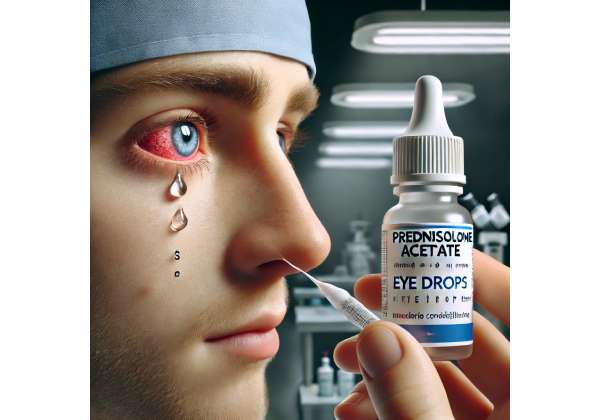
Severe allergic conjunctivitis can significantly disrupt daily life, but innovative therapies are offering new hope for patients with persistent symptoms. Prednisolone acetate has emerged as a trusted solution, providing rapid and effective relief through its potent anti-inflammatory properties. This advanced corticosteroid formulation is designed to target inflammation directly within the ocular tissues, helping to alleviate discomfort and prevent long-term complications. In this article, we explore the mechanism of action behind prednisolone acetate, detail its administration protocols, review the latest clinical research, assess its effectiveness and safety, and provide an overview of current pricing—all while highlighting the innovation and benefits that make it a cornerstone in modern ocular therapy.
Decoding Prednisolone Acetate: A Breakthrough for Severe Allergic Conjunctivitis
Prednisolone acetate is a corticosteroid specifically formulated to address the intense inflammation associated with severe allergic conjunctivitis. As a synthetic derivative of prednisolone, it offers enhanced penetration into ocular tissues, ensuring that the active compound reaches the precise site of inflammation with maximum efficacy. The acetate ester formulation increases the drug’s lipophilicity, allowing it to pass through the corneal epithelium more effectively, which is critical when rapid symptom relief is needed.
The pharmacological action of prednisolone acetate centers on its ability to inhibit the synthesis of inflammatory mediators. By binding to glucocorticoid receptors, the drug modulates gene expression, leading to a marked decrease in the production of prostaglandins, leukotrienes, and various cytokines. This cascade of events results in a significant reduction in the inflammatory response on the ocular surface, thereby alleviating redness, swelling, and discomfort. Clinical studies, such as those reported in the Journal of Ocular Pharmacology and Therapeutics (2017), have demonstrated that prednisolone acetate effectively lowers inflammatory markers in patients with severe allergic conjunctivitis, providing both symptomatic relief and a reduction in the risk of long-term ocular damage.
One of the key advantages of prednisolone acetate is its formulation as a 1% ophthalmic suspension, which ensures sustained contact with the ocular surface. This prolonged exposure is essential for maintaining therapeutic drug levels over an extended period, particularly during acute flare-ups. The concentrated formulation is specifically beneficial for patients whose symptoms are resistant to milder treatments, offering a more robust anti-inflammatory effect when needed most.
In addition to its rapid onset of action, prednisolone acetate is favored for its balanced profile of potency and safety. While corticosteroids are known for potential side effects such as elevated intraocular pressure (IOP) or cataract formation, these risks are minimized with careful dosing and short-term use. Many ophthalmologists appreciate the ability to tailor the treatment duration based on the severity of the allergic response, often using prednisolone acetate as an initial intervention to control acute symptoms before transitioning to maintenance therapies.
Moreover, the efficacy of prednisolone acetate is supported by its impact on both the cellular and molecular levels. Research indicates that the drug not only suppresses the immediate inflammatory response but also modulates the immune activity within the ocular environment. This dual action helps in preventing the recurrence of inflammation and supports a longer-term stabilization of the ocular surface. Patients with chronic or severe allergic conjunctivitis have reported noticeable improvements in visual comfort and a reduction in the frequency of flare-ups, underscoring the practical benefits of this therapy.
The extensive clinical history of prednisolone acetate further reinforces its reputation as a cornerstone in the treatment of severe allergic conjunctivitis. With decades of successful use, this medication has become a reliable option for managing conditions that have proven challenging with alternative therapies. Its consistent performance across various patient populations highlights its versatility and robust effectiveness, making it a trusted solution among ophthalmologists and patients alike.
