What is Orbital Hemorrhage?
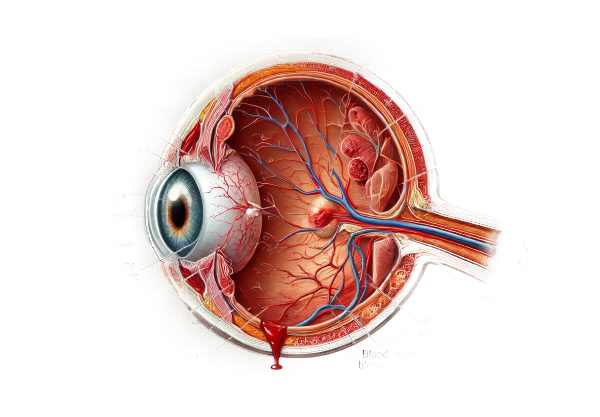
Orbital hemorrhage is a medical condition characterized by bleeding inside the orbit, the bony cavity that houses the eye. This condition can result from trauma, surgical complications, vascular malformations, or systemic diseases. Orbital hemorrhage can cause significant symptoms such as pain, swelling, bruising, and impaired vision, and if not treated promptly, it can lead to serious complications. Understanding orbital hemorrhage is critical for prompt diagnosis and treatment to avoid long-term ocular and systemic complications.
Detailed Investigation of Orbital Hemorrhage
Orbital hemorrhage is defined as bleeding in the area around the eye, which can be caused by a variety of factors. Hemorrhage can affect all of the bones, muscles, nerves, and blood vessels that make up the orbit. Understanding the causes, symptoms, and potential complications of orbital hemorrhage is critical for effective clinical management.
Types of Orbital Hemorrhages
- Retrobulbar Hemorrhage: Bleeding behind the eyeball causes increased intraorbital pressure. This type is especially dangerous because it can compress the optic nerve and cause rapid vision loss if not treated immediately.
- Subperiosteal Hemorrhage: Blood collects between the bone and the periosteum (the covering layer), which is frequently associated with trauma. This type can cause eye displacement, resulting in vision changes.
- Orbital Roof Hemorrhage: This type of bleeding occurs in the upper part of the orbit and is associated with fractures or intracranial trauma.
- Diffuse Orbital Hemorrhage: Generalized bleeding in the orbital tissues, usually caused by significant trauma or coagulopathy.
Causes and Risk Factors
Orbital hemorrhage can occur from a variety of causes, including:
- Trauma: The most common cause is blunt force trauma, which can result from sports injuries, car accidents, or physical altercations.
- Surgical Complications: Bleeding during or following orbital or sinus surgery.
- Vascular Disorders: Conditions such as arteriovenous malformations or aneurysms can result in spontaneous hemorrhage.
- Systemic Diseases: Blood disorders like hemophilia, leukemia, and anticoagulant therapy can predispose people to bleed.
- Infections: Severe infections can damage vessel walls, resulting in hemorrhage.
Symptoms
The appearance of orbital hemorrhage can differ depending on the extent and location of the bleeding:
- Pain: Severe, acute pain around the eye, frequently exacerbated by movement.
- Proptosis: An increase in pressure within the orbit causes the eye to bulge.
- Ecchymosis: Bruising around the eye, resulting in the distinctive “black eye” appearance.
- Visual Disturbances: The pressure on the optic nerve can cause blurred vision, double vision, or complete vision loss.
- Swelling: Significant swelling of the eyelids and surrounding tissues.
- Ophthalmoplegia: Limited eye movement due to swelling and muscle involvement.
- Chemosis is swelling of the conjunctiva (the membrane that covers the white part of the eye).
Pathophysiology
The pathophysiology of orbital hemorrhage involves bleeding from the orbital vasculature, which causes blood to accumulate in the confined orbital space. This accumulation raises intraorbital pressure, which can compress the optic nerve and other structures. The optic nerve is particularly susceptible to pressure, and prolonged compression can cause ischemia and irreversible damage, resulting in vision loss. The severity and rate of hemorrhage can have a significant impact on clinical outcomes.
