What is pleomorphic adenoma of the lacrimal gland?
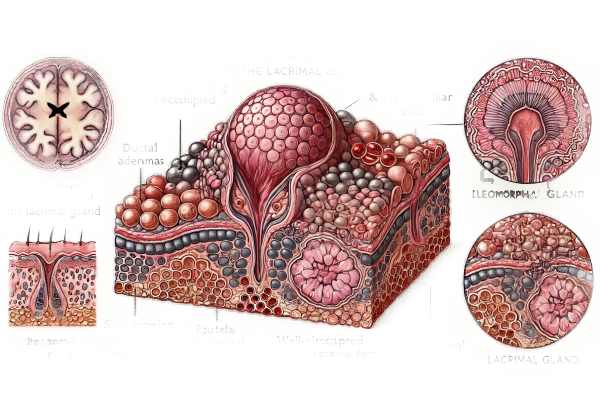
Pleomorphic adenoma of the lacrimal gland, also known as benign mixed tumor, is the most common benign epithelial tumor in the lacrimal gland. This condition primarily affects the eye’s orbital region, which contains the lacrimal gland. The lacrimal gland produces tears, which are necessary for the health and function of the ocular surface. Pleomorphic adenomas have a diverse histological appearance, with epithelial and myoepithelial cells embedded in a myxoid or chondroid stroma.
Epidemiology
Pleomorphic adenoma of the lacrimal gland is relatively uncommon, accounting for only about 10% of all lacrimal gland tumors. It most commonly affects adults aged 40 to 50, with no significant gender preference. Although it can happen at any age, it is less common in children and adolescents.
Pathophysiology
Pleomorphic adenoma develops from the proliferation of ductal and myoepithelial cells in the lacrimal gland. These tumors are typically slow-growing and well-circumscribed, which means they have a distinct separation from the surrounding normal tissue. Pleomorphic adenoma’s exact cause is unknown, but it is thought to be the result of genetic mutations that cause uncontrolled cell growth.
The tumor’s pleomorphic nature refers to its diverse cellular composition and structural patterns. Pleomorphic adenomas have both epithelial elements (such as ductal and acinar structures) and mesenchymal components. This diverse histological makeup causes the tumor to appear heterogeneous under the microscope.
Clinical Presentation
Pleomorphic adenoma of the lacrimal gland causes painless, progressive swelling in the upper outer quadrant of the orbit. The clinical course is often slow, with symptoms appearing over months or years. The following are common clinical characteristics associated with this condition:
Orbital Mass: The most noticeable symptom is a palpable mass in the orbit’s superotemporal region. The mass is typically firm, mobile, and nontender.
Proptosis: As the tumor grows, it may cause forward displacement of the eye (proptosis), resulting in a visible bulging appearance. Proptosis usually develops gradually and can be asymmetric if the tumor only affects one eye.
Diplopia: If the tumor compresses or impairs the extraocular muscles, double vision (diplopia) may result.
Eyelid Swelling: A tumor can cause swelling and fullness of the upper eyelid, which can be confused with other conditions like chronic blepharitis or chalazion.
Epiphora: The tumor may obstruct the lacrimal drainage system, causing excessive tearing (epiphora).
Decreased Visual Acuity: In rare cases, the tumor may compress the optic nerve or other ocular structures, resulting in reduced visual acuity.
Differential Diagnosis
Differentiating pleomorphic adenoma from other orbital and lacrimal gland tumors is critical for accurate diagnosis and treatment. Differential diagnosis includes:
Adenoid Cystic Carcinoma: This is a malignant tumor of the lacrimal gland that can exhibit similar clinical symptoms. It is typically more aggressive and painful than pleomorphic adenoma, with an increased risk of perineural invasion and early metastasis.
Lymphoma: Orbital lymphomas may present with a painless mass and proptosis. They are commonly associated with systemic lymphoproliferative disorders and may have a distinct appearance on imaging studies.
Inflammatory Pseudotumor: Also known as idiopathic orbital inflammation, this condition can have the appearance of a lacrimal gland tumor. It is distinguished by diffuse inflammation and fibrosis of the orbit, which is frequently accompanied by pain and restricted eye movements.
Dermoid cysts are congenital benign cystic lesions that can appear in the orbital region. They are usually present at birth or in early childhood and can cause a palpable mass with slow growth.
Pleomorphic Adenoma of the Salivary Gland: Due to histological similarities, pleomorphic adenomas of the lacrimal gland must be distinguished from those that originate in the salivary glands, particularly the parotid gland.
Complications
Although pleomorphic adenoma is benign, it can cause a variety of complications if not treated properly. Potential complications include:
Malignant Transformation: Although rare, pleomorphic adenoma can progress to carcinoma ex pleomorphic adenoma. This transformation is associated with an aggressive clinical course and a worse prognosis.
Orbital Compression: As the tumor grows, it can put pressure on nearby orbital structures, causing complications like optic nerve compression, extraocular muscle dysfunction, and limited eye movement.
