What is myopic maculopathy?
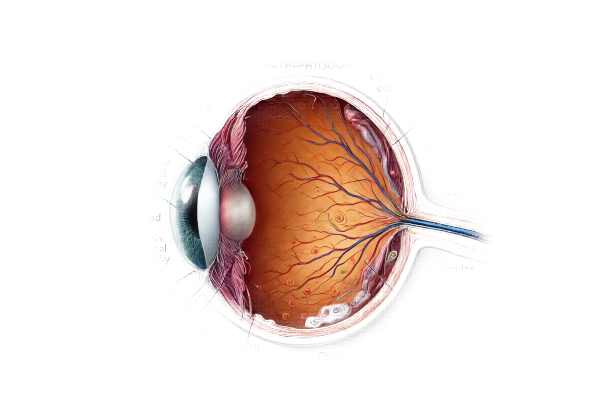
Myopic maculopathy, also known as myopic macular degeneration, is a serious complication of high myopia that can cause vision loss. High myopia is defined as a refractive error of more than -6.00 diopter. The progressive elongation of the eyeball causes structural changes and degenerative processes in the retina, particularly the macula, resulting in this condition. The macula is responsible for central vision, and damage to this area can result in significant visual impairment or blindness. Myopic maculopathy is a leading cause of vision loss worldwide, especially in East Asia, where high myopia prevalence is particularly high.
Myopic Maculopathy: Thorough Exploration
Pathophysiology
Myopic maculopathy develops as a result of the eyeball’s excessive axial elongation in high myopia. This elongation causes a variety of structural changes in the retina, choroid, and sclera. The key pathological changes are:
- Posterior Staphyloma: An outpouching of the eye’s wall in the posterior pole caused by sclera thinning and stretching. Posterior staphyloma can cause significant distortion and thinning of the surrounding retina and choroid.
- Chorioretinal Atrophy: The stretching and thinning of the choroid and retina causes atrophic changes. These changes can be classified into several grades:
- Diffuse Chorioretinal Atrophy: The retina and choroid thin and atrophy, resulting in a yellowish fundus.
- Patchy Chorioretinal Atrophy: Well-defined, whitish lesions resulting from localized atrophy around the macula.
- Lacquer Cracks are linear breaks in Bruch’s membrane, the choroid’s innermost layer. Lacquer cracks increase the risk of choroidal neovascularization (CNV).
- Choroidal Neovascularization (CNV): The formation of abnormal blood vessels from the choroid that penetrate the retina. CNV can cause hemorrhage, exudation, and scar formation, severely impairing vision.
- Macular Hemorrhage: Sudden bleeding in the macula caused by fragile blood vessels or CNV, resulting in vision loss.
- Fuchs’ Spots: Pigmented scars from CNV activity and subsequent hemorrhage. They appear as dark spots in the macula and are indicative of chronic, recurring CNV.
Epidemiology
Myopic maculopathy is most common in populations with high levels of myopia, particularly in East Asian countries like Japan, China, and South Korea. The global rise in myopia, particularly among younger generations, is expected to result in an increase in myopic maculopathy cases. The condition typically begins in early adulthood and can progress with age, resulting in cumulative vision loss over time.
Risk Factors
Several factors influence the development and progression of myopic maculopathy:
- High Myopia: The primary risk factor is a high degree of myopia, which is usually greater than -6.00 diopter.
- Age: The risk grows with age as degenerative changes accumulate over time.
- Genetics: A family history of high myopia and its complications can raise the risk.
- Environmental Factors: Prolonged near work, limited outdoor activities, and high educational pressures have all been linked to the development of high myopia and related complications.
- Posterior Staphyloma: The presence of a posterior staphyloma greatly increases the risk of developing myopic maculopathy.
Clinical Presentation
Patients with myopic maculopathy frequently exhibit a variety of visual symptoms, which can differ depending on the stage and severity of the condition. Common symptoms include:
- Blurred Vision: Progressive blurring of central vision is a defining feature of myopic maculopathy, prompting patients to seek medical attention.
- Metamorphopsia: Distortion of vision in which straight lines appear wavy or bent is common, particularly in the presence of CNV.
