Imagine a therapy that replaces the deteriorating cells in your retina and potentially halts—maybe even reverses—the vision loss in dry age-related macular degeneration (AMD). That’s exactly the promise behind OpRegen, a groundbreaking approach that involves transplanting healthy retinal pigment epithelium (RPE) cells into areas affected by the advanced atrophic form of AMD. Instead of relying on drugs or invasive procedures that only slow the disease, OpRegen aims to restore the very cell layer essential for supporting photoreceptors. Below, you’ll find out how this transformative therapy works, why it stands apart from conventional treatments, and what to expect if you or a loved one is considering participating in or benefiting from this innovative solution.
Why OpRegen Is Redefining Hope in Dry AMD
OpRegen is built upon the understanding that retinal pigment epithelium (RPE) cells play a critical role in maintaining healthy vision. These specialized cells supply nutrients, clear waste, and recycle photoreceptor components at the back of the eye. In dry AMD—the most common variant—these RPE cells gradually degenerate, leading to the death of overlying photoreceptors and progressive vision loss. Traditional treatments, while helpful in managing inflammation and other factors, can’t replace cells that are already gone.
Putting Cell Replacement at the Forefront
This therapy’s main goal is to transplant lab-cultured RPE cells to areas damaged by AMD. Here’s why that’s significant:
- Targeted Cell Restoration: Instead of administering broad-spectrum treatments, clinicians implant healthy, lab-grown RPE cells precisely where they’re needed most, offering a more direct and potent intervention.
- Reestablishing Tissue Integrity: These new RPE cells aim to re-create the supportive environment for photoreceptors, potentially halting disease progression and stabilizing or even improving vision.
- Expanding Options for Dry AMD: Dry AMD historically lacks the robust range of therapies available for wet AMD, such as anti-VEGF injections. OpRegen fills this gap with a regenerative approach rather than a purely palliative one.
The Role of Stem Cell Technology
The RPE cells used in OpRegen often originate from pluripotent stem cells—which can differentiate into many tissue types—in a controlled lab environment. This transformation ensures the transplanted cells closely match native RPE functionality. Unlike donor organs, stem-cell–derived RPE doesn’t rely on scarce, time-sensitive donors. Labs can scale up cell production for multiple patients, increasing access and consistency in quality.
Designed for the Atrophic Stage
While early and intermediate AMD primarily involve drusen deposits and subtle changes, atrophic or “dry” AMD often leads to geographic atrophy—large patches of lost RPE and photoreceptors. This is the ideal scenario for RPE replacement because you’re introducing new cells where native ones are missing.
Potential Advantages Beyond Status Quo
- Long-Term Impact: If successful, transplanted RPE could reduce or eliminate the need for repeated office visits common with other treatments (e.g., ongoing injections).
- Vision Preservation: By targeting a root cause—degenerating RPE—OpRegen goes beyond temporarily propping up existing tissue or addressing secondary complications.
- Compatibility: Preclinical and early human data suggest that these transplanted cells integrate well into the retinal structure without eliciting significant immune rejection, especially with proper immunosuppressive strategies.
Who Might Benefit the Most?
Those with moderate to advanced dry AMD—especially with clear signs of geographic atrophy—are prime candidates for RPE therapy. However, the therapy may be less helpful if the surrounding photoreceptors are too far gone or if there’s extensive scarring. Doctors generally evaluate each patient’s degree of atrophy, visual acuity, and overall ocular health (including the macula’s architecture) to determine suitability.
The Hope Factor
Seeing the world in sharp detail, reading comfortably, and retaining independence in daily tasks stand out as pressing concerns for anyone with AMD. OpRegen speaks directly to these aspirations, offering a route to not merely slow the disease but potentially restore some crucial visual functions. Although still under clinical investigation in many areas, the results thus far indicate that regenerating the RPE layer can reshape the standard of care for dry AMD and give new reasons for optimism among patients.
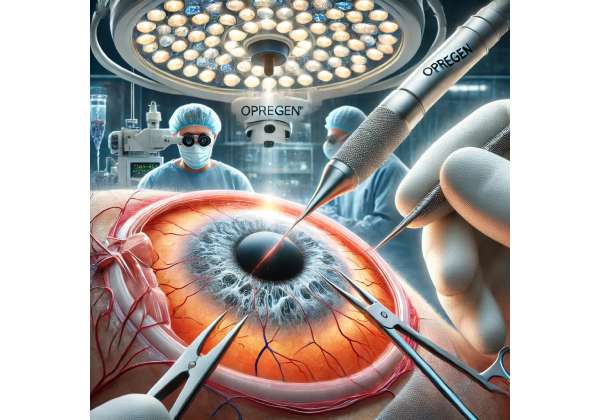
Understanding the RPE Transplant Procedure Step by Step
A successful OpRegen therapy involves much more than injecting cells into the eye. It’s a carefully orchestrated protocol that starts long before patients arrive in an operating suite. From stringent screening to specialized surgical techniques, every element is designed to maximize the potential for healthy cell engraftment and minimal complications.
Initial Assessments and Screening
- Detailed Eye Exam: Specialists use optical coherence tomography (OCT) and other imaging methods to confirm areas of geographic atrophy and evaluate the structural integrity of the retina.
