What is gonococcal conjunctivitis?
Gonococcal conjunctivitis is a severe and acute bacterial eye infection caused by Neisseria gonorrhoeae, which is also responsible for the sexually transmitted infection gonorrhea. This condition most commonly affects newborns (neonatal conjunctivitis) and sexually active adults. If left untreated, gonococcal conjunctivitis can result in serious complications such as corneal perforation and blindness. Rapid diagnosis and treatment are critical to avoiding long-term damage and ensuring a positive outcome. The infection is extremely contagious and requires immediate medical attention.
Clinical Features of Gonococcal Conjunctivitis
Gonococcal conjunctivitis is a type of bacterial conjunctivitis that is especially severe and necessitates immediate medical attention. Understanding its pathophysiology, risk factors, clinical presentation, and potential complications is critical for successful treatment and prevention.
Pathophysiology
Neisseria gonorrhoeae is a gram-negative diplococcus that infects mucous membranes in the genital tract, rectum, and throat. This bacterium infects the conjunctiva, causing severe inflammation and purulent discharge. The infection can spread through direct contact with infected genital secretions, making neonates and sexually active adults especially vulnerable.
In newborns, the infection is usually contracted during passage through an infected birth canal, resulting in neonatal conjunctivitis, also known as ophthalmia neonatorum. Adults can become infected through direct contact with infected genital secretions, either from themselves or from a sexual partner.
Clinical Presentation
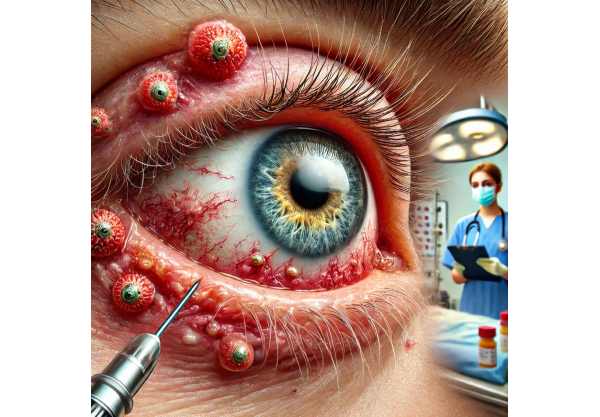
Gonococcal conjunctivitis has unique and severe symptoms that distinguish it from other types of conjunctivitis:
- Rapid Onset: Symptoms develop quickly, usually within 1-3 days of exposure.
- Severe Hyperemia: The conjunctiva becomes very red and inflamed.
- Profuse Purulent Discharge: A thick, yellow-green discharge that can be copious and continuous, causing crusting of the eyelids and difficulty opening them.
- Swelling of the Eyelids: Severe eyelid edema that can cause significant discomfort and vision problems.
- Pain and Discomfort: Patients frequently report severe pain, irritation, and a feeling of grittiness in the affected eye.
- Photophobia: Light sensitivity is common as a result of the severe inflammation.
- Preauricular Lymphadenopathy: Swelling of lymph nodes near the ear may occur.
Risk Factors
Several factors boost the
Risk of getting gonococcal conjunctivitis:
- Neonates: Newborns are especially vulnerable if their mothers have untreated gonorrhea during childbirth. Pregnant women who receive routine gonorrhea screening and treatment are significantly less likely to develop the disease.
- Sexually Active Adults: People who have multiple sexual partners or engage in unprotected sex are at a higher risk. Men who have sex with men (MSM) are also more likely to contract gonorrhea.
- Previous Sexually Transmitted Infections (STIs): Having a history of other STIs, such as chlamydia or syphilis, increases the risk of gonococcal infection.
- Poor Hygiene Practices: Poor personal hygiene and improper handwashing can promote the spread of Neisseria gonorrhoeae to the eyes, particularly through self-inoculation.
- Immunocompromised State: People with weakened immune systems, such as HIV/AIDS patients, are more vulnerable to infections like gonococcal conjunctivitis.
Complications
If not treated promptly, gonococcal conjunctivitis can cause severe complications, including permanent vision loss.
- Corneal Ulceration and Perforation: The intense inflammatory response can cause corneal ulcers, which can progress to perforation. This is a vision-threatening condition that requires immediate surgical intervention.
- Blindness: Severe corneal damage from ulceration or perforation can cause irreversible blindness.
