What is Map-Dot Fingerprint Dystrophy?
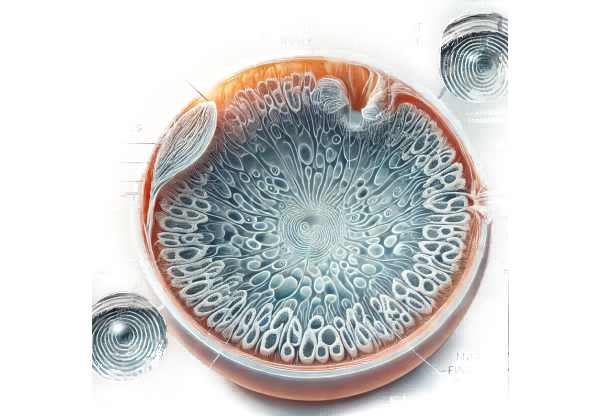
Map-Dot-Fingerprint Dystrophy, also known as epithelial basement membrane dystrophy (EBMD) or Cogan’s microcystic epithelial dystrophy, is a common and usually benign corneal condition. The corneal epithelium is irregular, resulting in a pattern of maps, dots, and fingerprint-like lines on the corneal surface. These abnormalities can result in blurred vision, pain, and recurrent corneal erosion. Although often asymptomatic, symptoms can have a significant impact on daily activities and quality of life.
Detailed Insights into Map-Dot-Fingerprint Dystrophy
Map-Dot-Fingerprint Dystrophy is a condition with distinct morphological characteristics and varying clinical manifestations. Understanding the pathophysiology, risk factors, symptoms, and complications is critical for effective management.
Pathophysiology
Map-Dot-Fingerprint Dystrophy primarily affects the cornea’s epithelial layer and basement membrane. The condition results from an abnormal thickening and duplication of the basement membrane, which causes irregularities on the corneal surface. These abnormalities are typically described as maps, dots, and fingerprint-like patterns that can be seen under a slit lamp.
- Epithelial Changes: The abnormal basement membrane impairs the adhesion of epithelial cells to the underlying stroma. This weak adhesion can lead to recurrent epithelial erosions, in which the outermost layer of the cornea detaches, causing pain and discomfort.
- Irregular Basement Membrane: The duplication and thickening of the basement membrane result in a bumpy surface, causing visual disturbances. The irregularities disrupt the smooth passage of light through the cornea, resulting in blurry vision and glare.
Risk Factors
Several factors can raise the risk of developing Map-Dot-Fingerprint Dystrophy:
- Age: The condition is more common in middle-aged and elderly people, but it can happen at any age.
- Genetics: A family history of corneal dystrophies raises the risk, indicating a genetic predisposition.
- Gender: Some studies indicate that women have a higher prevalence, but the reasons for this are unclear.
- Previous Eye Injuries: Trauma to the eye can worsen the condition or cause symptoms in predisposed people.
- Underlying Eye Conditions: Other corneal disorders or surgeries may contribute to the development or progression of the dystrophy.
Symptoms and Clinical Presentation
The clinical presentation of Map-Dot-Fingerprint Dystrophy varies greatly. While many people are asymptomatic, others have significant symptoms.
- Blurred Vision: Irregularities on the corneal surface disrupt light transmission, resulting in blurred or fluctuating vision. This is often more noticeable upon awakening and may improve throughout the day as the eye surface smoothes with blinking.
- Glare and Halos: Patients may have increased sensitivity to light, glare, and halos near lights, particularly at night.
- Recurrent Corneal Erosions: One of the most distinguishing symptoms is recurrent corneal erosion, which occurs when poorly adherent epithelial cells detach from the cornea. This causes intense eye pain, tearing, redness, and sensitivity to light. These episodes usually occur in the morning or at night.
- Discomfort or Foreign Body Sensation: Patients may experience gritty or foreign body sensations in the eye, particularly during episodes of corneal erosion.
Complications
If left untreated, Map-Dot-Fingerprint Dystrophy can cause a number of complications:
- Chronic Pain: Recurrent corneal erosions cause chronic pain and discomfort, reducing the patient’s quality of life.
- Scarring: Repeated erosions and poor healing can cause corneal scarring, which can lead to permanent vision loss.
- Infections: Corneal erosions increase the risk of bacterial infections, which can cause additional corneal damage and lead to serious complications.
- Visual Impairment: Persistent irregularities and scarring can cause long-term vision impairment, making daily tasks difficult.
Differential Diagnosis
Differentiating Map-Dot-Fingerprint Dystrophy from other corneal conditions is critical for effective management:
- Recurrent Corneal Erosion Syndrome (RCES): Although RCES can be a symptom of Map-Dot-Fingerprint Dystrophy, it can also occur independently or in conjunction with other corneal conditions.
