What is ocular histoplasmosis syndrome?
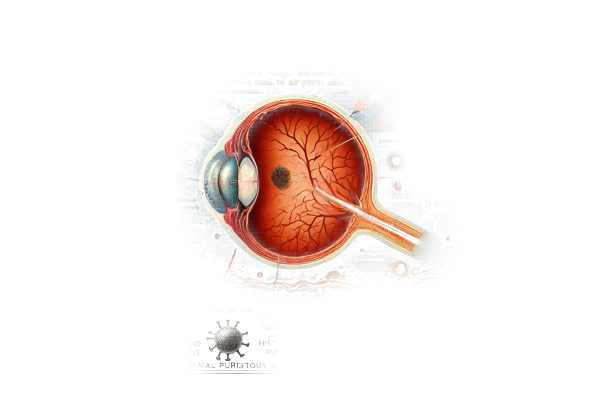
The Histoplasma capsulatum fungus, which typically enters the body through the respiratory system, causes Ocular Histoplasmosis Syndrome (OHS), a severe eye condition. If not treated properly, this syndrome can cause significant vision loss. It primarily affects the choroid and retina, two layers of tissue in the back of the eye. Individuals living in fungus-endemic areas, such as the Ohio and Mississippi River valleys, are more likely to have OHS.
Examining Ocular Histoplasmosis Syndrome Thoroughly
Etiology
Histoplasma capsulatum, a fungus, causes Ocular Histoplasmosis Syndrome. This fungus is often found in soil contaminated with bird or bat droppings. When disturbed, the spores become airborne and can enter the lungs, causing a primary infection. While the initial pulmonary infection is typically mild and self-limiting, in some people, the fungus can spread hematogenously to other parts of the body, including the eyes.
Pathophysiology
The pathophysiology of OHS includes several stages:
- Primary Infection: The first infection occurs in the lungs, where the spores are inhaled. The body’s immune response usually clears the infection, but in some cases, the fungus can spread to other organs, including the eyes.
- Dissemination to the Eyes: Histoplasma organisms can travel from the bloodstream to the choroid, the vascular layer of the eye. The choroid nourishes the retina, and the presence of the fungus can result in choroidal inflammation and lesions.
- Development of Choroidal Lesions: Histo spots are small, white, atrophic areas that spread across the retina. Histo spots may not directly impair vision, but their presence indicates a prior infection.
- Choroidal Neovascularization (CNV): The most serious complication of OHS is the formation of choroidal neovascularization. CNV happens when new, abnormal blood vessels form beneath the retina. These vessels can leak fluid and blood, resulting in scarring and severe vision loss.
Risk Factors
Several factors contribute to the risk of developing OHS.
- Geographic Location: People who live in Histoplasma capsulatum-endemic areas, such as the Ohio and Mississippi River valleys, are more likely to contract the disease.
- Exposure to Contaminated Soil: Activities that disturb bird or bat dropping-contaminated soil, such as farming or construction, can increase the risk of inhaling fungal spores.
- Immune Status: Immunocompromised people, such as those with HIV/AIDS or taking immunosuppressive drugs, are more likely to develop disseminated histoplasmosis and subsequent ocular involvement.
Symptoms
The symptoms of OHS can vary according to the severity and progression of the disease.
- Early Symptoms: In the early stages, people may be asymptomatic or have minor symptoms like floaters or blurriness in their vision.
- Advanced Symptoms: As the disease advances and CNV develops, more severe symptoms may occur, including:
- Blurred or Distorted Vision: The development of CNV can cause significant changes in vision, such as blurring and distortion.
- Loss of Central Vision: CNV can damage the macula, which controls central vision, resulting in a central scotoma (blind spot).
- Metamorphopsia: This condition, which makes straight lines appear wavy or curved, is a common symptom of CNV.
Complications
If left untreated, OHS can cause a number of serious complications:
- Severe Vision Loss: The most serious complication is CNV-induced vision loss with subsequent macula scarring.
- Retinal Detachment: In rare cases, severe CNV can result in retinal detachment, necessitating immediate surgical intervention.
- Secondary Infections: Lesions and inflammation in the eye can increase the risk of secondary infections.