- Secondary Infections: The damaged ocular surface is more vulnerable to secondary bacterial or fungal infections, which complicates treatment and recovery.
- Systemic Spread: In neonates, gonococcal conjunctivitis can progress to disseminated gonococcal infection, which can affect multiple organ systems and be fatal.
- Chronic Conjunctivitis: Persistent inflammation can result in chronic conjunctivitis, which causes long-term discomfort and vision problems.
Pathogenesis
Neisseria gonorrhoeae binds to the mucosal surfaces of the eye via pili and outer membrane proteins. The bacteria then invade and multiply in the epithelial cells, causing an intense inflammatory response. The release of pro-inflammatory cytokines and chemokines attracts neutrophils to the infection site, producing the characteristic purulent discharge. Bacteria can also produce enzymes that degrade the extracellular matrix, allowing tissue invasion and damage.
Prevention
Preventing gonococcal conjunctivitis entails taking measures to reduce the incidence of gonorrhea and protect newborns at birth:
- Prenatal Screening and Treatment: Pregnant women can avoid neonatal conjunctivitis by routinely screening for gonorrhea and treating it with appropriate antibiotics on time.
- Prophylactic Eye Drops for Newborns: To prevent ophthalmia neonatorum, prophylactic antibiotic eye drops or ointment, such as erythromycin, are administered immediately after birth.
- Safe Sexual Practices: Consistent and proper condom use, limiting the number of sexual partners, and regular STI screenings can all help reduce the risk of gonorrhea and subsequent gonococcal conjunctivitis.
- Education and Awareness: Public health initiatives to raise awareness about gonorrhea, its transmission, and prevention strategies are critical to lowering the incidence of this infection.
Understanding the specific pathophysiology, risk factors, and potential complications of gonococcal conjunctivitis emphasizes the importance of early detection, prompt treatment, and preventive measures in managing this serious ocular condition.
Gonococcal Conjunctivitis Diagnosis Tools
Accurate diagnosis of gonococcal conjunctivitis is critical for successful treatment and avoiding complications. A clinical examination, laboratory tests, and imaging studies are typically used to confirm the presence of Neisseria gonorrhoeae and determine the extent of ocular involvement.
Clinical Examination
- History and Symptoms: It is critical to obtain a complete patient history, including recent sexual activity, urethritis or cervicitis symptoms, and neonatal background. Gonococcal conjunctivitis symptoms include rapid onset of purulent discharge, severe redness, and swelling of the eyelids.
- Physical Examination: A thorough examination of the eyes with a slit lamp to determine the severity of conjunctival inflammation, discharge, corneal involvement, and any signs of corneal ulceration or perforation.
Lab Tests
- Gram Stain: A Gram stain of the purulent discharge can provide a quick preliminary diagnosis. Neisseria gonorrhoeae is detected as gram-negative diplococci within polymorphonuclear leukocytes.
- Culture: The best way to diagnose gonococcal conjunctivitis is to culture the conjunctival swab on selective media like Thayer-Martin agar. This method uses antibiotic sensitivity testing to guide treatment.
- Nucleic Acid Amplification Tests (NAATs): NAATs are a highly sensitive and specific method for detecting Neisseria gonorrhoeae DNA or RNA in conjunctival samples. These tests produce quick results and can confirm the diagnosis even when bacterial counts are low.
- Polymerase Chain Reaction (PCR): PCR testing of conjunctival swabs is another quick and dependable way to detect gonococcal DNA. It is especially useful in situations where cultures are difficult to obtain or delayed.
Ancillary tests
- Corneal Staining: Using fluorescein dye to stain the cornea can aid in the detection of ulcers or epithelial defects. This test is critical for determining the risk of corneal perforation.
- Ocular Ultrasound: In cases of severe eyelid swelling or suspected complications, ocular ultrasound can reveal important information about the globe’s integrity and the presence of any intraocular involvement.
- Systemic Screening: Neonates and sexually active adults should be screened for other sexually transmitted infections (STIs) such as chlamydia, syphilis, and HIV. Co-infections are common and necessitate simultaneous treatment.
Advanced Treatments for Gonococcal Conjunctivitis
Because Neisseria gonorrhoeae is highly infectious and has the potential to rapidly progress to severe complications, gonococcal conjunctivitis must be treated promptly and aggressively. Treatment consists of both local and systemic antibiotic therapy, supportive care, and prevention measures to prevent transmission.