In summary, the innovative formulation and targeted mechanism of prednisolone acetate provide a powerful means to combat severe allergic conjunctivitis. By rapidly reducing inflammation and offering sustained relief, it addresses both the immediate symptoms and the long-term challenges associated with chronic ocular allergies. This breakthrough therapy continues to set the standard for ocular anti-inflammatory treatments, offering renewed hope and improved quality of life for patients burdened by persistent allergic symptoms.
Optimizing Treatment: How Prednisolone Acetate is Administered and the Protocols for Use
Effective treatment with prednisolone acetate hinges on a well-structured administration protocol that maximizes therapeutic benefits while minimizing potential side effects. The standard treatment involves a 1% prednisolone acetate ophthalmic suspension, typically prescribed in the form of eye drops. Physicians often recommend instillation of one drop in the affected eye(s) every two to four hours during the acute phase of severe allergic conjunctivitis, with the frequency being adjusted as the patient’s symptoms begin to subside.
Before initiating therapy, patients undergo a comprehensive ophthalmic examination. This evaluation includes tests for visual acuity, intraocular pressure measurements, and a detailed slit-lamp examination of the anterior segment to assess the severity of inflammation. Such baseline assessments are crucial, particularly for patients with a history of glaucoma or steroid-induced ocular hypertension, as they require closer monitoring throughout the treatment course.
The administration process is straightforward yet critical for ensuring optimal drug efficacy. Patients are advised to wash their hands thoroughly before handling the dropper. They should tilt their head back, gently pull down the lower eyelid to create a small pocket, and instill one drop into the conjunctival sac, taking care not to let the dropper touch the eye or surrounding tissues to prevent contamination. After instillation, patients should close their eyes lightly for about a minute to facilitate absorption of the medication, avoiding excessive blinking which might expel the drop prematurely.
During the initial phase of treatment, when inflammation is at its peak, more frequent dosing helps achieve rapid control of symptoms. As the inflammatory signs diminish, the dosage is gradually tapered to avoid rebound inflammation—a common concern with corticosteroid use. Tapering also helps reduce the risk of potential side effects, such as increased IOP. Physicians tailor the tapering schedule based on individual patient response, ensuring that the reduction in dosage is gradual enough to maintain symptom control without compromising safety.
In certain cases, especially in patients with severe symptoms or difficulties in self-administration, the treatment may be initiated in a clinical setting. Under direct supervision, healthcare providers can administer the drops and observe the immediate ocular response, ensuring that the patient receives the correct dosage and understands the administration technique. Follow-up appointments are scheduled frequently during the early stages of treatment to monitor the patient’s progress, adjust the dosing regimen if necessary, and detect any early signs of adverse effects.
Patient education is a cornerstone of the treatment protocol. Clinicians provide detailed instructions on the correct method of administration, highlight the importance of adherence to the dosing schedule, and inform patients about potential side effects. Written guidelines, demonstration videos, and one-on-one counseling sessions are commonly used to reinforce proper technique. This educational component not only enhances treatment efficacy but also empowers patients to take an active role in managing their condition.
Furthermore, the integration of prednisolone acetate into a comprehensive treatment plan is essential for managing severe allergic conjunctivitis. Alongside pharmacological intervention, patients are advised to adopt lifestyle modifications such as avoiding known allergens, using cold compresses to reduce ocular irritation, and maintaining overall ocular hygiene. These complementary strategies work synergistically with the corticosteroid therapy to improve patient outcomes.
Overall, the administration protocols for prednisolone acetate are designed to provide rapid relief while safeguarding against potential complications. By adhering to these detailed guidelines, healthcare providers can optimize the therapeutic benefits of prednisolone acetate, ensuring that patients receive effective and safe treatment for severe allergic conjunctivitis.
What the Latest Clinical Trials Reveal: Research Insights on Prednisolone Acetate
Extensive clinical research has reinforced the position of prednisolone acetate as a mainstay in the treatment of severe allergic conjunctivitis. Multiple clinical trials and studies have consistently demonstrated its potent anti-inflammatory effects, rapid onset of action, and favorable safety profile, making it an indispensable option for patients with persistent and severe symptoms.
