What is Marfan syndrome?
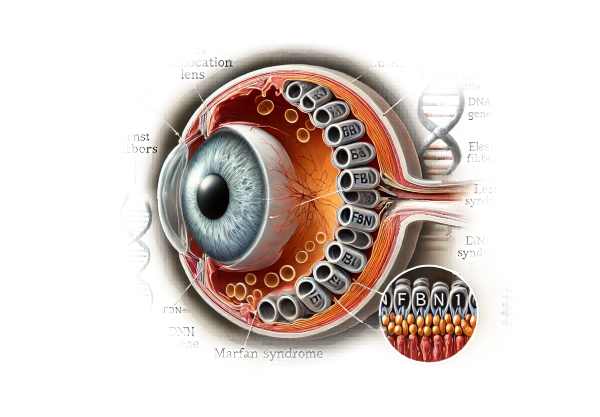
Marfan syndrome is a genetic disorder that affects the connective tissue that structures and supports the body’s organs and tissues. One of the most common ocular manifestations of Marfan syndrome is lens dislocation, also known as ectopia lentis. In this condition, the eye’s lens, which helps to focus light on the retina, is displaced from its normal position. This displacement can cause a variety of visual disturbances and complications, severely affecting the patient’s vision and quality of life.
Detailed Investigation of Marfan Syndrome (Related Lens Dislocation)
Mutations in the FBN1 gene, which encodes the protein fibrillin-1, cause Marfan syndrome, an autosomal dominant disorder. Fibrillin-1 is required for the formation of elastic fibers in connective tissue throughout the body. Defects in this protein cause the various manifestations of Marfan syndrome, including those affecting the ocular system.
Pathophysiology
Lens dislocation in Marfan syndrome occurs as a result of abnormalities in the zonular fibers that hold the lens in place within the eye. Individuals with Marfan syndrome have structurally compromised fibers made of fibrillin. The weakened or disrupted zonules fail to properly anchor the lens, causing it to shift out of its natural position. This dislocation may be partial (subluxation) or complete (luxation).
Clinical Features
The lens dislocation associated with Marfan syndrome has several distinct clinical features and can cause a variety of visual impairments.
- Ectopia Lentis: Ectopia lentis is the most characteristic ocular manifestation of Marfan syndrome. Patients may notice a change in vision as a result of lens misalignment, which can cause blurred or double vision (diplopia). Depending on the severity and direction of the zonular weakness, the lens may shift upward, downward, or sideways.
- Myopia: As a result of eyeball elongation, many Marfan syndrome patients develop myopia (nearsightedness). This condition may exacerbate the visual disturbances caused by lens dislocation.
- Astigmatism: Dislocation-induced irregular curvature of the cornea or lens can result in astigmatism, which causes distorted or blurry vision.
- Lens Opacities: Over time, the dislocated lens may develop opacities or cataracts, worsening vision.
- Glaucoma: A dislocated lens can obstruct the normal outflow of aqueous humor from the eye, causing increased intraocular pressure and the development of secondary glaucoma. If not treated properly, this condition can severely damage the optic nerve and result in permanent vision loss.
Systematic Manifestations
While lens dislocation is a prominent feature of Marfan syndrome, it is important to consider the disorder’s systemic manifestations, which can have a significant impact on overall health and quality of life.
- Cardiovascular System: Marfan syndrome frequently affects the cardiovascular system, with the most serious complications being aortic root dilation and aortic dissection. Mitral valve prolapse and other valve abnormalities are also common, necessitating regular monitoring and, in some cases, surgical repair.
- Skeletal System: Patients with Marfan syndrome frequently have skeletal abnormalities like long, thin limbs (arachnodactyly), scoliosis, and chest deformities (pectus excavatum or pectus carinatum). Joint hypermobility and an increased risk of joint dislocation are also common.
- Respiratory System: Marfan syndrome’s connective tissue abnormalities can harm the lungs, resulting in conditions like spontaneous pneumothorax (collapsed lung) and sleep apnea.
- Skin and Integumentary System: Stretch marks (striae) on the skin are common, even when there is no significant weight change, due to a lack of elastic fibers. In people with Marfan syndrome, hernias may occur more frequently.
Genetic and Environmental Influences
The severity and range of manifestations of Marfan syndrome can vary greatly between individuals, even within the same family. This variability is due to various mutations in the FBN1 gene, as well as potential influences from other genetic and environmental factors. Genetic counseling and testing can assist in identifying specific mutations and providing useful information for managing the condition.
