What is neuroretinitis?
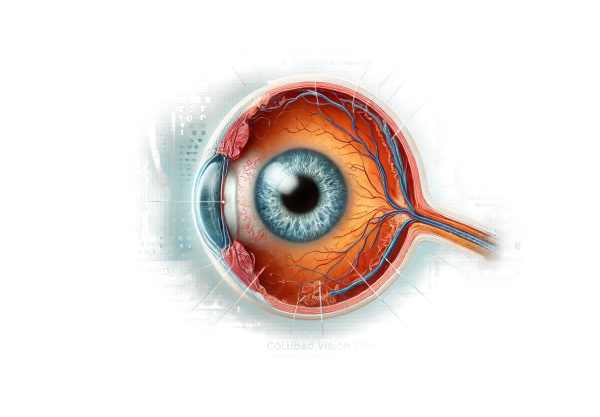
Neuroretinitis is an inflammatory condition affecting both the optic nerve (neuritis) and the retina. The optic nerve head swells, and a macular star, a pattern of exudates radiating from the central macula, is present. This condition frequently results in acute vision loss in one eye and can be caused by a variety of infectious agents, autoimmune diseases, or idiopathic factors. Early diagnosis and treatment are critical for successfully managing the condition and restoring vision.
Detailed Analysis of Neuroretinitis
Neuroretinitis is a relatively uncommon but serious ocular condition that can severely impair vision if not diagnosed and treated promptly. Understanding the pathophysiology, clinical presentation, etiological factors, and complications is critical for both healthcare professionals and patients.
Pathophysiology
Neuroretinitis causes inflammation of both the optic nerve and the retina. The exact mechanism varies depending on the underlying cause, but it typically involves an immune-mediated response. The inflammation leads to:
- Optic Disc Edema: Swelling of the optic nerve head, which is commonly visible during an eye exam.
- Macular Star Formation: Fluid and proteins leak from inflamed retinal vessels and deposit in the retina’s outer plexiform layer, resulting in a distinctive star-shaped pattern.
Clinical Features
Patients with neuroretinitis usually present with acute, unilateral vision loss. The key clinical features are:
- Visual Acuity Reduction: A sudden decrease in vision, commonly referred to as blurring or a gray shadow in the central field of vision.
- Scotoma: Blind spots in the visual field.
- Photophobia: High sensitivity to light.
- Color Vision Deficiency: Difficulty recognizing colors, particularly red and green.
Etiology
Neuroretinitis has two types of causes: infectious and non-infectious.
Infectious Causes
- Cat-Scratch Disease: Cat scratches or bites are a common source of infection for Bartonella henselae.
- Syphilis: Treponema pallidum infection can cause ocular symptoms, including neuroretinitis.
- Lyme Disease: Caused by Borrelia burgdorferi, this condition can cause neuroretinitis in the presence of systemic infection.
- Tuberculosis: Mycobacterium tuberculosis can infect the eye, causing neuroretinitis.
- Viral Infections: Herpes simplex virus, varicella-zoster virus, and other viral agents can all cause neuroretinitis.
Non-infectious Causes
- Autoimmune Diseases: Sarcoidosis and systemic lupus erythematosus can affect the optic nerve and retina.
- Idiopathic: In many cases, no specific cause is identified, so the condition is known as idiopathic neuroretinitis.
Complications
While many patients recover their vision with appropriate treatment, neuroretinitis can cause complications such as:
- Chronic Vision Loss: Persistent inflammation or delayed treatment can cause permanent damage to the optic nerve and the retina.
- Recurrence: Patients with a history of neuroretinitis may have recurrent episodes, especially if the underlying cause is not properly treated.
- Secondary Glaucoma: Inflammation can cause increased intraocular pressure, which can lead to glaucoma and further impair vision.
- Macular Edema: Persistent leakage from retinal vessels can cause chronic swelling in the macula, resulting in persistent visual disturbances.
Differential Diagnosis
Differentiating neuroretinitis from other conditions that cause optic disc edema and vision loss, such as:
- Optic Neuritis: Inflammation of the optic nerve that does not affect the retina or cause macular star formation.
- Central Retinal Vein Occlusion (CRVO): Can cause optic disc swelling and retinal hemorrhages, but lacks the distinctive macular star.
- Papilledema: Bilateral optic disc swelling caused by increased intracranial pressure, without a macular star pattern.
Epidemiology
Neuroretinitis is a rare condition with different incidence rates depending on the underlying cause. It can affect people of all ages, but some causes, such as cat-scratch disease, are more prevalent in younger populations. Both sexes are affected equally, though the prevalence may differ depending on geography and environmental factors.
Prognosis
The prognosis of neuroretinitis is heavily dependent on the underlying cause and the timing of treatment. Infectious causes typically respond well to antimicrobial therapy, whereas non-infectious and idiopathic cases may necessitate prolonged immunosuppressive treatment. Most patients experience significant visual recovery, though some may still have visual deficits.
Diagnostic methods
A combination of clinical examination, imaging studies, and laboratory tests is required to accurately diagnose neuroretinitis. These methods aid in confirming the diagnosis, determining the underlying cause, and directing appropriate treatment.
Clinical Examination
The first step in diagnosing neuroretinitis is to have an ophthalmologist perform a thorough clinical examination. The key components of the examination are:
- Visual Acuity Test: Determines the degree of vision loss.