- Visual Function Tests: Baseline measures such as best-corrected visual acuity, contrast sensitivity, and microperimetry help set expectations and track postoperative changes.
- Overall Health Review: Because immunosuppression may be needed, your doctor will check for any conditions—like uncontrolled diabetes or infections—that could complicate healing or increase risks.
Preparing the RPE Cells
- Lab-Grown Cells: Stem cells are coaxed to differentiate into RPE cells in a controlled laboratory setting. Rigorous quality checks ensure the cells have the right morphology and pigment to function as authentic RPE.
- Shipping and Storage: Cell batches often require specialized containers that keep them at stable temperatures, ensuring viability until the moment of transplantation.
Surgical Day: The Transplant Procedure
- Local or General Anesthesia: Depending on the clinic and patient preference, sedation can range from local eye anesthesia to a controlled general procedure, particularly if extended operating times are anticipated.
- Small Incision: The surgeon typically makes a microincision in the sclera (white of the eye) to access the retina.
- Vitrectomy: A vitrectomy tool removes the vitreous gel in the rear chamber, clearing a path for cell placement.
- RPE Cell Delivery: Surgeons use a fine needle or cannula to inject the OpRegen cell suspension into the subretinal space, right beneath the retina where natural RPE usually resides. The injection is slow, ensuring an even spread of cells.
- Monitoring and Closure: The site is carefully inspected. The surgeon checks for complications such as retinal detachment or hemorrhage before sealing the incision.
Postoperative Medications and Care
- Immunosuppression: Transplanted cells may trigger immune reactions, so short-term oral or local immunosuppressants (like corticosteroids) may be prescribed to help the cells survive.
- Infection Prevention: Antibiotic drops are commonly used to ward off infection risks during the early days.
- Anti-Inflammatory Drops: These help control swelling around the injection site and promote stable healing.
- Follow-Up Imaging: OCT and other scans track how well the transplanted cells are integrating. The position, viability, and potential complications—like fluid accumulation—are scrutinized during repeat visits.
Recovery Milestones
- Immediate Days: Some mild discomfort, redness, or blurriness is typical. Adherence to eyedrop schedules and activity restrictions is essential.
- First Weeks to Months: Patients gradually notice whether there’s a stabilization or slight improvement in vision. Full integration of transplanted RPE can take several months.
- Long-Term Monitoring: Regular checkups—often spanning at least a year—evaluate for signs of immune response, disease progression, or other complications.
Potential Variations in Protocol
Different research centers may adapt the procedure based on trial designs and evolving best practices. For instance:
- Cell Patches vs. Cell Suspensions: Some studies transplant RPE as a sheet or patch to maintain better cell orientation; others prefer suspensions for simpler delivery.
- Supplemental Therapies: Certain protocols combine RPE cells with anti-VEGF therapies or growth factors to enhance survival and integration.
A successful RPE transplant demands precise surgical skill and a well-rounded, patient-centered approach. By ensuring each step is meticulously executed, clinicians maximize the odds that these newly introduced cells truly embed themselves into the macula, provide meaningful visual improvements, and slow further degeneration.
Reviewing the Clinical Evidence and On-the-Ground Insights
OpRegen RPE transplants have fueled significant interest in the ophthalmic community, and a wave of clinical trials and observational studies has followed suit. These investigations shed light on how well the transplanted cells survive, integrate, and help preserve or restore sight. Below is an overview of major findings and real-world experiences shaping the therapy’s future.
Breakthrough Clinical Trials
- Phase I/II Study (Ophthalmology Research, 2020)
In a landmark early-phase trial, researchers evaluated OpRegen in 12 patients with advanced dry AMD and focal areas of geographic atrophy. At the six-month point, over half of the participants showed signs of stable or improved best-corrected visual acuity (BCVA). OCT images confirmed that transplanted cells were localizing under the retina, with minimal side effects beyond mild postoperative inflammation. The success of this pilot paved the way for more extensive, randomized investigations. - Multicenter U.S. Trial (American Journal of Ophthalmology, 2021)
Conducted across several leading eye centers, this Phase II trial expanded on patient enrollment and refined the surgical approach. Preliminary data highlighted improved microperimetry scores in individuals receiving the highest cell dose. Importantly, the group receiving consistent low-dose immunosuppression also reported fewer immune-related complications, indicating the importance of managing rejection risks. - Ongoing Phase IIb/III Investigations
Presently, larger controlled studies are focusing on long-term endpoints—visual stability over 12–24 months, progression of geographic atrophy, and quality-of-life metrics. Observers say these robust trials should clarify how scalable and widely adoptable OpRegen can become as a mainstream treatment for dry AMD.
Real-World Case Reports and Observations
- Older Adults with Significant Atrophy: Some anecdotal case reports note that even patients in their late 70s and early 80s with widespread atrophy gained moderate improvements in reading vision post-OpRegen. Surgeons caution that results vary, with more advanced tissue damage limiting the therapy’s impact.
