced Imaging Techniques
Advanced imaging techniques can provide detailed information about the structure and function of the eye.
- Scanning Laser Polarimetry (SLP): This technique uses polarized light to measure the thickness of the retinal nerve fiber layer. This test detects early glaucomatous changes and tracks disease progression.
- Confocal Scanning Laser Ophthalmoscopy (CSLO): CSLO captures detailed images of the optic nerve head and retina. It evaluates the structural integrity of the optic nerve and detects glaucomatous damage.
- Ultrasound Biomicroscopy (UBM): This technique uses high-frequency ultrasound to produce detailed images of the eye’s anterior segment. This method is useful for determining the anatomy of the drainage angle, ciliary body, and other structures involved in XFG.
Standard and Emerging Treatments for Exfoliative Glaucoma
Exfoliative glaucoma (XFG) is treated by lowering intraocular pressure (IOP) to protect the optic nerve and preserve vision. The choice of treatment is determined by the severity of the condition, the patient’s overall health, and their response to initial therapies. Medications, laser therapy, and surgery are all standard treatment options. In addition, novel and emerging therapies are being investigated to improve treatment efficacy and patient outcomes.
Standard Treatment Options
- Medications
- Topical Eye Drops: These are the first line of treatment for XFG and include the following classes of medications:
- Prostaglandin Analogs: Drugs like latanoprost, bimatoprost, and travoprost increase the outflow of aqueous humor, lowering IOP.
- Beta-blockers: Timolol and betaxolol reduce aqueous humor production, which helps to lower IOP.
- Alpha Agonists: Brimonidine and apraclonidine decrease aqueous humor production while increasing uveoscleral outflow.
- Carbonic anhydrase inhibitors: Dorzolamide and brinzolamide reduce aqueous humor production.
- Rho Kinase Inhibitors: Netarsudil promotes the outflow of aqueous humor through the trabecular meshwork.
- Oral Medications: When topical medications fail to control IOP, oral carbonic anhydrase inhibitors such as acetazolamide may be prescribed.
- Laser therapy
- Laser Trabeculoplasty: Laser trabeculoplasty, which includes selective laser trabeculoplasty (SLT) and argon laser trabeculoplasty (ALT), improves aqueous humor outflow through the trabecular meshwork. SLT is frequently preferred due to its reduced risk of scarring and inflammation.
- Laser Iridotomy: When there is a risk of angle closure, a laser iridotomy can create a small hole in the peripheral iris, improving aqueous humor flow and lowering IOP.
- Surgical interventions
- Trabeculectomy: This surgical procedure opens a new drainage pathway for aqueous humor, lowering IOP. It is commonly used when medications and laser therapy are insufficient to control IOP.
- Glaucoma Drainage Devices: Implants like the Ahmed, Baerveldt, or Molteno devices provide an alternative drainage route for aqueous humor, which can help control IOP in severe or refractory cases of XFG.
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures, such as iStent, Trabectome, and Xen Gel Stent, are less invasive options for improving aqueous humor outflow with fewer complications and faster recovery times.
Innovative and Emerging Therapies
- Genetic Therapy
- Gene therapy research aims to target XFG-associated genetic mutations such as LOXL1 polymorphisms. By targeting the underlying genetic factors, gene therapy has the potential to provide a long-term solution for preventing or slowing the progression of XFG.
- stem cell therapy
- Stem cell therapy is being investigated as a means of regenerating damaged trabecular meshwork cells and increasing aqueous humor outflow. Early research suggests that normal trabecular function can be restored while IOP is reduced.
- Neuroprotection
- Neuroprotective agents are being studied to protect the optic nerve from the damage caused by high IOP. In patients with XFG, these agents aim to preserve retinal ganglion cells while also maintaining vision.
- Advanced Drug Delivery System
- Nanotechnology-based drug delivery systems and sustained-release implants are being developed to provide more effective and long-term control of IOP. These technologies aim to increase medication adherence and therapeutic outcomes.
By combining standard treatments with novel therapies, healthcare providers can provide a comprehensive approach to managing exfoliative glaucoma, improving patient outcomes and preserving vision.
Best Practices for Avoiding Exfoliative Glaucoma
- Regular Eye Examination
- Have regular eye exams to catch early signs of exfoliative glaucoma and other vision issues. Early detection enables timely intervention and management.
- Protect the eyes from UV exposure
- Wear 100% UV-blocking sunglasses to protect your eyes from UV exposure, which may contribute to the development of exfoliation syndrome.
- Keep a Healthy Diet
- Consume a well-balanced diet high in antioxidants, vitamins, and minerals that promote eye health, such as leafy greens, fish, and colorful fruits and vegetables.
- Stay hydrated
- Proper hydration improves overall eye health. Drink plenty of water throughout the day to keep your eyes moist and avoid dryness.
- Avoiding Eye Trauma
- Wear protective eyewear when participating in activities that could cause eye injury, such as sports or working with hazardous materials.
- Monitor Systemic Health
- Treat systemic conditions like hypertension and diabetes, which can increase the risk of developing glaucoma.
- Avoid smoking
- Smoking increases the risk of a variety of eye diseases, including glaucoma. Quitting smoking can significantly lower your risk.
- Take Prescribed Medications As Directed
- Follow your eye doctor’s instructions for using prescribed medications to control IOP and slow the progression of exfoliative glaucoma.
- Educate Yourself & Others
- Understand the symptoms and risk factors for exfoliative glaucoma. Educating and encouraging family members to get regular eye exams can aid in early detection and treatment.
- Exercise regularly
- Exercise regularly to improve overall health and reduce the risk of developing conditions that can lead to glaucoma.
Trusted Resources
Books
- “Glaucoma: A Patient’s Guide to the Disease” by Graham E. Trope
- “Clinical Pathways in Glaucoma” by Thom J. Zimmerman
- “The Glaucoma Book: A Practical, Evidence-Based Approach to Patient Care” by Paul N. Schacknow and John R. Samples