Recurrence: Incomplete surgical excision of the tumor may result in a local recurrence. Recurrent tumors can be more difficult to treat and carry a higher risk of malignant transformation.
Cosmetic Deformity: Large orbital masses can cause significant cosmetic deformities such as proptosis and eyelid asymmetry.
Prognosis
The prognosis for patients with pleomorphic adenoma of the lacrimal gland is generally good, especially if the tumor is detected early and treated properly. The most effective treatment is complete surgical excision with careful preservation of surrounding structures, which has a low recurrence rate. Regular follow-up is necessary to detect any signs of recurrence or malignant transformation.
Diagnostic methods
Pleomorphic adenoma of the lacrimal gland is diagnosed using a combination of clinical evaluation, imaging studies, and histopathology. The main diagnostic methods used are as follows:
Clinical Evaluation
Patient History: A detailed patient history is required to understand the onset, duration, and progression of symptoms. A painless orbital mass, proptosis, diplopia, and any vision changes are all important considerations. It is also important to note any previous ocular conditions or surgeries.
Physical Examination: A thorough examination of the eyes and surrounding structures is carried out. This includes palpating the orbital region to determine the mass’s size, consistency, mobility, and tenderness. Proptosis and eyelid swelling are assessed, as well as any indications of inflammation or infection.
Visual Acuity and Field Testing: Measuring visual acuity and visual fields can help determine whether the tumor is affecting the patient’s vision. This can reveal important information about the tumor’s effects on ocular structures.
Imaging Studies
Computed Tomography (CT) Scan: A CT scan of the orbit is the preferred imaging modality for detecting pleomorphic adenoma. It provides detailed information on the tumor’s size, location, and extent. CT imaging can also reveal characteristics of pleomorphic adenoma, such as a well-defined, non-invasive mass with possible calcification. It is possible to assess the tumor’s relationship to adjacent orbital structures, such as the optic nerve and extraocular muscles.
Magnetic Resonance Imaging (MRI): MRI can help characterize the tumor, particularly its soft tissue components. It provides better contrast resolution than CT and can help distinguish pleomorphic adenoma from other orbital tumors. MRI is especially useful for assessing the potential invasion of adjacent tissues and planning surgical excision.
Ultrasound: Orbital ultrasound can be used in conjunction with other imaging techniques to evaluate the tumor’s internal structure. It is non-invasive and can provide real-time data on the vascularity and echogenicity of the mass.
Histopathologic Examination
Fine-Needle Aspiration Biopsy (FNAB): FNAB is a technique for collecting a tissue sample for cytological analysis. While this procedure is less invasive than surgical biopsy, it has limitations in providing a definitive diagnosis due to the possibility of insufficient sampling and the mixed histological nature of pleomorphic adenoma.
Incisional Biopsy: If FNAB is inconclusive or insufficient, an incisional biopsy may be used to obtain a larger tissue sample. This entails surgically removing a portion of the tumor for histological analysis.
Histopathology: A histopathological examination of the excised tumor is required to make a definitive diagnosis of pleomorphic adenoma. Histological features include epithelial and myoepithelial cells in a myxoid, chondroid, or osseous stroma. Immunohistochemical staining can help to identify specific cell types and confirm the diagnosis.
Treatment for Pleomorphic Adenoma in the Lacrimal Gland
Surgical Treatment
Complete surgical excision:
- The primary treatment for pleomorphic adenoma of the lacrimal gland is complete surgical removal. The goal is to completely remove the tumor while preserving as much of the normal tissue as possible.
- Lateral Orbitotomy: This is the most common surgical procedure for accessing the lacrimal gland. It entails making an incision in the lateral orbital rim, which allows the surgeon to reach and remove the tumor. The adjacent structures, such as the optic nerve and extraocular muscles, are carefully protected.
- Transconjunctival Approach: In some cases, a transconjunctival approach is used, especially if the tumor is small and easily accessible. To reach the lacrimal gland, make an incision in the conjunctiva, the thin membrane that covers the white part of the eye.
- Endoscopic Techniques: Certain tumors can be treated using minimally invasive endoscopic techniques. These techniques remove the tumor with small incisions and specialized instruments, causing minimal disruption to the surrounding tissues.
Post-operative Care
Monitoring and follow-up:
- Regular follow-up visits are required to monitor for signs of recurrence. Postoperative imaging studies, such as MRI or CT scans, may be used to confirm that the tumor has been completely removed and to detect any potential regrowth.
- Histopathological Examination: The excised tumor undergoes histopathological examination to confirm the diagnosis and ensure that the tumor margins are free of residual disease.
Managing complications:
- Postoperative complications are uncommon but may include infection, bleeding, or damage to nearby structures. Prompt management of these complications is critical for a successful recovery.
Non-surgical Management
Observation:
- In some cases, especially for asymptomatic, slow-growing tumors or patients with significant surgical risk factors, a conservative approach involving regular observation and monitoring may be considered. This includes regular imaging studies and clinical evaluations to monitor any changes in tumor size or behavior.