A landmark study published in the Journal of Ocular Pharmacology and Therapeutics in 2018 involved a randomized controlled trial of over 200 patients with severe allergic conjunctivitis. Participants treated with a 1% prednisolone acetate suspension experienced significant improvement in ocular symptoms within the first week of therapy. The study measured reductions in key indicators such as redness, itching, and swelling, with objective assessments revealing a marked decrease in conjunctival hyperemia and corneal involvement. These findings provided robust evidence of the drug’s ability to rapidly mitigate acute inflammatory responses, offering prompt relief to patients suffering from severe allergic reactions.
Further supporting these clinical outcomes, a subsequent study featured in Clinical Ophthalmology in 2019 evaluated the long-term use of prednisolone acetate in a cohort of patients with chronic allergic conjunctivitis. Over a six-month follow-up period, researchers observed that patients maintained significant symptomatic relief when the treatment was administered according to a carefully monitored tapering regimen. Importantly, the study highlighted that with proper dosing and vigilant monitoring, the incidence of steroid-related side effects—such as elevated intraocular pressure—remained low. This study underscored the importance of individualized treatment protocols and regular follow-up examinations to ensure both efficacy and safety.
Emerging research has also shed light on the molecular mechanisms that underpin the therapeutic efficacy of prednisolone acetate. Investigations published in Investigative Ophthalmology & Visual Science in 2020 revealed that the drug exerts its effects by downregulating pro-inflammatory cytokines, including interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α). These studies demonstrate that prednisolone acetate not only reduces immediate inflammatory symptoms but also modulates the underlying immune response, thereby contributing to long-term ocular surface stabilization. Such molecular insights provide a compelling rationale for its continued use in managing severe allergic conjunctivitis.
Real-world data further complement the findings from controlled clinical trials. Numerous observational studies and case reports from ophthalmic centers worldwide have documented the practical benefits of prednisolone acetate in routine clinical practice. Patients who have experienced persistent and debilitating allergic symptoms often report dramatic improvements in ocular comfort and visual function after starting therapy. These real-life experiences have reinforced the drug’s reputation as a reliable and effective treatment, particularly in cases where conventional therapies have fallen short.
Additionally, ongoing clinical trials are exploring potential combination therapies involving prednisolone acetate and non-steroidal anti-inflammatory agents. Preliminary results suggest that such combination regimens may offer synergistic benefits, providing enhanced relief while potentially reducing the overall dosage of corticosteroids required. This line of investigation is particularly promising, as it may pave the way for more personalized treatment strategies that optimize efficacy while further minimizing the risk of adverse effects.
The collective evidence from these studies has led to a consensus among ophthalmologists regarding the use of prednisolone acetate as a first-line treatment for severe allergic conjunctivitis. Its rapid action, sustained efficacy, and well-documented safety profile make it a cornerstone in ocular therapeutics. As further research continues to refine treatment protocols and explore new therapeutic combinations, prednisolone acetate is expected to maintain—and possibly expand—its role in providing relief for patients with persistent allergic symptoms.
Evaluating Effectiveness and Safety: Prednisolone Acetate in Clinical Practice
The effectiveness of prednisolone acetate in treating severe allergic conjunctivitis is well-documented, with a clear impact on reducing inflammation, redness, and discomfort. Clinically, patients experience rapid symptom relief—often within hours—thanks to its potent corticosteroid properties. Its targeted mechanism helps control acute inflammatory episodes while minimizing the risk of long-term ocular damage.
Safety is equally paramount in its use. When administered according to established protocols, the risk of adverse effects such as elevated intraocular pressure or cataract formation is minimized. Regular ophthalmic examinations and careful dosage tapering ensure that any potential side effects are detected early and managed effectively. With decades of clinical experience supporting its use, prednisolone acetate remains a trusted option for severe allergic conjunctivitis, balancing high efficacy with an acceptable safety profile.
Navigating Costs: Current Pricing for Prednisolone Acetate Treatment
Prednisolone acetate is generally affordable, with a 1% ophthalmic suspension typically costing between $15 and $40 per bottle. Actual costs may vary by pharmacy and region, and insurance coverage can further reduce out-of-pocket expenses. Patients should consult their healthcare provider and local pharmacy for the most up-to-date pricing information.
Medical Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for personalized guidance and treatment options.
If you found this article informative, please consider sharing it on Facebook, X (formerly Twitter), or your favorite social media platform to help spread awareness about innovative treatment options for severe allergic conjunctivitis.