- Fundoscopy: Using an ophthalmoscope, examine the optic nerve head and retina. The presence of optic disc edema and a macular star are distinguishing features.
- Visual Field Test: Find any scotomas or blind spots in the visual field.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT generates high-resolution cross-sectional images of the retina, allowing for precise visualization of the macular star and retinal layers.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream to create images of the retinal vessels. It aids in the detection of leaks and inflammations.
- Magnetic Resonance Imaging (MRI): An MRI of the brain and orbits can help rule out other causes of optic nerve swelling and detect any associated intracranial pathology.
Lab Tests
- Blood Tests: These tests aid in determining infectious or autoimmune causes. Complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and specific serologies for infections such as Bartonella henselae, syphilis, Lyme disease, and tuberculosis are examples of relevant tests.
- Lumbar Puncture: If central nervous system involvement is suspected, a lumbar puncture may be used to examine cerebrospinal fluid for infections or inflammatory markers.
Neuroretinitis Treatment
Neuroretinitis treatment aims to address the underlying cause, reduce inflammation, and manage symptoms in order to prevent permanent vision loss. The treatment regimen varies according to whether the condition is infectious or not.
Treatment of Infectious Causes
- Antibiotics: When bacterial infections, such as cat-scratch disease (Bartonella henselae) or syphilis, are the cause of neuroretinitis, appropriate antibiotic therapy is required. Cat-scratch disease is typically treated with doxycycline or azithromycin, whereas syphilis is treated with penicillin or doxycycline.
- Antivirals: For viral infections such as herpes simplex virus or varicella-zoster virus, antiviral medications such as acyclovir, valacyclovir, or famciclovir are prescribed.
- Antituberculous Therapy: For tuberculosis-related neuroretinitis, a combination of antituberculous drugs (isoniazid, rifampin, pyrazinamide, and ethambutol) is prescribed.
Treatment of Non-Infectious Causes
- Corticosteroids: Oral or intravenous corticosteroids are frequently used to reduce inflammation and swelling in the optic nerve and retina. Prednisone is commonly prescribed, with dosages based on the severity of the condition.
- Immunosuppressive Agents: Immunosuppressive drugs such as methotrexate, azathioprine, or mycophenolate mofetil may be used to control the immune response and prevent further damage in cases of autoimmune neuroretinitis.
- Intravitreal Injections: In some cases, corticosteroids can be injected directly into the vitreous cavity to better target inflammation.
Symptomatic Treatment
- Pain Management: Neuroretinitis-related pain can be managed with analgesics or nonsteroidal anti-inflammatory drugs (NSAIDs).
- Vision Aids: Using low-vision aids, such as magnifying glasses or specialized lighting, can help patients cope with vision loss during the acute stage.
Innovative and Emerging Therapies
- Biologic Agents: Recent advances in biologic therapies, such as monoclonal antibodies that target specific inflammatory pathways, provide new treatment options for autoimmune neuroretinitis. Agents such as infliximab and adalimumab are being studied for potential benefits.
- Gene Therapy: Research into gene therapy seeks to correct genetic mutations that cause certain types of neuroretinitis. While still experimental, this approach shows promise for future treatments.
- Stem Cell Therapy: Researchers are looking into stem cell therapy’s ability to regenerate damaged retinal and optic nerve tissues. Early studies are promising, but more research is needed to determine efficacy and safety.
Monitoring and Follow-up
Regular follow-up appointments are critical for monitoring the patient’s response to treatment and detecting signs of recurrence or complications. Follow-ups include:
- Visual Acuity Testing: Assess visual acuity on a regular basis to monitor recovery or progression.
- Fundoscopic Examination: A continuous examination of the optic nerve and retina to determine the resolution of inflammation and exudates.
- Imaging Studies: Regular OCT or fluorescein angiography to monitor retinal changes and ensure effective treatment.
Effective Methods to Improve and Prevent Neuroretinitis
Neuroretinitis prevention and management require proactive measures to reduce infection risk and complications. Here are a few effective methods:
- Hygiene Practices: Practice good hygiene, particularly around pets. Wash your hands thoroughly after handling animals to reduce the risk of zoonotic infections such as cat scratch disease.
- Pet Management: To prevent the spread of Bartonella henselae, keep pets indoors, especially cats, and treat them for fleas on a regular basis.
- Vaccinations: Stay up to date on vaccinations to avoid infections like herpes zoster, which can cause neuroretinitis.
- Early Treatment: If you notice any symptoms of infection or unexplained vision loss, seek medical attention right away to ensure an early diagnosis and treatment.
- Regular Eye Examinations: Get regular eye exams, especially if you have underlying conditions that increase your risk of neuroretinitis, such as autoimmune diseases.
- Monitor Chronic Conditions: Treat chronic conditions such as diabetes and hypertension, which can cause ocular inflammation and increase the risk of neuroretinitis.
- Avoid Eye Trauma: Keep your eyes safe from trauma, which can cause inflammatory responses that lead to neuroretinitis.
- Healthy Lifestyle: Maintain a healthy lifestyle that includes a well-balanced diet and regular exercise to improve overall immune function and lower the risk of infections and autoimmune responses.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Ocular Pathology” by Myron Yanoff and Joseph W. Sassani
- “The Retina Atlas” by Lawrence A. Yannuzzi






