What is pseudophakia?
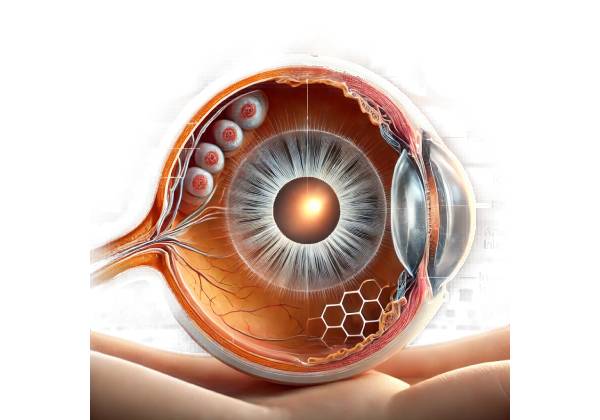
Pseudophakia is the condition of having an artificial intraocular lens (IOL) implanted in the eye following the removal of the natural lens during cataract surgery. The term comes from Greek, where “pseudo” means false and “phakia” refers to a lens. Thus, pseudophakia literally means “false lens.” This condition is a common and highly effective side effect of cataract surgery, which is one of the most commonly performed surgical procedures worldwide.
The Natural Lens and Cataracts
The natural lens of the eye is a transparent, biconvex structure that sits behind the iris and pupil. It focuses light on the retina, allowing us to see clearly from a variety of distances. Over time, due to aging or other factors, the natural lens can become cloudy, resulting in a condition known as a cataract. Cataracts cause blurred vision, glare, difficulty seeing at night, and can significantly impair daily activities if not treated.
The Evolution of Cataract Surgery
Cataract surgery has changed dramatically over the centuries. Early procedures, such as couching, involved displacing the clouded lens within the eye, but they were risky and frequently ineffective. The development of extracapsular cataract extraction (ECCE) in the twentieth century, which involves removing the lens while leaving the lens capsule intact, paved the way for the use of IOLs.
The introduction of phacoemulsification, a technique that uses ultrasonic vibrations to emulsify the cataract before removal, transformed cataract surgery by making it safer, more efficient, and enabling smaller incisions. This technique is now considered standard in modern cataract surgery.
Intraocular Lens (IOL)
Intraocular lenses are artificial lenses placed in the eye to replace the natural lens that was removed during cataract surgery. These lenses are made of biocompatible materials like acrylic, silicone, or polymethyl methacrylate (PMMA) and are intended to stay in the eye permanently. There are several types of IOLs, each with its own benefits and indications:
- Monofocal IOLs: These lenses have a single fixed focus distance, usually set for clear distance vision. Patients may still require glasses for near tasks, such as reading.
- Multifocal IOLs: These lenses have multiple focal points, which improves distance, intermediate, and near vision. They can reduce the need for glasses, but they may produce glare and halos, particularly at night.
- Accommodative IOLs: These lenses, designed to mimic the natural lens’s ability to change shape and focus at different distances, provide better intermediate and close vision. However, their effectiveness varies by individual.
- Toric IOLs: Designed specifically for patients with astigmatism, toric IOLs correct this refractive error and provide clear vision at a specific focal distance.
Benefits of Pseudophakia
Pseudophakia provides numerous advantages, significantly improving the quality of life for people who have had cataract surgery:
- Vision Restoration: By replacing the clouded natural lens with a clear IOL, patients’ vision improves significantly, with visual acuity often restored to pre-cataract levels or better.
- Reduced Requirement for Glasses: Depending on the type of IOL implanted, many patients discover that they require glasses less frequently or not at all for certain activities.
- Improved Quality of Life: Better vision enables patients to resume daily activities like reading, driving, and engaging in hobbies with greater ease and confidence.
- Long-Term Solution: Because IOLs are designed to last a lifetime, pseudophakia is a long-lasting and effective vision restoration option.
Potential Complications and Considerations
While pseudophakia is generally safe and effective, there are some potential complications and considerations:
- Posterior Capsule Opacification (PCO): Also known as “secondary cataract,” PCO develops when the lens capsule, which is left intact during surgery to support the IOL, becomes cloudy. A YAG laser capsulotomy is a quick and painless procedure that can restore clear vision.
- IOL dislocation: In rare cases, the IOL may shift out of its intended position, resulting in blurred vision and the need for surgical repositioning.