- Central Scotomas: Dark or blind spots in the central visual field can appear as macular degeneration progresses.
- Decreased Visual Acuity: Gradual loss of vision clarity, making it difficult to read, drive, or perform tasks that require fine visual detail.
- Sudden Vision Loss: In cases of macular hemorrhage or CNV, patients may experience a sudden and severe loss of central vision.
Complications
Myopic maculopathy can cause a number of serious complications that worsen vision:
- Choroidal Neovascularization (CNV): As previously stated, CNV is a significant complication that can cause hemorrhage, fluid leakage, and scar formation, resulting in severe vision loss.
- Retinal Detachment: High myopia increases the risk of retinal detachment because the retinal tissue thins and stretches.
- Macular Hole: The formation of a full-thickness defect in the macula, which can impair central vision.
- Fuchs’ Spots: These pigmented lesions can indicate recurrent or chronic CNV activity, which contributes to overall vision loss.
Prognosis
The prognosis for myopic maculopathy varies according to the severity and progression of the disease. Early detection and intervention can help to manage symptoms and slow the disease’s progression. However, in advanced cases with significant atrophy or CNV, the prognosis is typically poor, with a high risk of severe visual impairment or blindness.
Methods to Diagnose Myopic Maculopathy
A comprehensive eye examination and advanced imaging techniques are required to accurately diagnose myopic maculopathy. These diagnostic methods assist in determining the extent of retinal damage, identifying complications, and guiding appropriate treatment strategies.
Visual Acuity Test
The visual acuity test, which typically uses a Snellen chart, determines the sharpness of vision. This test determines the degree of visual impairment and tracks changes over time.
Fundus Examination
A thorough examination of the fundus (the eye’s interior surface) with an ophthalmoscope or fundus camera allows direct visualization of the retina, choroid, and optic disc. Key features of myopic maculopathy include posterior staphyloma, chorioretinal atrophy, lacquer cracks, and Fuchs’ spots.
Optical Coherence Tomography(OCT)
OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. It is crucial in diagnosing myopic maculopathy because it can detect:
- Retinal and Choroidal Thickness: OCT determines the thickness of the retina and choroid, revealing areas of thinning and atrophy.
- Lacquer Cracks are linear breaks in Bruch’s membrane.
- Choroidal Neovascularization (CNV): OCT detects CNV, fluid accumulation, and retinal edema.
Fluorescein Angiography(FA)
FA involves injecting a fluorescent dye into the bloodstream and photographing the retina. This imaging technique aids in the detection of leakage, staining, and CNV. FA is especially effective at detecting active CNV and planning treatment interventions.
Indocyanine green angiography (ICGA)
ICGA uses a different dye (indocyanine green) and is particularly useful for visualizing the choroidal vasculature. It aids in the detection of CNV and other choroidal abnormalities that may not be visible using FA.
B-Scan Ultrasound
B-scan ultrasound can provide detailed images of the eye’s internal structures, confirming the presence and extent of posterior staphyloma or retinal detachment.
Visual Field Testing
Visual field tests, such as automated perimetry, determine the extent of central and peripheral vision loss. These tests help to track the progression of myopic maculopathy and assess its impact on the visual field.
Electroretinography (ERG)
ERG measures the retina’s electrical responses to light stimuli. It aids in determining retinal function and identifying any generalized retinal dysfunction that may be associated with myopic maculopathy.
Effective Treatments for Myopic Maculopathy
The goal of myopic maculopathy treatment is to manage symptoms, slow disease progression, and address complications in order to preserve vision. Different therapeutic approaches are used depending on the severity and specific manifestations of the condition.
Pharmacologic Treatments
- Anti-VEGF Therapy: Anti-vascular endothelial growth factor (anti-VEGF) medications used to treat choroidal neovascularization (CNV) include ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin). These drugs prevent the formation of abnormal blood vessels and reduce fluid leakage, thereby improving vision and preventing further damage. Injections are typically given intravitreally, necessitating regular follow-up and monitoring.
- Corticosteroids: In cases where inflammation is a significant factor, corticosteroids can be administered intravitreally to reduce inflammation and edema. Their use is, however, restricted due to potential side effects such as increased intraocular pressure and cataract formation.