Advanced and Recurrent Cases
Radiation Therapy:
- Radiation therapy may be considered for recurrent pleomorphic adenomas or when surgical excision is not feasible. This method is less commonly used due to the tumor’s typically benign nature and the potential side effects of radiation.
Chemotherapy:
- Because pleomorphic adenoma is a benign tumor, chemotherapy is typically not recommended. However, if malignant transformation occurs, systemic chemotherapy may be part of the treatment plan.
Lifestyle and Supportive Care
Patient education:
- It is critical to educate patients about the nature of the condition, the significance of regular follow-up, and the warning signs of potential recurrence. Patients should be encouraged to report any new or worsening symptoms immediately.
Psychological support:
Living with a benign lacrimal gland tumor can be stressful. Providing psychological support, such as counseling and support groups, can assist patients in dealing with the emotional and social aspects of their condition.
Common Questions Regarding Pleomorphic Adenoma of the Lacrimal Gland
What is a pleomorphic adenoma of the lacrimal gland?
Pleomorphic adenoma of the lacrimal gland is a benign tumor that develops from the epithelial and myoepithelial cells of the lacrimal gland. It has a slow growth rate and a mixed histological appearance.
How are pleomorphic adenomas diagnosed?
Clinical evaluation, imaging studies (such as CT or MRI), and histopathological examination of the excised tumor all contribute to the diagnosis. Tissue samples can also be obtained through a fine-needle aspiration biopsy (FNAB) or an incisional biopsy.
What are the signs of a pleomorphic adenoma of the lacrimal gland?
Common symptoms include painless, progressive swelling of the upper outer quadrant of the orbit, proptosis (forward displacement of the eye), double vision, eyelid swelling, excessive tearing, and, in rare cases, decreased visual acuity.
How are pleomorphic adenomas treated?
The primary treatment is complete surgical removal of the tumour. The surgical approach may differ, but the goal is to remove the tumor while preserving the surrounding structures. In certain cases, regular observation and monitoring may be necessary.
Can pleomorphic adenomas become cancerous?
Pleomorphic adenoma is typically benign, but it can transform into carcinoma ex pleomorphic adenoma in rare cases. This emphasizes the value of regular follow-up and monitoring.
Is pleomorphic adenomas of the lacrimal gland hereditary?
There is no evidence that pleomorphic adenomas of the lacrimal gland are hereditary. The exact cause of the tumor is unknown.
What are the consequences of not treating pleomorphic adenoma?
Pleomorphic adenoma can grow uncontrollably if not treated, potentially leading to complications such as optic nerve compression, extraocular muscle dysfunction, and cosmetic deformity. There is also the possibility of malignant transformation, though this is uncommon.
Can pleomorphic adenoma recur following surgery?
Yes, incomplete surgical excision can cause tumor recurrence. Regular follow-up visits and imaging studies are required to detect any signs of recurrence.
Is there any non-surgical treatment for pleomorphic adenoma?
Regular observation and monitoring are non-surgical treatment options for asymptomatic, slow-growing tumors. Radiation therapy may be considered in recurrent cases or when surgery is not an option.
How can I help a loved one with a pleomorphic adenoma?
Providing emotional support, assisting with medical appointments, and encouraging adherence to follow-up visits and treatment plans are all important ways to help a loved one with pleomorphic adenoma. Joining support groups can also provide more resources and assistance.
Trusted Resources and Support
Books and Organizations
Books:
- “Ophthalmic Pathology: A Text and Atlas”* by David J. Apple and Arthur M. Sandford.
- “Spencer’s Pathology of the Eye” (J. Donald M Gass.
Organizations:
- American Academy of Ophthalmology (AAO): Provides patients and healthcare professionals with comprehensive information on ocular conditions, including pleomorphic adenoma of the lacrimal gland.
- National Eye Institute (NEI): An extensive source of information on eye health and related conditions, including pleomorphic adenoma.
- The American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS) offers information and support to patients suffering from orbital and lacrimal gland conditions.
Financial Aid Options
Insurance Coverage: Most health insurance policies cover the diagnosis and treatment of pleomorphic adenoma. Patients should check with their insurance providers to learn about the specifics of their coverage, such as co-pays and deductibles.
Patient Assistance Programs: Pharmaceutical companies and non-profit organizations frequently provide patient assistance programs to help with the cost of medications and treatments. Programs such as RxAssist provide information about available resources.
Non-Profit Organizations: Organizations like the HealthWell Foundation and the Patient Advocate Foundation help patients pay for medical expenses, including treatments for pleomorphic adenoma.
Government Programs: Medicaid, Medicare, and the Children’s Health Insurance Program (CHIP) provide coverage to eligible individuals. These programs can help cover the costs of treating and caring for pleomorphic adenoma, ensuring that patients receive the medical care they require regardless of their financial situation.






