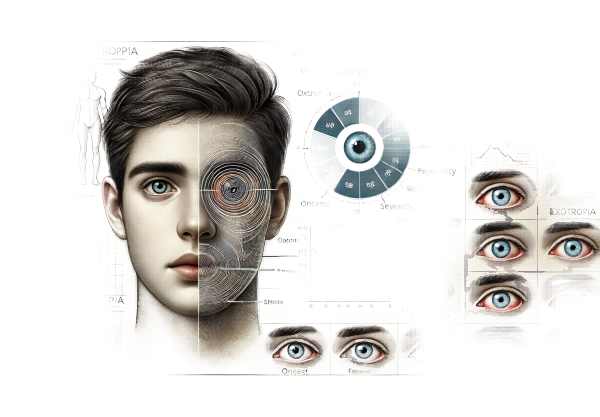
What is exotropia?
Exotropia is an ocular condition marked by outward deviation of one or both eyes. This type of strabismus, also called divergent strabismus, occurs when the eyes are misaligned and point away from each other. Exotropia can be continuous or intermittent, and it may affect one eye more than the other. The condition can occur at any age, but it is most commonly noticed in early childhood. Symptoms include double vision, eye strain, and difficulty perceiving depth, which can interfere with daily activities and overall quality of life.
Comprehensive Study of Exotropia
Exotropia is a type of strabismus in which one or both eyes turn outward. It can have a significant impact on a person’s vision and quality of life. This condition is classified into several types based on its onset, frequency, and severity. Understanding these classifications is necessary for accurate diagnosis and treatment.
Types of Exotropia
- Intermittent Exotropia:
- The most common type is intermittent exotropia, which occurs sporadically. The eye may occasionally turn outward, especially when the person is tired, sick, or concentrating on distant objects. This type typically begins in childhood and can progress over time if not managed properly.
- Constant exotropia:
- In constant exotropia, the outward deviation is consistent and visible at all times. This type can be more difficult to treat and frequently necessitates early intervention to avoid complications such as amblyopia, in which one eye weakens due to lack of use.
- Congenital (Infantile) Exotropia:
- Congenital exotropia is present from birth or develops within the first six months of life. It is usually consistent and may be linked to other neurological or systemic conditions. Early diagnosis and treatment are critical for improving visual outcomes.
- Sensory Exotropia:
- Sensory exotropia is characterized by poor vision in one eye, which can be caused by a variety of conditions including cataracts, retinal diseases, or optic nerve abnormalities. The brain relies on the better-seeing eye, so the weaker eye drifts outward.
- Consecutive Exotropy:
- Following surgical correction of esotropia (inward deviation), consecutive exotropia may develop. It represents an overcorrection, in which the eyes turn outward rather than inward.
Symptoms and Impacts
The symptoms of exotropia differ depending on the type and severity. Common symptoms include:
- Double vision (diplopia):
- This occurs when the brain receives two distinct images from each eye, resulting in visual confusion and discomfort.
- Eye strain (asthenopia):
- Prolonged periods of focusing can lead to fatigue, headaches, and eye discomfort.
- Difficulty in Depth Perception:
- For accurate depth perception, both eyes must be properly aligned. Exotropia can impair this ability, making it difficult to perform tasks requiring precise hand-eye coordination.
- Squinting or closing one eye:
- To avoid double vision, people with exotropia may squint or close one eye, particularly in bright light or while concentrating on a task.
- HEADACHES:
- Chronic eye strain and the effort to maintain binocular vision can cause frequent headaches.
Risk Factors and Causes
Exotropia can be caused by a variety of factors, including:
- Genes:
- A family history of strabismus raises the risk of developing exotropia.
- Visual impairments:
- Conditions such as myopia (nearsightedness) and hyperopia (farsightedness) can disrupt normal eye alignment.
- Neurological Condition:
- Certain neurological disorders, such as cerebral palsy and Down syndrome, are linked to an increased risk of strabismus.
- Trauma
Exotropia can occur as a result of head injuries or eye muscle trauma. - Systemic illnesses:
- Conditions such as thyroid eye disease or myasthenia gravis can impair the muscles that control eye movements.
Pathophysiology
Exotropia is caused by complex interactions of genetic, environmental, and neurological factors. The alignment of the eyes is dependent on the coordinated action of six extraocular muscles controlled by cranial nerves. Strabismus can develop as a result of a breakdown in coordination.
In exotropia, the lateral rectus muscle, which pulls the eye outward, can overpower the medial rectus muscle, which pulls the eye inward. This imbalance causes the outward deviation associated with exotropia.