Laser Treatments
- Photodynamic Therapy (PDT): PDT involves injecting a photosensitizing agent (verteporfin) into the bloodstream, where it accumulates in abnormal blood vessels. A low-energy laser is then used to activate the drug, which selectively destroys the CNV while sparing the surrounding tissues. PDT is especially effective in treating CNV associated with myopic maculopathy.
- Laser Photocoagulation: Traditional laser photocoagulation may be used in certain cases to seal leaking blood vessels and prevent further damage. However, because of the risk of causing damage to surrounding retinal tissue, this method is less common.
Surgical Interventions
- Vitrectomy: In severe cases with macular hemorrhage, vitreous hemorrhage, or retinal detachment, vitrectomy surgery may be required. This procedure entails removing the vitreous gel and replacing it with a clear solution to improve vision and provide access to the retina for future treatment.
- Macular Buckling: Macular buckling surgery is a novel approach to treating posterior staphyloma. It involves wrapping a silicone band around the eye to reduce sclera stretching and stabilize the macula. This procedure can help to prevent the progression of myopic maculopathy and improve visual outcomes.
Emerging Therapies
- Gene Therapy: Advances in genetic research point to future treatments for myopic maculopathy. The goal of gene therapy is to correct genetic mutations that contribute to disease progression, potentially slowing or stopping it.
- Stem Cell Therapy: Researchers are investigating stem cell therapy’s potential to regenerate damaged retinal cells and restore vision. Although still in the experimental stages, this approach shows promise for treating advanced myopic maculopathy.
- Neuroprotective Agents: Researchers are looking into drugs that protect retinal cells from damage while also promoting cell survival. These neuroprotective agents may provide new treatment options for patients with myopic maculopathy.
Supportive Treatments
- Low Vision Aids: Magnifying glasses, telescopic lenses, and electronic devices can help patients with significant vision loss improve their remaining vision and quality of life.
- Vision Rehabilitation: Vision rehabilitation services offer patients training and support to help them adjust to vision loss. This includes learning how to use low-vision aids, adapting to daily tasks, and receiving psychological support.
By combining these treatments, healthcare providers can effectively manage myopic maculopathy, improving vision and lowering the risk of serious complications.
Effective Ways to Improve and Avoid Myopic Maculopathy
- Regular Eye Exams: Have regular eye exams to detect early signs of myopic maculopathy and track disease progression. Early intervention can help to manage symptoms and avoid complications.
- Control Myopia Progression: Use strategies to slow the progression of high myopia, such as atropine eye drops, orthokeratology lenses, and encouraging children to participate in outdoor activities.
- Monitor Symptoms: Be alert for changes in vision, such as increased blurriness, distortion, or sudden vision loss. Please notify an eye care professional as soon as any new or worsening symptoms appear.
- Protect Eyes from Trauma: Wear protective eyewear when participating in activities that could cause eye injury. Trauma can exacerbate myopic maculopathy and cause additional complications.
- Manage Underlying Conditions: Manage systemic conditions that can harm eye health, such as hypertension and diabetes. Proper treatment of these conditions can lower the likelihood of retinal complications.
- Healthy Lifestyle: Eat a well-balanced diet high in vitamins and nutrients that promote eye health. Foods high in omega-3 fatty acids, vitamins A, C, and E, and zinc are good for your vision.
- Avoid Smoking: Smoking raises the risk of developing myopic maculopathy and other eye diseases. Quitting smoking can improve overall eye health while lowering the risk of complications.
- UV Protection: Wear UV-blocking sunglasses to protect your eyes from harmful ultraviolet rays that can cause retinal damage.
- Stress Management: Engage in stress-reduction activities like mindfulness, meditation, or yoga. Stress can have an impact on one’s overall health, including their eyes.
- Educate Yourself: Learn more about myopic maculopathy and its risk factors. Understanding the condition allows you to take proactive measures to protect your vision.
Trusted Resources
Books
- “Myopia: Prevalence and Progression” by Earl L. Smith III
- “The Myopia Epidemic: Research and Clinical Insights” by Mark A. Bullimore
- “Retina” by Stephen J. Ryan






