Exogenous depression, often referred to as reactive depression, emerges as a natural response to challenging life events—anything from a painful breakup to the stress of job loss. Unlike endogenous depression, which arises from internal biochemical imbalances, exogenous forms are triggered by identifiable external pressures. Understanding how mood shifts in reaction to life’s storms can help you recognize early warning signs and seek the right support. In this article, we’ll walk through the hallmarks of exogenous depression, explore key risk factors and preventive strategies, outline diagnostic approaches, and share practical treatment pathways so you can feel empowered on your path to recovery.
Table of Contents
- Comprehensive Insight into Exogenous Depression
- Recognizing the Signs of Exogenous Depression
- Understanding Risk Factors and Staying Proactive
- Approaches to Diagnosing Exogenous Depression
- Exploring Effective Management Strategies
- Frequently Asked Questions
A Comprehensive Insight into Exogenous Depression
Exogenous depression is, in many ways, like an emotional umbrella that opens in response to a sudden downpour of life stressors. When you experience a major upheaval—such as the death of a loved one, a financial crisis, or a traumatic incident—your mood can pivot sharply, leading to feelings of sadness, emptiness, or hopelessness that may not have been there before. While these feelings are a normal part of human resilience, they cross into the territory of clinical depression when they persist, impair daily functioning, or significantly affect your quality of life.
At its core, exogenous depression is distinguished by its clear trigger: an external event or series of events. Unlike depressive episodes rooted in genetics or neurochemical imbalances, reactive depression’s hallmark is its context. This doesn’t mean it’s any less real or painful—on the contrary, the intensity of emotions can feel overwhelming, especially when life’s challenges hit unexpectedly. Yet pinpointing the root cause can be an advantage; it offers a tangible starting point for both understanding and intervention.
Key distinguishing factors of exogenous depression include:
- Event-related onset: Symptoms typically follow soon after a triggering event, often within days or weeks.
- Contextual connection: The severity of mood disturbance usually aligns with the magnitude of the stressor.
- Variable duration: Some individuals bounce back within weeks, while others may continue to struggle without guidance.
- Differential recovery: Once the external stressor is managed or resolved, mood may lift more quickly than in endogenous forms.
Imagine your emotional state as a bucket collecting raindrops—each stressful event pours more water into the bucket. If too many drops accumulate without proper drainage (coping strategies), the bucket overflows, leading to a depressive episode. Recognizing the first few droplets—that is, early signs of emotional distress—can allow you to engage your coping drains before the bucket tips over.
Although the diagnosis centers on the link to an external cause, research shows that individual differences—such as coping style, social support, and personal resilience—play a major role in whether someone develops exogenous depression after a stressful event. By combining awareness of external factors with a deeper look at personal resources, you can take proactive steps to mitigate risk and boost recovery.
Recognizing the Signs of Exogenous Depression
Spotting exogenous depression early can feel like recognizing a sudden weather change: the sky darkens, the air feels heavier, and something in your mood shifts. Yet unlike a forecast you can check on your phone, emotional storms may catch you off guard. Being attuned to both subtle and obvious shifts can help you—and those who care about you—take action before symptoms worsen.
Common emotional and cognitive symptoms include:
- Persistent sadness or tearfulness: Feeling down almost every day and crying more easily than usual.
- Irritability or restlessness: Getting frustrated over small things or feeling on edge.
- Difficulty concentrating: Struggling to focus on work, conversations, or previously enjoyable tasks.
- Negative self-talk: Harsh thoughts like “I’m worthless” or “Nothing will ever get better.”
- Loss of interest: No longer finding pleasure in hobbies, socializing, or favorite activities.
Physical and behavioral indicators often manifest as:
- Changes in sleep patterns: Sleeping too much (hypersomnia) or too little (insomnia), waking up earlier, or tossing and turning.
- Appetite and weight fluctuations: Overeating for comfort or losing appetite altogether.
- Low energy and fatigue: Feeling drained, sluggish, or physically heavy, even with minimal exertion.
- Slowed movements or speech: Speaking more slowly or moving as if underwater.
- Withdrawal from loved ones: Cancelling plans, avoiding calls, or isolating in a room.
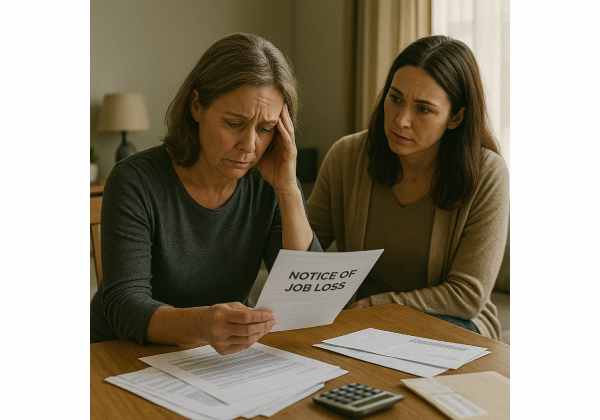
Consider the story of Maya, a 38-year-old teacher who faced an unexpected layoff. Within days, she noticed that her morning jogs felt pointless and her phone buzzes from friends felt annoying rather than welcome. Despite usually handling stress well, she found herself crying on her commute. Because these changes aligned closely with her job loss, Maya’s situation fit the pattern of exogenous depression—her emotional shift was directly tied to an external event.