Development and Progression
Individuals’ experiences with exotropia can vary greatly. In many cases, it begins as intermittent exotropia, or outward deviation that occurs only on occasion. Without intervention, it can lead to constant exotropia, in which the deviation is always present. Visual demand, fatigue, and overall health are all factors that can influence progression.
Children with intermittent exotropia may initially be able to control the deviation using fusion, which is the brain’s ability to combine images from both eyes into a single picture. However, as the condition worsens, the frequency and duration of the outward deviation may increase, resulting in more obvious symptoms and potential complications.
Complications
Untreated exotropia can result in a number of complications, including:
- Amblyopia (lazy eye):
- When the brain prefers one eye over the other, the unused eye can weaken, resulting in amblyopia. Early detection and treatment are critical for avoiding permanent vision loss in the affected eye.
- Loss of Binocular Vision:
- Proper eye alignment is required for binocular vision, which provides depth perception and a large field of view. Exotropia can impair these functions, limiting daily activities and tasks that require precise vision.
- The Psychosocial Impact:
- Visible eye misalignment can have an impact on self-esteem and social interactions, especially among children. Addressing the cosmetic and functional aspects of exotropia is critical to overall well-being.
Epidemiology
Exotropia is a relatively common type of strabismus, with a higher incidence in some populations. It is estimated to affect 1-2% of the general population, with females having a slightly higher prevalence than males. The condition can develop at any age, but it is most commonly diagnosed in early childhood.
Intermittent exotropia is more common in some regions, particularly in Asian populations, where studies have reported rates of up to 5%. These regional differences are most likely the result of genetic and environmental influences.
Psychological and Social Considerations
Living with exotropia can have serious psychological and social consequences, especially for kids. Visible eye misalignment can cause self-consciousness, bullying, and social anxiety. It is critical that parents, caregivers, and educators provide support and understanding to children with exotropia, assisting them in developing confidence and coping with any challenges they may face.
Exotropia in adults can have an impact on their professional and social lives. Addressing the cosmetic aspects of the condition with appropriate treatment can boost self-esteem and improve overall quality of life.
Exotropia Examination Methods
An accurate diagnosis of exotropia is critical for developing an effective treatment strategy. Several diagnostic techniques are used to determine the presence, type, and severity of exotropia.
Comprehensive Eye Examination
A thorough eye examination is the first step in diagnosing exotropia. This includes:
- Patient history:
- Collecting data on the patient’s symptoms, their onset, and any family history of strabismus or other ocular conditions.
- The Visual Acuity Test:
- Assessing the clarity of vision in each eye to detect refractive errors or amblyopia.
- Cover Test:
- The cover test is an important diagnostic tool for exotropia. The patient focuses on a target with one eye covered, and the movement of the uncovered eye is observed. Exotropia is diagnosed when the cover is removed and the covered eye moves outward.
Prism Coverage Test
The prism cover test measures the degree of exotropia. Prisms of varying strengths are placed in front of the eye to balance the deviation. The strength of the prism used to align the eyes indicates the severity of the exotropia.
Hirschberg Test
The Hirschberg test consists of shining a light into the patient’s eyes and observing the reflection on the corneas. The position of the reflections can reveal the extent and severity of eye misalignment. Exotropia causes reflections to be displaced temporally, indicating an outward deviation.
Synoptophore Examination
A synoptophore is an instrument that measures the angle of deviation and evaluates binocular function. The patient looks through the synoptophore, and the examiner adjusts the device to align the images, resulting in a precise measurement of the deviation.
Cycloplegic Refraction
Cycloplegic refraction uses eye drops to temporarily paralyze the ciliary muscle, preventing the eye from accommodating. This allows for precise measurement of refractive errors, which can lead to exotropia. Correcting these errors can help improve eye alignment.
Worth the 4-Dot Test
The Worth 4-dot test measures binocular vision and suppression. The patient wears red-green glasses and sees a target with four dots. The perception of the dots indicates whether both eyes are working together or if one eye is being suppressed.
Near-Point of Convergence (NPC) Test
The NPC test determines the closest point where the eyes can maintain convergence. Patients with exotropia may struggle to maintain convergence, particularly during near tasks. This test evaluates the functional impact of the condition on daily activities.
Imaging Studies
Imaging tests, such as MRIs or CT scans, may be required in some cases to rule out underlying neurological or structural abnormalities that contribute to exotropia. These tests are usually reserved for atypical cases or when other neurological symptoms.