- Systemic Antibiotics: – Ceftriaxone: The standard treatment for gonococcal infections is a single intramuscular dose of ceftriaxone. This antibiotic is extremely effective against Neisseria gonorrhoeae and is the recommended systemic treatment for gonococcal conjunctivitis.
• Azithromycin: In addition to ceftriaxone, azithromycin is frequently given orally to treat potential co-infection with Chlamydia trachomatis, which frequently coexists with gonorrhea infections. - Topical Antibiotics: – Erythromycin Ointment: Apply multiple times daily to the affected eye to reduce bacterial load and prevent spread.
- Fluoroquinolones: Topical fluoroquinolones, such as moxifloxacin, are effective against Neisseria gonorrhoeae and can be used alongside systemic antibiotics.
- Supportive Care: – Saline Irrigation: Regular saline irrigation clears purulent discharge and reduces bacterial load in the eyes.
- Pain Management: Analgesics and anti-inflammatory drugs may be prescribed to relieve pain and inflammation.
- Hospitalization: Severe cases of gonococcal conjunctivitis, particularly those with corneal ulcers or risk of perforation, may necessitate hospitalization for intensive monitoring and treatment.
Innovative and Emerging Therapies
- Combination Antibiotic Therapy: To combat antibiotic-resistant strains of Neisseria gonorrhoeae, researchers are investigating combination antibiotic therapy to improve efficacy and reduce resistance development.
- New Antibiotics: – New antibiotic classes are being researched for potential effectiveness against resistant Neisseria gonorrhoeae strains. These include new cephalosporins and macrolides.
- Immunotherapy: – Immunotherapy treatments aim to enhance the immune response to Neisseria gonorrhoeae, potentially complementing traditional antibiotics.
- Adjunctive Treatments: – Probiotics are being studied to support antibiotic therapy and maintain eye surface health.
Gonococcal conjunctivitis is effectively managed by combining prompt antibiotic treatment, supportive care, and prevention measures to avoid transmission. Emerging therapies and ongoing research are helping to improve outcomes and address issues like antibiotic resistance.
Tips to Prevent Gonococcal Conjunctivitis
- Practice Safe Sex: – Use condoms correctly during all sexual activities to prevent contracting and spreading Neisseria gonorrhoeae and other STIs.
- Regular STI Screenings: – Regular screenings for STIs, including gonorrhea, are critical for sexually active people, especially those who have multiple partners. Early detection and treatment can stop the spread of infections.
- Prenatal Care: – Pregnant women should receive regular STI screenings and treatment as needed. Preventive measures, such as giving newborns prophylactic antibiotic eye drops, can help reduce the risk of neonatal conjunctivitis.
- Hygiene Practices: – Practice good personal hygiene, such as regular handwashing, to prevent self-inoculation and the spread of bacteria from infected areas to the eyes.
- Avoid Sharing Personal Items: – Towels, washcloths, and eye makeup can spread Neisseria gonorrhoeae and other pathogens.
- Education and Awareness: – Use public health campaigns and education programs to raise awareness about the symptoms, transmission, and prevention of gonorrhea and gonococcal conjunctivitis.
- Prompt Treatment: Seek medical attention immediately if symptoms of gonococcal conjunctivitis or other STIs are suspected. Early treatment is critical to avoiding complications and transmission.
- Partner Notification and Treatment: – If diagnosed with gonorrhea, notify sexual partners so they can be tested and treated to prevent further spread of the infection.
- Avoid Risky Behaviors: – Minimize risky sexual behaviors, such as having multiple partners or engaging in unprotected sex, to reduce the risk of infection.
Individuals who follow these preventive measures have a significantly lower risk of contracting and spreading gonococcal conjunctivitis and other sexually transmitted infections.
Trusted Resources
Books
- “Ocular Infection” by Tarek Shaarawy, Deepak P. Edward, and Roger A. Hitchings
- “The Sanford Guide to Antimicrobial Therapy” by David N. Gilbert, Henry F. Chambers, and Michael S. Saag
- “Neonatal and Pediatric Ophthalmology” by Robison D. Harley and Leonard B. Nelson