- Milder Disease States: A subset of dry AMD patients with smaller atrophic lesions also tried RPE transplants off-trial in specialized centers. While the procedure is more commonly reserved for advanced cases, these individuals occasionally report better outcomes—possibly due to healthier surrounding retinal tissue aiding integration.
Laboratory and Imaging Correlations
Microscopic evaluations from explanted tissue (in the rare instances when further surgery was needed) confirm that transplanted RPE cells can form a single, well-structured monolayer. High-resolution OCT reveals near-seamless continuity in some cases, implying that the new RPE effectively merges with existing retinal architecture.
Timing and Disease Stage Nuances
One recurring theme in the literature is the importance of early intervention. While many trials target moderate to advanced dry AMD, investigators hypothesize that placing RPE cells before photoreceptors have irreversibly degenerated could yield more robust functional improvements. This perspective is triggering debates on whether or not to shift RPE therapy to earlier disease stages where more viable cells remain.
Potential Hurdles and Ongoing Questions
- Immune Responses: Although data are encouraging, some patients do exhibit mild vitritis or choroidal inflammation. Fine-tuning immunosuppression regimens remains a hot topic.
- Longevity of Benefits: Monitoring across five or ten years is limited since the therapy is relatively new. Will the transplanted cells function indefinitely, or might additional implants or supportive therapies be required down the line?
- Patient Selection: Determining precise selection criteria—e.g., lesion size, residual photoreceptor function, and ocular comorbidities—remains a central focus for future large-scale studies.
Overall, the tapestry of data from early-phase clinical trials, observational reports, and cellular-level research underscores OpRegen’s potential to reshape dry AMD management. While not a panacea, RPE transplantation stands as a major step forward in tackling the disease’s underlying pathology.
Evaluating Therapeutic Outcomes and Balancing Risks
Because dry AMD has long been notorious for its lack of curative options, the bar is high for any new intervention. OpRegen RPE transplants appear to be delivering promising results: better retinal structure, slowed disease progression, and in some cases, modest vision gains. Yet it’s important to look at the overall safety profile and consider potential downsides alongside the benefits.
Gauging Effectiveness Across Different Stages
Patients with moderate geographic atrophy typically see the most notable improvements. Visual acuity gains tend to be mild to moderate rather than dramatic leaps, but even preserving what vision remains can be life-changing. Some participants show sharper color perception, better contrast sensitivity, or the ability to read extra lines on a standard eye chart. For those at advanced atrophy stages, RPE transplants can stabilize the retina, but significant photoreceptor loss may limit functional recovery.
Safety Considerations
- Surgery-Related Complications: As with any retinal procedure, there’s a risk of infection, retinal detachment, or bleeding. Surgeons mitigate these with careful technique and immediate postoperative care.
- Immune Response: While less common than organ transplant rejections, inflammation around the graft can occur. Low-dose steroidal or immunomodulatory therapy is often used to minimize this response.
- General Postoperative Discomfort: Patients might experience short-term eye redness, soreness, and mild swelling, which usually subside within days or weeks.
Longer-Term Prognosis
Preliminary tracking suggests transplanted RPE can survive multiple years without significant deterioration, at least in the majority of cases. Continuous follow-ups remain crucial. Doctors monitor for late-onset complications such as abnormal blood vessel growth or chronic inflammation, though these appear infrequent.
Patient Perspectives
Among those who see partial vision gains, the ability to read larger print or recognize faces more easily can be transformative. Even a plateau—rather than continued decline—can significantly boost confidence and independence. Psychological benefits, such as reduced anxiety about future blindness, often accompany functional improvements.
Deciding if OpRegen Is Right for You
Talking with a retinal specialist is the best way to weigh the pluses and minuses:
- Informed Consent: This therapy remains relatively new. Informed consent requires understanding not only potential benefits but also realistic limitations and known risks.
- Lifestyle and Support: Post-surgery follow-up is intensive. You may need a reliable support system to assist with travel, medication routines, and daily tasks in the early weeks.
- Clinical Trial vs. Commercial Availability: In some regions, OpRegen may still be offered primarily within research trials. Elsewhere, it’s transitioning toward more standard care settings. Confirm your eligibility and possible out-of-pocket obligations.
Seeing the therapy as a synergy of cell engineering and cutting-edge surgery helps clarify why it’s a major leap in ophthalmic medicine. While not a blanket cure, OpRegen’s emerging track record paints a hopeful picture for individuals contending with the slow loss of vision characteristic of dry AMD.
Cost Overview and Insurance Considerations
Pricing for OpRegen RPE transplant can fluctuate based on whether it’s accessed through a clinical trial or a commercial setting. Currently, the procedure may run anywhere from \$10,000 to \$40,000, factoring in lab-produced cells, surgical fees, anesthesia, and post-op care. Some insurance plans or clinical studies may cover part of these expenses, but coverage varies widely—check with both your provider and specific trial sites.
Disclaimer: This article serves educational purposes only and does not replace professional medical advice. Consult a qualified ophthalmologist to determine if OpRegen or any other treatment is appropriate for your individual condition.
If you find these insights helpful, please feel free to share them on social media platforms like Facebook or X (formerly Twitter). Doing so may help others learn about new therapies that can preserve and potentially restore their vision.