Exotropia Therapy Methods
Standard Treatment Options
- Corrective lenses:
- Corrective lenses, such as glasses and contact lenses, are frequently prescribed to treat underlying refractive errors like myopia, hyperopia, and astigmatism. These lenses can help with eye alignment and reduce the outward deviation caused by exotropia.
- Vision Therapy:*
- Vision therapy, also known as orthoptics, is a series of eye exercises that aim to improve the coordination and strength of the eye muscles. This therapy, usually supervised by an optometrist or orthoptist, aims to improve the brain’s ability to control eye alignment.
- Prism lenses:
- Prism lenses are specialized eyeglasses that help align the images seen by each eye, allowing the brain to combine them into a single image. These lenses can be especially beneficial for managing intermittent exotropia and alleviating symptoms such as double vision.
- Occlusion Therapy:*
- Occlusion therapy involves patching the dominant eye to force the brain to use the weaker eye, which improves function and alignment. This method is commonly used in children to treat amblyopia (lazy eye) caused by exotropia.
- Botulinum Toxin Injections:
- Botulinum toxin (Botox) injections can temporarily weaken the lateral rectus muscle, causing the eye to move outward. This treatment can assist in achieving better alignment and is occasionally used as a less invasive alternative to surgery.
Surgical Treatments
- Strabismus surgery:
Strabismus surgery is a common and effective treatment for severe or persistent exotropia. The surgery consists of repositioning or tightening the eye muscles to improve alignment. It is typically performed as an outpatient procedure, with a short recovery time. - Recession and Resection Procedures:
- These surgical techniques correct the deviation by weakening (recession) or strengthening (resection) specific eye muscles. The type and severity of the exotropia determine which procedure is used.
Innovative and Emerging Therapies
- Neurovisual Training:
- Advances in neuro-visual training employ virtual reality and computer-based programs to create interactive exercises that improve binocular vision and eye coordination. These programs take a modern approach to traditional vision therapy.
- Genetic Therapy:
- Research into gene therapy for strabismus is ongoing, with a focus on correcting the genetic factors that contribute to muscle and nerve dysfunction in the eyes. Although still experimental, gene therapy shows promise for future treatment options.
- Robotic Assisted Surgery:
- Robotic-assisted strabismus surgery improves precision and control during the procedure. This technology is still in the development stages, but it has the potential to improve surgical outcomes and shorten recovery times.
- Pharmacological Interventions:
- Researchers are looking into new medications that target the neurological pathways that control eye movement and alignment. These drugs are intended to improve the efficacy of existing treatments and provide additional options for managing exotropia.
Best Practices for Avoiding Exotropia
- Regular Eye Examination:
- Have a comprehensive eye exam at least once a year to detect and treat any vision issues early.
- Corrected Refractive Errors:
- Correct any refractive errors, such as myopia or hyperopia, with proper glasses or contact lenses to avoid eye strain and misalignment.
- Develop Good Visual Habits:
- Use the 20-20-20 rule: every 20 minutes, look at something 20 feet away for at least 20 seconds to reduce eye strain from prolonged near tasks.
- Keep Proper Lighting:
- Use adequate lighting while reading or working to reduce eye strain and the risk of developing exotropia.
- Limited Screen Time:
- To avoid excessive eye strain, limit your time spent on digital devices and take regular breaks.
- Promote Outdoor Play for Children:
- Encourage children to spend more time playing outside, as natural light and distance focusing can help lower the risk of exotropia.
- Practice Proper Posture:
- Maintain proper posture while reading, writing, and doing other close work to reduce the risk of eye strain and misalignment.
- Monitor for symptoms:
- Be aware of any signs of eye misalignment, such as squinting or closing one eye, and seek immediate evaluation from an eye care professional.
- Promote Eye Exercises:
- Regularly perform eye exercises to strengthen the eye muscles and improve coordination, especially if you have a family history of strabismus.
- Stay hydrated and eat a balanced diet.
- Proper hydration and a diet rich in vitamins and minerals, particularly those beneficial to eye health, can help maintain overall visual function and prevent complications.
Trusted Resources
Books
- “Clinical Management of Binocular Vision” by Mitchell Scheiman and Bruce Wick
- “Binocular Vision and Ocular Motility: Theory and Management of Strabismus” by Gunter K. Von Noorden and Emilio C. Campos
- “Strabismus Surgery and its Complications” by David K. Coats
- “Pediatric Ophthalmology and Strabismus” by Kenneth W. Wright and Peter H. Spiegel