Effects on Quality of Life
OHS can have a significant impact on one’s quality of life. Loss of vision, particularly in the central vision, can impair daily activities such as reading, driving, and recognizing faces. The psychological effects of vision loss, such as anxiety and depression, can be significant.
Epidemiology
OHS is most common in the United States, particularly along the Ohio and Mississippi River valleys. The disease’s prevalence is closely related to the geographic distribution of Histoplasma capsulatum. While primary pulmonary infection is common in endemic areas, only a small number of people develop disseminated histoplasmosis and subsequent OHS.
Pathogenesis
OHS pathogenesis involves an interaction between the host’s immune response and the Histoplasma organism. The initial pulmonary infection causes an immune response, which typically eliminates the infection. However, in some people, the fungus can spread to the eyes, causing the development of histo spots and possibly CNV. The exact mechanisms by which the fungus spreads and causes ocular disease are unknown and under investigation.
Genetic Factors
There is evidence that genetic factors may influence susceptibility to OHS. Certain HLA genotypes are associated with an increased risk of developing the syndrome. Understanding the genetic predisposition to OHS may lead to improved risk assessment and targeted prevention strategies.
Diagnostics
OHS diagnosis requires a combination of clinical evaluation, imaging studies, and laboratory tests. The presence of histo spots on fundoscopic examination, along with symptoms of vision changes and the presence of CNV, are key indicators of the disease. Optical coherence tomography (OCT) and fluorescein angiography are imaging studies used to confirm the diagnosis and determine the extent of ocular involvement.
Methods for Diagnosing Ocular Histoplasmosis Syndrome
Clinical Examination
- Patient History: A detailed patient history is required, with emphasis on symptoms, duration, and potential Histoplasma capsulatum exposure. Detailed questions about activities that may involve exposure to contaminated soil can aid in the identification of risk factors.
- Visual Acuity Test: Measuring visual acuity helps determine the impact of OHS on vision and directs subsequent diagnostic steps.
- Fundoscopic Examination: Using an ophthalmoscope, the eye care professional can examine the retina for histo spots, signs of CNV, and other retinal changes that may indicate OHS.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. It aids in detecting and tracking CNV, retinal thickness, and other structural changes.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and photographing the retina while the dye circulates. It aids in visualizing blood flow in the retina and detecting areas of leakage or neovascularization.
- Indocyanine Green Angiogram (ICG): ICG, like fluorescein angiography, uses a different dye that is especially useful for visualizing choroidal circulation. It may reveal additional information about CNV and other choroidal abnormalities.
Lab Tests
- Histoplasma Antigen Testing: Blood and urine tests can detect antigens or antibodies to Histoplasma capsulatum, indicating a recent or previous infection.
- Chest X-ray or CT Scan: Imaging studies of the chest can reveal signs of previous histoplasmosis infection, such as calcified granulomas in the lungs.
Differential Diagnosis
It is critical to distinguish OHS from other conditions that can produce similar symptoms, such as age-related macular degeneration (AMD), toxoplasmosis, and other causes of CNV. An accurate diagnosis requires a comprehensive clinical evaluation as well as appropriate imaging and laboratory tests.
Ocular Histoplasmosis Syndrome Treatment
Medical Management
- Anti-VEGF Therapy: Injections of anti-vascular endothelial growth factor (anti-VEGF) are the primary treatment for OHS-associated choroidal neovascularization (CNV). Medications like ranibizumab (Lucentis), bevacizumab (Avastin), and aflibercept (Eylea) stop the growth of abnormal blood vessels, reducing leakage and swelling. These injections are given directly into the vitreous cavity of the eye and usually require multiple treatments.
- Corticosteroids: Corticosteroids can help manage inflammation in OHS. They are available as oral medications, periocular injections, and intravitreal injections. While corticosteroids are effective at reducing inflammation, their long-term use should be monitored for potential side effects such as increased intraocular pressure and cataract formation.
- Photodynamic Therapy (PDT): PDT uses a light-activated drug called verteporfin, which is injected into the bloodstream and accumulates in the abnormal blood vessels of the eye. The drug is then activated using a laser, resulting in selective destruction of the CNV while leaving surrounding healthy tissue intact. PDT can be a useful adjunctive therapy for treating CNV.