Complications
If not treated properly, orbital hemorrhage can cause a number of serious complications.
- Permanent Vision Loss: Caused by sustained pressure on the optic nerve, resulting in ischemic optic neuropathy.
- Orbital Compartment Syndrome: A significant increase in intraorbital pressure necessitating emergency decompression.
- Infection: Secondary infections can develop, especially if the hemorrhage is associated with an open fracture or surgical site.
- Cosmetic Deformities: Prolonged swelling and fibrosis can result in visible disfigurement.
Differential Diagnosis
Distinguishing orbital hemorrhage from other conditions with similar symptoms is critical for accurate diagnosis.
- Orbital Cellulitis: An infection that causes similar symptoms of pain, swelling, and proptosis but is frequently accompanied by systemic signs of infection, such as fever.
- Orbital Fractures: Trauma can cause fractures with associated hemorrhage, necessitating imaging to distinguish.
- Thyroid Eye Disease: Thyroid dysfunction causes chronic swelling and proptosis, which usually develops gradually.
- Orbital Tumors: Proptosis and visual changes may occur, but they usually appear gradually.
Epidemiology
Orbital hemorrhage is uncommon but can occur in people of all ages, with a higher incidence in those who participate in high-risk activities such as contact sports or occupations with a risk of facial trauma. Individuals with underlying blood disorders or those taking anticoagulants may be more prone to the condition.
Understanding the complexities of orbital hemorrhage, such as its types, causes, symptoms, and potential complications, is critical for healthcare providers to accurately diagnose and manage this condition.
Methods for Diagnosing Orbital Hemorrhage
Orbital hemorrhage diagnosis requires a combination of clinical evaluation, imaging studies, and, in some cases, laboratory tests to confirm the diagnosis and determine the severity of the condition.
Clinical Evaluation
A thorough clinical evaluation is the first step in diagnosing orbital hemorrhage.
- Patient History: Provide a detailed history of the onset and nature of symptoms, as well as any recent trauma, surgeries, or underlying medical conditions that may predispose to bleeding.
- Physical Examination: Look for signs of orbital hemorrhage, such as proptosis, bruising, swelling, and limited eye movement. Evaluating visual acuity and pupillary responses to determine the effect on vision.
- Palpation: Assessing tenderness, swelling, and any palpable abnormalities in the orbital region.
Imaging Studies
Imaging is essential for confirming the diagnosis of orbital hemorrhage and understanding its extent.
- CT Scan (Computed Tomography) is the preferred imaging modality for orbital hemorrhage. CT scans produce detailed images of bony structures and can detect the presence and extent of blood accumulation in the orbit. They are especially useful in detecting associated fractures or structural damage.
- MRI (Magnetic Resonance Imaging): MRI provides superior soft tissue contrast and can be used to determine the extent of hemorrhage as well as the effects on the optic nerve and surrounding tissues. It is especially useful when the optic nerve is involved or the hemorrhage has spread intracranially.
- Ultrasound: Ocular ultrasound can be used in certain situations to assess the presence of hemorrhage and its effects on ocular structures. It is a non-invasive and quick diagnostic tool, but less detailed than CT or MRI.
Lab Tests
Laboratory tests may be required to identify the underlying causes or contributing factors to the hemorrhage.
- Complete Blood Count (CBC): To detect abnormalities in blood cell counts that may indicate an underlying hematologic disorder.
- Coagulation Profile: Includes PT, PTT, and INR to detect clotting abnormalities or the effects of anticoagulant therapy.
- Blood Chemistry: Check for systemic conditions that could cause bleeding, such as liver disease or renal insufficiency.
Orbital Hemorrhage Treatment
The severity and underlying cause of orbital hemorrhage determine the treatment options. Immediate and effective management is critical for avoiding complications like vision loss and permanent disfigurement. Treatment strategies range from conservative to surgical interventions, with emerging therapies providing new options for management.
Conservative Management
- Observation and Monitoring: In cases of mild orbital hemorrhage with no significant vision impairment or proptosis, careful observation and monitoring may be necessary. Patients should be closely monitored for any changes in symptoms or indications of a worsening condition.
