Introduction
Malignant melanoma of the eyelid is a rare but aggressive type of skin cancer that develops from melanocytes, the pigment-producing cells in the skin. This condition falls under the category of periocular melanomas, which also includes melanomas of the conjunctiva and other structures surrounding the eye. Melanomas of the eyelid make up a small percentage of all eyelid malignancies, but they are noteworthy for their ability to metastasize and cause significant morbidity.
Malignant melanoma of the eyelid can present in a variety of ways, most commonly as a pigmented lesion or nodule with irregular borders and coloration. It is easily mistaken for benign lesions such as moles or lentigines, emphasizing the importance of early and accurate diagnosis. Symptoms may include changes in the appearance of an eyelid mole or spot, as well as bleeding, itching, or rapid lesion growth.
Excessive ultraviolet (UV) exposure, fair skin, a history of sunburns, and a family history of melanoma all increase the risk of developing malignant melanoma of the eyelid. Given the eyelid’s exposure to sunlight and the thin, delicate skin in this area, UV rays are especially damaging. The prognosis for malignant melanoma of the eyelid is determined by several factors, including the stage at diagnosis, the size and depth of the lesion, and whether it has spread to other areas of the body. Early detection and treatment are critical to improving outcomes.
Conventional Management of Malignant Melanoma of the Eyelids
Traditional treatments for malignant melanoma of the eyelid primarily involve surgical excision, which aims to completely remove the tumor while preserving as much healthy tissue as possible. Here are the main traditional methods:
Surgical Excision
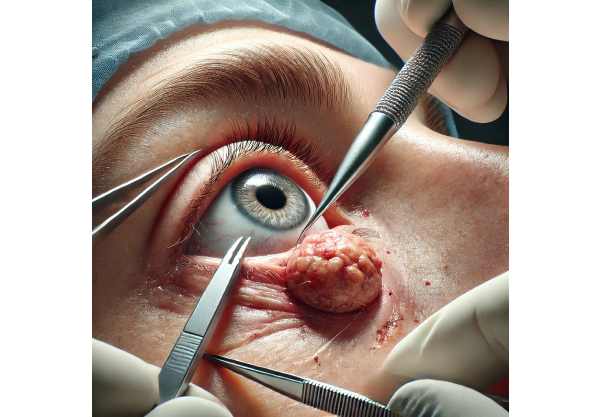
Surgical excision is the primary treatment for malignant melanoma of the eyelid. The goal is to have clear margins, which means no cancer cells remain at the edges of the removed tissue. There are a number of surgical techniques:
- Wide Local Excision: This procedure involves removing the tumor as well as a margin of normal tissue around it in order to ensure complete cancer cell removal. The excised tissue is then sent for histopathological examination to ensure that the margins are clear.
- Mohs Micrographic Surgery: Mohs surgery is a tissue-sparing procedure in which the tumor is removed layer by layer and examined under a microscope until no cancer cells are found. This method is especially useful for tumors with poorly defined borders or those located in cosmetically sensitive areas, such as the eyelid.
Sentinel Lymph Node Biopsy
Sentinel lymph node biopsy is commonly used to determine whether the melanoma has spread to nearby lymph nodes. This procedure involves identifying, removing, and examining the sentinel lymph node (the first node to which cancer cells are likely to spread). If melanoma cells are detected, additional lymph node dissection may be required.
Adjuvant Radiation Therapy
Adjuvant radiation therapy may be recommended when the surgical margins are not clear or the melanoma is aggressive. Radiation can help destroy any remaining cancer cells, lowering the risk of recurrence. It is frequently used in conjunction with surgery in more advanced cases.
Chemotherapy
Chemotherapy is less commonly used for malignant melanoma of the eyelid because melanomas are typically resistant to many traditional chemotherapy agents. However, in cases of advanced or metastatic melanoma, chemotherapy may be considered to control the disease and alleviate symptoms.
Follow-Up and Monitoring
Following initial treatment, regular follow-up is required to monitor for recurrence or the development of new melanomas. Physical examinations, imaging studies, and blood tests are common follow-up procedures. Patients are also advised to use sun protection and self-examination techniques to detect new or changing lesions early.
Innovative Approaches to Treating Malignant Melanoma of the Eyelid
Advances in the treatment of malignant melanoma of the eyelid have significantly improved outcomes and increased the number of available therapies. These cutting-edge innovations include new surgical techniques, targeted therapies, immunotherapies, and advanced diagnostic tools. Here, we will go over these ground-breaking treatments in detail.
Sentinel Lymph Node Mapping using Advanced Imaging
Recent advances in imaging technology have improved sentinel lymph node mapping, which is an important step in the staging of melanoma. Lymphoscintigraphy, single-photon emission computed tomography (SPECT), and positron emission tomography (PET) all produce high-resolution images that aid in the accurate identification of sentinel lymph nodes. These methods improve biopsies’ precision and reduce the possibility of false-negative results, ensuring that even microscopic metastases are detected early.
Targeted Therapies
Targeted therapies have transformed the treatment of many cancers, including malignant melanoma of the eyelids. These treatments target specific genetic mutations or molecular pathways involved in cancer growth and proliferation. The key targeted therapies for melanoma are:
- BRAF Inhibitors: BRAF gene mutations are present in approximately 50% of melanomas. Drugs such as vemurafenib and dabrafenib specifically target these mutations, inhibiting tumor growth and inducing cell death.
- MEK Inhibitors: Often used in conjunction with BRAF inhibitors, MEK inhibitors (such as trametinib) target a downstream component of the same signaling pathway, resulting in a synergistic effect and improved treatment effectiveness.
Immunotherapy
Immunotherapy has emerged as a ground-breaking approach to treating malignant melanoma that uses the body’s immune system to recognize and eliminate cancer cells. The most significant advancements in immunotherapy for melanoma are:
- Checkpoint Inhibitors: These drugs inhibit proteins that keep the immune system from attacking cancer cells. Examples include pembrolizumab and nivolumab, which block the PD-1 pathway, and ipilimumab, which targets CTLA-4. These inhibitors have demonstrated remarkable efficacy in treating advanced melanoma, resulting in long-lasting responses and increased survival.
- Adoptive Cell Transfer (ACT): ACT entails collecting and expanding a patient’s own immune cells (typically T cells) in a laboratory before reintroducing them into the body to combat cancer. This personalized approach has shown promise in clinical trials, particularly in patients with refractory melanoma.
Oncolytic Virus Therapy
Oncolytic virus therapy is a novel treatment in which genetically modified viruses selectively infect and kill cancer cells. T-VEC (talimogene laherparepvec) is an oncolytic herpes virus treatment for advanced melanoma. The virus is injected directly into the tumor, where it replicates, causing tumor cell lysis and activating the anti-tumor immune system.
Photodynamic therapy (PDT)
Photodynamic therapy uses a photosensitizing agent and light to kill cancer cells. A photosensitizer is applied to the affected area and activated by a specific wavelength of light, resulting in reactive oxygen species that kill cancer cells. PDT is especially effective for superficial melanomas and, in some cases, a viable alternative to surgery.
Advanced Surgical Techniques
Advances in surgical techniques are improving the precision and outcomes of melanoma excision. Robotic-assisted surgery, for example, provides increased dexterity and visualization, allowing for more precise tumor removal with less damage to surrounding tissues. Additionally, 3D printing technology is being used to create custom surgical guides and prosthetics, which improves cosmetic and functional outcomes for patients who require extensive reconstruction.