Effects on Quality of Life
Living with Marfan syndrome and its ocular complications can significantly impair a patient’s quality of life. Lens dislocation can cause visual disturbances that interfere with daily activities such as reading, driving, and sports. The fear of progressive vision loss, as well as the need for regular monitoring and possible surgical interventions, can all contribute to anxiety and emotional stress.
Furthermore, the systemic manifestations of Marfan syndrome necessitate comprehensive and coordinated care across multiple medical specialties. Regular appointments with cardiologists, orthopedists, and pulmonologists are required to monitor and manage the various aspects of the disorder. Patients and their families may face significant financial burdens due to the need for lifelong medical care and the possibility of serious complications.
Diagnostic methods
An accurate diagnosis of lens dislocation in Marfan syndrome necessitates a thorough evaluation that includes clinical examination, imaging techniques, and genetic testing. Early detection and diagnosis are critical to timely intervention and management.
Clinical Examination
- Visual Acuity Test: Measuring the patient’s visual acuity can help determine the severity of visual impairment caused by lens dislocation. This test assesses visual clarity and sharpness and can detect myopia, astigmatism, and other refractive errors.
- Slit-Lamp Examination: A slit-lamp examination provides a detailed view of the eye’s anterior segment, allowing the ophthalmologist to see the lens and detect any displacement or opacities. This examination can reveal the direction and extent of the lens dislocation, as well as the presence of any associated cataracts.
- Fundus Examination: A thorough examination of the retina and optic nerve is required to detect any signs of glaucoma or other retinal abnormalities. This examination helps to determine the overall health of the eye and to identify potential complications associated with lens dislocation.
Imaging Techniques
- Ultrasound Biomicroscopy (UBM) is a high-resolution imaging technique that produces detailed images of the eye’s anterior segment. It is especially useful for visualizing zonular fibers and determining the amount of lens displacement. UBM can also detect subtle changes that would not be visible under a slit lamp.
- Optical Coherence Tomography (OCT) is a non-invasive imaging technique that generates cross-sectional images of the retina and optic nerve. It is useful for determining the effect of lens dislocation on retinal structures and detecting secondary complications like glaucoma or macular edema.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT examines the anterior segment of the eye, which includes the cornea, iris, and lens. This imaging technique allows for the visualization of the lens’s position and the condition of the zonular fibers, which aids in the diagnosis and treatment of lens dislocation.
Genetic Testing
Genetic testing is an important part of diagnosing Marfan syndrome because it confirms the presence of mutations in the FBN1 gene. Identifying the specific mutation can provide critical information about the disorder’s severity and progression, guiding clinical management and genetic counseling.
- Molecular Genetic Testing: This test examines the patient’s DNA for mutations in the FBN1 gene. It can confirm the diagnosis of Marfan syndrome while also distinguishing it from other connective tissue disorders with similar characteristics.
- Family History and Genetic Counseling: A detailed family history can reveal inheritance patterns and help identify other family members who may be at risk. Genetic counseling informs patients and their families about the disorder’s genetic components, potential risks, and implications for future pregnancies.
Treatment for Marfan Syndrome (related lens dislocation)
The treatment of lens dislocation in Marfan syndrome focuses on reducing visual impairment, avoiding complications, and managing associated systemic symptoms. A multidisciplinary approach involving ophthalmologists, geneticists, cardiologists, and other specialists is required for complete care.
Non-surgical Management
- Corrective Lenses: Prescription glasses or contact lenses can correct refractive errors like myopia and astigmatism in cases of mild lens dislocation. This method is frequently the first line of treatment for improving visual acuity without invasive procedures.
- Monitoring: Regular eye exams are essential for tracking the progression of lens dislocation and detecting any complications, such as glaucoma or retinal detachment. Early intervention can help prevent severe vision loss.
- Medications: If elevated intraocular pressure is detected, medications such as beta-blockers, prostaglandin analogs, or carbonic anhydrase inhibitors may be prescribed to treat glaucoma.
Surgical Interventions
- Lens Removal (Lensectomy): If lens dislocation severely impairs vision or causes other complications, surgical removal of the dislocated lens (lensectomy) may be required. This procedure involves removing the lens while keeping the capsular bag intact to support a future intraocular lens (IOL) implant.
- Intraocular Lens (IOL) Implantation: Following lens removal, an artificial intraocular lens (IOL) can be inserted to restore focusing power. Several techniques, including:
- Capsular Tension Ring (CTR): Inserting a CTR helps to stabilize the capsular bag and support the IOL, which is especially useful in patients with weak or damaged zonules.