- Cold Compresses: Applying cold compresses to the affected area can help reduce swelling and discomfort in the early stages after a hemorrhage.
- Pain Management: Nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen can be used to treat pain and inflammation. However, patients with coagulopathy or those on anticoagulant therapy should exercise caution when taking NSAIDs.
- Head Elevation: Keeping the head elevated can help relieve orbital pressure and swelling.
Medical Treatment
- Steroids: Corticosteroids may be prescribed in cases of severe inflammation and swelling to alleviate symptoms and prevent additional tissue damage.
- Antibiotics: If there is a risk of secondary infection, especially after trauma or surgery, prophylactic antibiotics may be given.
- Management of Underlying Conditions: It is critical to treat any underlying conditions that contribute to the hemorrhage, such as blood pressure control, anticoagulant therapy adjustment, or systemic disease management, such as diabetes.
Surgical Intervention
Surgery is necessary in cases of severe orbital hemorrhage where there is a significant risk of vision loss or other complications.
- Orbital Decompression: This procedure entails making an incision to relieve pressure on the orbit and drain accumulated blood. It is commonly used as an emergency measure to prevent optic nerve damage.
- Endoscopic Surgery: Orbital hemorrhages, particularly those involving the sinuses, can be accessed and treated using minimally invasive endoscopic techniques.
- Orbital Structure Repair: If there are associated fractures or structural damage, surgery may be required to restore normal anatomy and function.
Innovative and Emerging Therapies
- Angiographic Embolization: In cases of vascular malformations or aneurysms, angiographic embolization can be used to control bleeding. This minimally invasive procedure entails injecting materials to block bleeding vessels.
- Advanced Imaging Techniques: New imaging modalities, such as functional MRI, can provide detailed assessments of orbital structures and help guide targeted treatments.
- Regenerative Medicine: Research into regenerative therapies, such as stem cell treatments, shows promise for repairing damaged orbital tissues and improving outcomes in patients suffering from severe hemorrhage.
- Pharmacologic Innovations: New drugs targeting specific pathways involved in bleeding and inflammation are in the works, with the potential for more effective and targeted treatments.
Effective treatment of orbital hemorrhage necessitates a multidisciplinary approach that includes conservative management, medical therapy, and surgical intervention as needed. Innovative and emerging therapies continue to expand the treatment options for this complex condition.
Effective Methods for Improving and Avoiding Orbital Hemorrhage
- Protective Eyewear: Wear protective eyewear when participating in activities that pose a high risk of facial injury, such as sports, construction work, or handling hazardous materials.
- Seatbelt Use: Always wear a seatbelt when driving or riding in a vehicle to reduce the risk of facial trauma during an accident.
- Safe Environment: Ensure that your home and workplace are free of hazards that could cause falls or blunt force trauma to the face.
- Regular Medical Check-Ups: Regular health check-ups can assist in managing systemic conditions such as hypertension and diabetes, which can increase the risk of bleeding.
- Medication Management: If you are taking an anticoagulant, carefully follow your doctor’s instructions to avoid excessive bleeding and have your blood coagulation levels checked on a regular basis.
- Healthy Lifestyle: To improve overall vascular health and reduce the risk of hemorrhage, follow a healthy lifestyle that includes a balanced diet, regular exercise, and quitting smoking.
- Immediate Medical Attention: Seek immediate medical attention if you sustain any facial or ocular injuries to avoid complications like orbital hemorrhage.
- Avoid High-Risk Behaviors: Limit participation in high-risk activities and use appropriate safety precautions when they are unavoidable.
- Education and Awareness: Inform yourself and others about the risks and precautions for orbital hemorrhage in order to promote safer practices and environments.
Trusted Resources
Books
- “Orbital Disease: Imaging and Analysis” by Jack Rootman and A.D. Murray
- “Ocular Trauma: Principles and Practice” by Ferenc Kuhn
- “Manual of Oculoplastic Surgery” by Mark R. Levine
Online Resources
- American Academy of Ophthalmology (AAO): aao.org
- National Eye Institute (NEI): nei.nih.gov
- American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS): asoprs.org