- Glare and Halos: Some patients, particularly those with multifocal IOLs, may experience glare and halos when near lights, especially at night.
- Dry Eye: Cataract surgery can worsen dry eye symptoms in some patients, necessitating the use of lubricating eye drops or other treatments.
- Endophthalmitis: Endophthalmitis is a rare but serious infection that can develop after cataract surgery and requires immediate treatment to avoid severe vision loss.
Pseudophakia in Special Populations
Certain populations may have specific considerations for pseudophakia:
- Pediatric Patients: Although cataracts are less common in children, they do occur and may necessitate IOL implantation. Pediatric pseudophakia presents unique challenges, including the need to adjust the IOL power as the eye grows.
- Patients with Ocular Comorbidities: Patients with other eye conditions, such as glaucoma or diabetic retinopathy, may require specialized surgical approaches and meticulous postoperative care to achieve the best results.
- Refractive Lens Exchange: Some people without cataracts choose to have lens replacement surgery to correct refractive errors and reduce their reliance on glasses or contact lenses. This elective procedure, similar to cataract surgery, results in pseudophakia.
The Future of Pseudophakia
Technological advancements continue to improve patient outcomes and options for cataract surgery. Innovative IOL design features, such as extended depth of focus (EDOF) lenses and customizable light-adjustable lenses, improve visual outcomes and patient satisfaction. Furthermore, advances in surgical techniques and preoperative diagnostics improve the safety and efficacy of pseudophakia.
Pseudophakia Diagnostic Approaches
Pseudophakia is diagnosed through a combination of clinical evaluation, imaging studies, and specialized tests to ensure proper intraocular lens (IOL) placement and function, as well as monitoring for potential complications. Common diagnostic methods include the following:
Clinical Examination
- Visual Acuity Testing: This is the initial step in determining the visual outcomes of pseudophakia. Standard eye charts are used to assess the clarity of vision at various distances, assisting in determining the effectiveness of the implanted IOL.
- Slit-Lamp Examination: A slit-lamp microscope provides a close-up view of the eye’s anterior segment, which includes the cornea, iris, and lens. This examination aids in determining the position of the IOL, looking for signs of inflammation, and detecting any abnormalities.
- Fundus Examination: The fundus examination uses ophthalmoscopy to evaluate the health of the retina and optic nerve. It is critical for detecting any retinal issues that may affect visual outcomes following surgery.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic nerve. It detects any retinal edema, macular holes, or other retinal pathologies that could impair vision.
- Ultrasound Biomicroscopy (UBM) provides high-resolution imaging of anterior segment structures, including the IOL. It is useful for determining the position of the IOL and detecting complications such as dislocation or capsular opacification.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT focuses on the anterior segment of the eye, providing detailed views of the cornea, anterior chamber, and IOL. It aids in determining the IOL’s position and detecting anterior segment abnormalities.
Specialized Tests
- Corneal Topography: This test determines the curvature of the cornea, which is critical for detecting changes in corneal shape that may affect visual acuity. It is especially beneficial for patients with toric IOLs to ensure proper alignment.
- Wavefront Aberrometry: Wavefront aberrometry detects optical aberrations in the eye and provides detailed information about vision quality. It aids in determining the performance of multifocal and accommodative IOLs, resulting in optimal visual outcomes.
- Specular Microscopy: This test examines the corneal endothelium and is useful for monitoring corneal health after surgery. It aids in detecting any endothelial cell loss or dysfunction that may impair corneal clarity and vision.
Monitor for Complications
Regular follow-up visits are required to monitor for potential complications associated with pseudophakia.
- Posterior Capsule Opacification (PCO): Look for signs of PCO, which can be treated with a YAG laser capsulotomy if needed.
- Intraocular Pressure (IOP) Measurement: Regular IOP checks are essential for detecting any changes that could indicate complications such as glaucoma.
- Assessment of Visual Function: Ongoing evaluation of visual function, including contrast sensitivity and glare testing, helps ensure that the patient achieves the best visual outcomes and detects any problems early.
Pseudophakia Management
Managing pseudophakia primarily entails regular monitoring to ensure that the intraocular lens (IOL) is correctly positioned and functional, as well as addressing any complications that may arise following surgery. While the initial surgical procedure for cataract removal and IOL implantation is usually successful, follow-up care is required to maintain optimal visual outcomes and address any issues that arise.