- Scleral Fixation: If the capsular bag is not suitable, the IOL can be sutured to the sclera (white part of the eye).
- Vitrectomy: In some cases, a vitrectomy may be necessary to remove the vitreous gel and treat complications such as retinal detachment. This procedure, when combined with lensectomy and IOL implantation, can improve visual outcomes.
Innovative and Emerging Therapies
- Minimally Invasive Techniques: Advances in minimally invasive surgical techniques, such as micro-incision cataract surgery (MICS), result in shorter recovery times and fewer complications. To remove the dislocated lens, these techniques make smaller incisions and use advanced phacoemulsification technology.
- Femtosecond Laser-Assisted Surgery: Femtosecond laser technology enables precise, bladeless incisions for lens removal and IOL implantation, thereby improving surgical accuracy and outcomes. This technique is especially useful in complex cases with weak zonules.
- Customizable IOLs: Research into customizable intraocular lenses seeks to provide tailored solutions for patients with specific visual requirements. Multifocal and toric IOLs can correct multiple refractive errors, resulting in improved overall visual quality.
- Pharmacological Advances: Researchers are looking into pharmacological agents that can strengthen zonular fibers or prevent their degradation, potentially reducing the need for surgical interventions. These treatments seek to address the underlying connective tissue defect in Marfan syndrome.
Effective management of lens dislocation in Marfan syndrome necessitates a tailored approach that takes into account the severity of the condition, associated systemic manifestations, and patient preferences. Advances in surgical techniques and emerging therapies are improving patients’ outcomes and quality of life.
Effective Strategies for Improving and Avoiding Marfan Syndrome (Related Lens Dislocation)
- Regular Eye Examinations: Schedule regular eye exams to monitor your eyes’ health and detect early signs of lens dislocation or other complications. Early detection enables timely intervention and improved outcomes.
- Genetic Counseling: If you have a family history of Marfan syndrome, you should seek genetic counseling to determine your risk and discuss preventive measures. Genetic testing can provide useful information about the likelihood of passing the condition down to future generations.
- Maintain a Healthy Lifestyle: Eat a well-balanced diet high in vitamins and minerals that promote connective tissue health. Antioxidant-rich foods, such as fruits and vegetables, can help keep your eyes healthy.
- Avoid High-Risk Activities: Avoid activities that could cause eye trauma, such as contact sports, as these can exacerbate lens dislocation. If you’re doing anything that could cause an eye injury, wear protective eyewear.
- Manage Systemic Conditions: Collaborate with your healthcare provider to address systemic conditions associated with Marfan syndrome, such as cardiovascular problems. Controlling these conditions can help to reduce the overall disease burden and prevent complications.
- Educate Yourself: Understand the symptoms and potential complications of Marfan syndrome and lens dislocation. Being informed enables you to recognize changes in your vision and seek immediate medical attention.
- Use Corrective Lenses: If prescribed, always wear glasses or contact lenses to correct refractive errors caused by lens dislocation. This can improve visual acuity and reduce eye strain.
- Stay Hydrated: Drink plenty of water to keep your skin and eyes hydrated. Proper hydration promotes overall eye health and helps the ocular structures function properly.
- Protect Your Eyes from UV Radiation: To protect your eyes from harmful ultraviolet rays, wear UV-protective sunglasses. UV exposure can worsen ocular conditions and raise the risk of complications.
- Follow Medical Advice: Stick to the treatment plan and seek advice from your healthcare providers. Regular follow-ups and adherence to prescribed treatments are essential for managing Marfan syndrome and avoiding complications.
Implementing these preventive measures and lifestyle changes can help Marfan syndrome patients manage symptoms, reduce the risk of complications, and improve their overall quality of life.
Trusted Resources
Books
- “The Marfan Syndrome: A Primer for Clinicians and Scientists” by Peter N. Robinson and Maurice Godfrey
- “Marfan Syndrome: A Multidisciplinary Approach” by Alan C. Braverman and Harry C. Dietz
- “The Marfan Handbook: Everything You Need to Know” by Carolyn B. Munch and Peter K. Smith
Online Resources
- Marfan Foundation – marfan.org
- National Marfan Foundation – marfan.org
- Genetics Home Reference – Marfan Syndrome – ghr.nlm.nih.gov
- National Eye Institute (NEI) – nei.nih.gov