- Fuchs’ Endothelial Dystrophy: This condition affects the cornea’s endothelial layer, causing corneal swelling and vision changes, but it lacks the distinctive epithelial patterns found in Map-Dot-Fingerprint Dystrophy.
- Keratoconus is a progressive thinning of the cornea that results in a cone-shaped protrusion and visual distortion. Unlike Map-Dot-Fingerprint Dystrophy, keratoconus primarily affects the corneal stroma, resulting in more noticeable visual changes.
- Other Epithelial Dystrophies: Meesmann corneal dystrophy and Lisch epithelial corneal dystrophy both affect the corneal epithelium, but they have different clinical and histological characteristics.
Methods to Diagnose Map-Dot-Fingerprint Dystrophy
To accurately diagnose Map-Dot-Fingerprint Dystrophy, a comprehensive approach is required, combining clinical examination with advanced imaging techniques to confirm the presence of characteristic corneal changes.
Clinical Examination
- Slit-Lamp Biomicroscopy is the primary method for diagnosing Map-Dot-Fingerprint Dystrophy. This enables the ophthalmologist to see the corneal surface and identify distinct patterns such as maps, dots, and fingerprint-like lines. To increase the visibility of these subtle changes, the examination is typically conducted with a variety of lighting techniques and magnifications.
- Fluorescein Staining: Using fluorescein dye on the ocular surface can help highlight areas of epithelial irregularity and erosion. Under blue light, the dye accumulates in areas where the epithelium is disrupted, giving a more detailed view of the dystrophic changes.
Imaging Techniques
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the cornea. It can detect thickening and irregularities in the epithelial basement membrane, providing a detailed image of the affected areas. AS-OCT is especially useful for tracking disease progression and assessing treatment efficacy.
- Corneal Topography: This technique maps the cornea’s surface curvature, detecting subtle irregularities that would not be visible under a slit-lamp examination. Corneal topography can help determine the severity of the dystrophy and its effect on the corneal surface.
- Confocal Microscopy: Confocal microscopy enables in vivo examination of the corneal layers at the cellular level. It can detect changes in epithelial cells and basement membranes, providing valuable information about the structural changes associated with Map-Dot-Fingerprint Dystrophy.
Differential Diagnosis
Accurate diagnosis requires distinguishing Map-Dot-Fingerprint Dystrophy from other corneal conditions with similar symptoms. Key conditions to consider are:
- Recurrent Corneal Erosion Syndrome (RCES): RCES is characterized by repeated episodes of corneal epithelial breakdown. It can occur as a result of Map-Dot-Fingerprint Dystrophy or independently. Choosing between the two necessitates a thorough clinical examination and history taking.
- Keratoconus: Although it affects the corneal stroma, keratoconus can cause visual disturbances similar to Map-Dot-Fingerprint Dystrophy. Corneal topography and pachymetry are critical for distinguishing these conditions.
- Other Epithelial Dystrophies: Conditions such as Meesmann corneal dystrophy and Lisch epithelial corneal dystrophy have similar epithelial changes but differ genetically and histopathologically.
Genetic Testing
Genetic testing may be considered in certain cases, particularly if there is a family history of corneal dystrophies. Identifying specific genetic mutations can help confirm the diagnosis and understand the hereditary nature of the disease.
Map-Dot-Fingerprint Dystrophy Treatment Options
The treatment of Map-Dot-Fingerprint Dystrophy, also known as epithelial basement membrane dystrophy (EBMD), focuses on symptom relief, healing, and preventing recurrent corneal erosions. The severity of the symptoms and the impact on the patient’s quality of life determine the appropriate treatment.
Conservative Management
- Lubricating Eye Drops and Ointments: For mild cases, the first line of treatment is to use lubricating eye drops and ointments to keep the cornea moist and relieve discomfort. These products help to relieve dryness and irritation, particularly during periods of corneal erosion.
- Hypertonic Saline: Hypertonic saline eye drops or ointments can help reduce corneal edema and improve epithelial adherence. These treatments are especially beneficial for patients with recurring erosions.
- Bandage Contact Lenses: Soft bandage contact lenses can be used to protect the corneal surface, promote healing, and alleviate the pain caused by recurring erosions. These lenses act as a barrier, allowing the epithelial layer to regenerate uninterrupted.
Medical Treatments
- Topical Antibiotics: Topical antibiotics can be used during corneal erosion to prevent secondary bacterial infections. These are typically prescribed for short-term use.