When to seek help:
- If mood changes last more than two weeks and interfere with everyday life.
- If thoughts of self-harm or suicide emerge.
- If you feel unable to perform at work, school, or in relationships.
- If you rely heavily on alcohol, drugs, or risky behaviors to cope.
By tracking mood patterns—perhaps using a journal or a simple app—you can identify persistent trends rather than momentary dips. Sharing these notes with a trusted friend, family member, or mental health professional can shine a light on whether you’re entering a reactive depressive episode or just experiencing a temporary low.
Understanding Risk Factors and Staying Proactive
Some people weather life’s storms with remarkable resilience, while others find the same events overwhelming. Why does exogenous depression strike some more severely than others? A mix of personal, environmental, and situational risk factors can tip the scales.
Key risk factors include:
- History of depression or anxiety: A prior episode can lower the threshold for future episodes.
- Limited social support: Isolation or strained relationships reduce emotional outlets.
- Ineffective coping skills: Avoidance, suppression, or destructive habits (e.g., substance use).
- High-stress lifestyles: Overwork, caregiving responsibilities, or chronic financial strain.
- Traumatic backgrounds: Past trauma can amplify sensitivity to new stressors.
- Biological vulnerabilities: Genetics, hormonal imbalances, or thyroid issues may weaken emotional resilience.
Imagine your stress tolerance as a cup: if it’s already half-full due to previous challenges, even a small additional stressor can cause it to overflow. That’s why risk factors often compound; each one adds to the emotional load.
Preventive strategies to bolster resilience:
- Cultivate strong connections: Regularly check in with friends, join community groups, or volunteer.
- Learn healthy coping tools: Practice mindfulness, deep breathing, progressive muscle relaxation, or journaling.
- Maintain balanced routines: Prioritize consistent sleep, nutritious meals, and regular physical activity.
- Set realistic boundaries: Learn to say no when demands exceed capacity, whether at work or in relationships.
- Engage in enjoyable activities: Carve out time for hobbies, creative pursuits, or simple pleasures.
- Develop a personal stress plan: Identify early warning signs and map out steps to take—such as calling a friend, scheduling downtime, or seeking professional help.
Real-life example: After her divorce, Lena noticed her old habit of shutting down. Instead of waiting for sadness to intensify, she joined a local art class and reached out weekly to a support group. By proactively adding positive experiences, she widened the gap between stressors and her emotional threshold.
Remember, prevention doesn’t mean you’ll never feel pain—it means equipping yourself to navigate pain more effectively. Whether you keep a gratitude journal, schedule monthly therapy check-ins, or simply practice five minutes of deep breathing daily, each step increases your ability to absorb life’s raindrops without flooding.
Approaches to Diagnosing Exogenous Depression
Pinpointing exogenous depression involves more than ticking symptom boxes—it’s about understanding how your personal story and external circumstances intertwine. A thorough diagnostic process combines self-report measures, clinical interviews, and sometimes physical evaluations to rule out other medical causes.
1. Clinical interview and history taking
The cornerstone of diagnosis is a compassionate conversation with a qualified professional—typically a psychologist, psychiatrist, or licensed counselor. They’ll explore:
- Timeline of symptoms: When did changes start relative to the triggering event?
- Severity and impact: How are mood shifts affecting work, relationships, or self-care?
- Coping responses: What strategies have you tried, and how effective were they?
- Medical and psychiatric history: Any prior mental health diagnoses, medications, or medical conditions.
2. Standardized rating scales
Objective questionnaires help quantify symptom severity:
- PHQ-9 (Patient Health Questionnaire-9): A nine-item survey commonly used in primary care.
- Beck Depression Inventory (BDI): A 21-question instrument assessing emotional, cognitive, and physical symptoms.
- Hamilton Rating Scale for Depression (HAM-D): Clinician-administered scale focusing on observable signs.
3. Physical examination and lab tests
Because medical issues (like thyroid disorders, vitamin deficiencies, or neurological conditions) can mimic depression, your provider may order tests such as:
- Thyroid function panel
- Complete blood count (CBC)
- Vitamin B12 and folate levels
- Blood glucose
These tests help ensure that mood symptoms aren’t secondary to another health issue.
4. Differential diagnosis
Exogenous depression must be distinguished from:
- Endogenous depression: No clear external trigger, often linked to biochemical factors.
- Adjustment disorder: Emotional or behavioral symptoms in response to stressors that are less severe than full-blown depression.
- Bipolar disorder: Alternating manic or hypomanic episodes paired with depressive periods.