Regular monitoring
- Follow-Up Appointments: Following cataract surgery, patients should attend follow-up appointments scheduled by their ophthalmologist. These visits are critical for determining the position and stability of the IOL, as well as monitoring the health of the anterior and posterior segments of the eye.
- Visual Acuity Testing: Regular visual acuity tests help to ensure that the patient’s vision remains clear and that the IOL is providing the necessary level of correction.
- Intraocular Pressure (IOP) Checks: Regular IOP measurements are critical for detecting pressure-related issues that may indicate glaucoma or other complications.
- Slit-Lamp Examination: This thorough examination allows the ophthalmologist to examine the IOL, anterior chamber, and any other structures that could indicate complications such as inflammation or lens dislocation.
Addressing Complications
- Posterior Capsule Opacification (PCO) is a common complication in which the lens capsule becomes cloudy, resulting in decreased vision. This is treatable with a YAG laser capsulotomy, a quick and painless procedure that uses a laser to create a small opening in the cloudy capsule, restoring clear vision.
- IOL Dislocation: In rare cases, the IOL can shift out of position, resulting in blurred vision. To resolve this issue, surgical repositioning or IOL replacement may be required.
- Glare and Halos: Some patients, particularly those with multifocal or accommodative IOLs, may notice glare and halos around lights. While these symptoms usually subside over time, patients who are experiencing significant discomfort may benefit from additional interventions such as anti-glare lenses or, in severe cases, IOL exchange.
- Dry Eye: Cataract surgery may worsen dry eye symptoms. Lubricating eye drops, warm compresses, and prescription medications may be used to improve tear production.
- Endophthalmitis: Although uncommon, endophthalmitis is a severe infection that can develop following cataract surgery. To avoid severe vision loss, prompt antibiotic treatment and, if necessary, surgical intervention are required.
Lifestyle and Visual Aids
- Glasses and Contact Lenses: While many patients have good vision with their IOLs, some may still need glasses or contact lenses for certain tasks, particularly if they have monofocal IOLs. Regular eye exams can help determine whether you need corrective lenses.
- Sunglasses: Protecting the eyes from UV light is critical to overall eye health. Patients should wear sunglasses with adequate UV protection to avoid eye damage and discomfort from bright light.
- Visual Rehabilitation: Visual rehabilitation programs can help patients with significant visual changes or complications maximize their remaining vision and improve their quality of life.
Advanced Interventions
- Refractive Lens Exchange (RLE): For patients without cataracts who want to reduce their reliance on glasses or contact lenses, RLE involves replacing the natural lens with an intraocular lens (IOL). This elective procedure can correct refractive errors, but it requires the same postoperative care and monitoring as traditional cataract surgery.
- Enhanced IOLs: Advances in IOL technology continue to give patients new options. Extended depth of focus (EDOF) lenses, for example, provide a broader range of clear vision and may further reduce the need for glasses. Light-adjustable lenses (LALs) enable post-operative adjustments to fine-tune vision outcomes.
Patient Education
It is critical to educate patients about the importance of postoperative care, recognize signs of complications, and understand the limitations and benefits of their IOLs in order to ensure successful management. Patients should be encouraged to have regular eye exams and to notify their ophthalmologist immediately if their vision changes.
Trusted Resources and Support
Books
- “Cataract Surgery: A Patient’s Guide to Cataract Treatment” by David F. Chang: This book provides comprehensive information on cataract surgery, including the implantation of intraocular lenses and postoperative care for pseudophakia.
- “The Ophthalmology Examinations Review” by Tien Yin Wong: This resource is valuable for both patients and healthcare providers, offering detailed explanations of various ocular conditions, including pseudophakia, and their management.
Organizations
- American Academy of Ophthalmology (AAO): The AAO offers extensive resources, guidelines, and continuing education for ophthalmologists and patients dealing with cataract surgery and pseudophakia. AAO Website
- National Eye Institute (NEI): Part of the National Institutes of Health, the NEI conducts and supports research on eye diseases and provides comprehensive educational resources on cataracts, IOLs, and pseudophakia. NEI Website
- American Society of Cataract and Refractive Surgery (ASCRS): The ASCRS provides information and resources for patients undergoing cataract and refractive surgeries, including details on the latest advancements in IOL technology. ASCRS Website