- Topical Steroids: Applying topical corticosteroids for a short period of time can help reduce inflammation and promote healing. Long-term use is, however, discouraged due to potential side effects such as increased intraocular pressure.
- Autologous Serum Eye Drops: For patients with chronic symptoms, autologous serum eye drops made from the patient’s own blood can provide growth factors that promote epithelial healing and reduce inflammation.
Surgical Interventions
- Debridement: Mechanical debridement is the process of removing loose or abnormal epithelial cells to allow healthier epithelium to grow back. This procedure, usually performed under local anesthesia, can provide relief from recurring erosions.
- Anterior Stromal Puncture: This minor surgical procedure involves making small punctures in the anterior stroma to help the epithelial layer adhere more strongly. It is typically reserved for patients who experience frequent and severe erosions.
- Phototherapeutic Keratectomy (PTK) is a laser procedure that smoothes the corneal surface and removes irregularities. It entails the precise removal of superficial corneal layers with an excimer laser. PTK is especially useful for treating recurring corneal erosions and improving visual clarity.
Innovative and Emerging Therapies
- Gene Therapy: Research into the potential use of gene therapy to address the underlying genetic causes of corneal dystrophies is currently underway. Gene therapy, which targets specific genetic mutations, may provide a long-term solution for patients with hereditary corneal conditions.
- Stem Cell Therapy: Advances in stem cell research suggest the possibility of regenerating damaged corneal tissues. Stem cell therapy has the potential to restore normal epithelial function and improve outcomes for patients experiencing severe or recurring symptoms.
- Nanotechnology: Researchers are investigating nanoparticle-based drug delivery systems to improve the efficacy of topical treatments. These systems can deliver therapeutic agents on a continuous basis, thereby improving treatment outcomes and patient compliance.
To effectively manage Map-Dot-Fingerprint Dystrophy, symptomatic relief, preventive measures, and, in some cases, surgical intervention are required. Medical research advances are constantly improving our understanding of the condition and opening up new treatment options.
Effective Ways to Improve and Prevent Map-Dot-Fingerprint Dystrophy
- Regular Eye Exams: Have routine eye exams to monitor the health of your cornea and detect any early signs of dystrophy or other ocular conditions. Early detection enables timely intervention and improved outcomes.
- Use Lubricating Eye Drops: Regular use of lubricating eye drops can help keep the cornea moist and relieve discomfort. This is especially important for people who have dry eyes or experience recurring erosions.
- Protect Your Eyes: Wear protective eyewear when participating in activities that pose a risk of eye injury, such as sports or hazardous working conditions. Trauma can exacerbate symptoms and cause complications.
- Avoid Eye Rubbing: Rubbing your eyes can cause mechanical trauma to the corneal epithelium, resulting in erosions. If necessary, blot your eyes gently with a clean cloth or tissue.
- Manage Underlying Conditions: Keep systemic conditions like diabetes under control, as they can have an impact on ocular health and increase the risk of cornea problems. Work with your healthcare provider to effectively manage these conditions.
- Stay Hydrated: Stay hydrated to promote overall eye health. Drinking plenty of water can help keep your eyes moist, lowering the risk of dryness and irritation.
- Follow Postoperative Care Instructions: If you have eye surgery, you should follow all of your ophthalmologist’s postoperative care instructions to ensure optimal healing and avoid complications.
- Educate Yourself About Symptoms: Be aware of the symptoms of Map-Dot-Fingerprint Dystrophy, which include blurred vision, glare, and recurring erosions. If you notice any of these symptoms, seek medical attention right away.
- Use Humidifiers: Use a humidifier in your home or workplace to keep humidity levels stable, especially in dry climates. This can help to prevent dryness and irritation of the eyes.
- Wear Sunglasses: To protect your eyes from UV radiation, wear UV-protected sunglasses. UV exposure can lead to a variety of ocular conditions, including corneal dystrophies.
Implementing these preventive measures and lifestyle changes can help improve corneal health and lower the risk of complications caused by Map-Dot-Fingerprint Dystrophy.
Trusted Resources
Books
- “Corneal Dystrophies: A Molecular Genetics Approach” by Vincent P. Argento and Jorge L. Alio
- “Corneal Erosion and Dystrophies” by Ming Wang
- “Ocular Surface Disease: Cornea, Conjunctiva and Tear Film” by Edward J. Holland and Mark J. Mannis
Online Resources
- American Academy of Ophthalmology (AAO) – aao.org
- National Eye Institute (NEI) – nei.nih.gov
- Cornea Research Foundation of America – cornea.org
- EyeWiki by American Academy of Ophthalmology – eyewiki.aao.org