- Grief reaction: Bereavement can look similar but tends to fluctuate and include waves of positive memories.
5. Collaborative feedback and treatment planning
Diagnosis isn’t a one-way street. A strong practitioner will share findings, explain why exogenous depression is the best-fit label, and collaborate with you on next steps—from therapy referrals to lifestyle adjustments. This process builds trust and ensures you’re an active participant in your care.
By embracing a multi-pronged diagnostic approach, you gain a clearer picture of both the external forces at play and your internal response patterns. Armed with this clarity, tailored treatment plans can more precisely address the unique contours of your experience.
Exploring Effective Management Strategies
Treating exogenous depression often feels like assembling a toolkit: you pick the right combination of strategies that fit your specific triggers and needs. While no single approach works for everyone, blending professional guidance, self-help techniques, and lifestyle tweaks maximizes your chances of recovery.
1. Psychotherapy (talk therapy)
- Cognitive Behavioral Therapy (CBT): Helps you identify and reframe unhelpful thoughts tied to stressful events.
- Interpersonal Therapy (IPT): Focuses on improving communication and relationships, which can be strained by life changes.
- Acceptance and Commitment Therapy (ACT): Teaches mindful acceptance of emotions without getting pulled into negative thinking.
- Group therapy: Provides peer support, normalization, and shared coping strategies.
2. Medications
While exogenous depression can sometimes resolve as stressors subside, medications may be recommended if symptoms are severe or persistent. Common options include:
- Selective Serotonin Reuptake Inhibitors (SSRIs): e.g., sertraline, escitalopram.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): e.g., venlafaxine, duloxetine.
- Atypical antidepressants: e.g., bupropion or mirtazapine.
A psychiatrist or primary care provider can guide dosage, monitor side effects, and determine how long medication may be needed.
3. Lifestyle modifications
Small, consistent habits often pack a big punch:
- Regular physical activity: Exercise releases endorphins and builds resilience—aim for at least 30 minutes most days.
- Sleep hygiene: Establish a calming bedtime routine, limit screens before sleep, and keep a consistent schedule.
- Nutrition: Balanced meals rich in lean protein, whole grains, fruits, and vegetables support brain health.
- Stress reduction practices: Yoga, meditation, deep breathing exercises, or even mindful walking can lower cortisol.
4. Social support and community resources
- Peer support groups: Online or in-person groups can reduce isolation and offer practical tips.
- Family and friends: Open up about what you’re going through and ask for specific help—whether that’s running an errand or checking in daily.
- Employee assistance programs (EAP): Many workplaces offer confidential counseling and referral services.
5. Self-help and resilience-building
- Journaling: Writing down your thoughts can clarify patterns and lighten mental load.
- Creative outlets: Art, music, gardening, or other hobbies provide positive focus and a sense of accomplishment.
- Mindset shifts: Practice gratitude by noting three small things you appreciate each day, even during tough times.
6. Crisis planning
If intense emotions or suicidal thoughts arise:
- Create a safety plan: List warning signs, coping steps, contacts for immediate support (friends, crisis lines), and emergency resources.
- Hotline numbers: Store local suicide hotlines or the international 988 number.
- Professional contacts: Keep your therapist or psychiatrist’s number handy for urgent check-ins.
Just as a gardener tends to different parts of a plant—soil, water, sunlight—effective treatment addresses multiple dimensions of well-being. By combining therapy, medication when necessary, healthy habits, and strong social ties, you nourish the roots of recovery and open the door to lasting emotional growth.
Frequently Asked Questions
What is exogenous depression?
Exogenous depression is a form of clinical depression triggered by external events or stressors, such as loss, trauma, or major life changes. Symptoms mirror other depressive disorders but are directly linked in timing and intensity to identifiable external causes.
How does exogenous depression differ from endogenous depression?
Endogenous depression originates from internal biochemical and genetic factors, often without a clear external trigger. In contrast, exogenous depression follows a significant life event, and symptoms typically correlate with the severity and timing of that event.
What lifestyle changes can help prevent exogenous depression?
Building resilience involves consistent sleep routines, regular exercise, balanced nutrition, stress-management techniques (like mindfulness), and strong social support networks—each acting as a buffer against life’s stressors.
How is exogenous depression diagnosed?
Diagnosis relies on clinical interviews, standardized rating scales (e.g., PHQ-9), and medical evaluations to rule out other causes. A qualified mental health professional assesses symptom timing, severity, and the presence of an identifiable triggering event.
What treatments are most effective for exogenous depression?
A combined approach often yields the best results: psychotherapy (such as CBT or IPT), medication when needed (like SSRIs), lifestyle adjustments (exercise, sleep hygiene), and ongoing social support or group therapy.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for diagnosis and treatment tailored to your individual needs.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or your favorite social media platform, and follow us for more insights. Your support helps our team continue producing quality content to guide you through life’s challenges.