Surgical Management
- Laser Photocoagulation: Traditional laser photocoagulation uses thermal energy to seal leaking blood vessels and prevent CNV growth. To avoid damaging central vision, this treatment is usually reserved for lesions that are not located near the central macula. Advances in laser technology have improved the precision and effectiveness of this method.
- Vitrectomy: In severe cases with significant vitreous hemorrhage or retinal detachment, a vitrectomy may be required. This surgical procedure removes the vitreous gel from the eye and replaces it with a clear solution to restore and stabilize vision.
Innovative and Emerging Therapies
- Gene Therapy: Research into gene therapy for OHS is currently underway, with the goal of correcting the underlying genetic factors that predispose people to the condition. Although still experimental, gene therapy shows promise for long-term solutions by addressing the underlying cause of the disease.
- Stem Cell Therapy: Stem cell therapy is being investigated as a possible treatment for retinal damage caused by OHS. The goal is to regenerate damaged retinal cells and thus restore vision. Early studies have yielded promising results, but more research is required to determine the safety and efficacy of this approach.
- Combination Therapies: Adding anti-VEGF therapy to other treatments, such as corticosteroids or PDT, may improve treatment outcomes. Ongoing clinical trials are looking into the potential benefits of these combination approaches in treating CNV associated with OHS.
Monitoring and Follow-up
Effective OHS management requires regular monitoring and follow-up. Patients receiving treatment for CNV should have regular eye exams to monitor their response to therapy and detect any recurrence of neovascularization. Imaging studies, such as OCT and fluorescein angiography, are critical for monitoring disease progression and guiding treatment decisions.
Effective Ways to Improve and Prevent Ocular Histoplasmosis Syndrome
- Avoid Exposure to Contaminated Soil: Reduce activities that disturb soil contaminated with bird or bat droppings, particularly in endemic areas. If you cannot avoid exposure, wear protective equipment.
- Use Respiratory Protection: Wear masks or respirators when working in environments where there is a high risk of inhaling fungal spores, such as caves, construction sites, or areas with large bird or bat populations.
- Maintain Good Hygiene: Use good hygiene to reduce your risk of fungal infection. Wash your hands thoroughly after handling soil or working in potentially contaminated areas.
- Regular Eye Exams: Schedule routine eye exams, especially if you live in an endemic area or have a history of histoplasmosis infection. Early detection of ocular changes can help prevent serious complications.
- Monitor Symptoms: Be alert for changes in vision, such as blurriness, distortion, or the appearance of new floaters. Report any changes to an eye care professional as soon as they occur.
- Educate Yourself: Stay current on OHS and its risk factors. Understanding the condition allows you to take proactive steps to protect your eye health.
- Support Your Immune System: Lead a healthy lifestyle to help your immune system. A well-balanced diet, regular exercise, adequate sleep, and stress management can improve overall health and lower infection risk.
- Vaccination: While there is no vaccine for histoplasmosis, staying up to date on other vaccinations can help prevent illnesses that weaken the immune system and increase your risk of fungal infections.
- Avoidance of High-Risk Activities: Avoid activities that increase your risk of contracting Histoplasma capsulatum, such as exploring caves or handling bird or bat droppings without proper protection.
- Environmental Control: Use environmental controls in areas where Histoplasma capsulatum is common. This includes reducing dust and using fungicides in high-risk areas.
Trusted Resources
Books
- “Retinal and Choroidal Manifestations of Selected Systemic Diseases” by J. Fernando Arevalo
- “Infectious Diseases of the Eye” by P. K. Mukherjee
- “Ocular Disease: Mechanisms and Management” by Leonard A. Levin and Peter Humphrey
Online Resources
- American Academy of Ophthalmology: AAO.org
- National Eye Institute: NEI.nih.gov
- Centers for Disease Control and Prevention (CDC): CDC.gov
- Mayo Clinic: MayoClinic.org
- PubMed: PubMed.gov
- American Society of Retina Specialists: ASRS.org
- All About Vision: AllAboutVision.com
- MedlinePlus: MedlinePlus.gov






