Scleral melanocytosis is a benign ocular condition characterized by abnormal proliferation of melanocytes, or pigment-producing cells, within the sclera, the eye’s white outer layer. This results in gray or blue-gray patches on the sclera. The condition is usually congenital, which means it is present from birth, and it is more common in people of Asian and African descent. Although it is usually unilateral (affecting only one eye), it can also occur bilaterally.
The primary clinical manifestation of scleral melanocytosis is visible sclera discoloration. This pigmentation rarely causes symptoms or impairs vision, so it is primarily a cosmetic concern. However, in rare cases, extensive pigmentation may be associated with other ocular or systemic abnormalities, necessitating additional testing.
The exact cause of scleral melanocytosis is unknown, but it is thought to be caused by developmental abnormalities that cause melanocytes to migrate and proliferate in the sclera during embryonic development. This condition is generally considered benign and does not predispose people to cancer. Individuals with extensive ocular melanocytosis, on the other hand, have a slightly higher risk of developing uveal melanoma, a type of eye cancer, especially if it involves the uveal tract.
Scleral melanocytosis is primarily diagnosed clinically, based on the distinct appearance of the scleral pigmentation. Additional diagnostic tools, such as slit-lamp examination, optical coherence tomography (OCT), and ultrasound biomicroscopy (UBM), can be used to determine the extent and depth of pigmentation, as well as rule out any associated ocular pathologies.
Traditional Scleral Melanocytosis Management & Treatment
The primary goal of managing and treating scleral melanocytosis is to monitor and address any associated complications or cosmetic concerns. Because the condition is typically benign and asymptomatic, many patients do not require active treatment. However, a comprehensive approach is required to ensure patient comfort and mitigate potential risks.
- Regular Monitoring: Individuals with scleral melanocytosis should see an ophthalmologist on a regular basis to monitor any pigmentation changes and detect potential complications early. Periodic eye examinations, which include imaging studies such as OCT and UBM, aid in tracking the condition’s progression and detecting any associated abnormalities.
- Cosmetic Concerns: Patients who are concerned about the cosmetic appearance of scleral melanocytosis may consider using colored contact lenses to conceal the discoloration. Cosmetic treatments do not treat the underlying condition, but they can boost a patient’s confidence and quality of life.
- Addressing Associated Ocular Conditions: In rare cases, scleral melanocytosis may be associated with other ocular abnormalities, and appropriate interventions are required. These could include treatments for conditions such as uveal melanoma or glaucoma, which necessitate specialized care and management.
- Patient Education: It is critical to educate patients about the nature of scleral melanocytosis, its relatively benign course, and the importance of regular monitoring. Patients should be aware of the signs and symptoms that require immediate medical attention, such as vision changes, eye pain, or new growths within the eye.
- Genetic Counseling: For people who have a family history of ocular or systemic melanocytosis, genetic counseling can provide important information about inheritance patterns and potential risks. This information can help at-risk family members make informed decisions about family planning and early detection strategies.
- Sun Protection: Patients with scleral melanocytosis should be advised to shield their eyes from direct sunlight, as ultraviolet (UV) radiation can aggravate pigmentation and potentially increase the risk of malignant transformation. Wearing UV-protective sunglasses and wide-brimmed hats can help to reduce UV exposure.
- Addressing Psychological Impact: For some patients, scleral melanocytosis’s visible discoloration can have a psychological impact on their self-esteem and social interactions. Psychological support and counseling can help patients deal with these difficulties and improve their overall well-being.
Cutting-Edge Innovations in Scleral Melanocytosis Treatment
Ophthalmology has made significant advances in the diagnosis and treatment of a variety of ocular conditions, including scleral melanocytosis. Cutting-edge innovations are improving our understanding of the condition and opening up new avenues for treatment and monitoring.
Advanced Diagnostic Imaging
Accurate and timely diagnosis is critical for successful treatment of scleral melanocytosis. Diagnostic imaging advances are improving the ability to visualize and assess the extent of scleral pigmentation and related ocular abnormalities.
- Enhanced Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the sclera and other ocular structures. Advanced OCT technologies, such as swept-source OCT and OCT angiography, provide detailed visualization of scleral melanocytosis, allowing for accurate measurement of pigmentation depth and distribution. These tools are extremely useful for diagnosing and monitoring the condition, guiding treatment decisions, and detecting complications early.
- Ultrasound Biomicroscopy (UBM): UBM is a high-frequency ultrasound technique that produces detailed images of the eye’s anterior segment, which includes the sclera. UBM is especially useful for determining the extent of scleral pigmentation and planning surgical interventions as needed. Advances in UBM technology improve image resolution and diagnostic accuracy, allowing for more effective scleral melanocytosis management.
- Confocal Microscopy: Confocal microscopy allows for detailed, in-vivo imaging of the ocular surface and anterior segment at the cellular level. This technology can be used to study the properties of melanocytes in the sclera, providing insights into the pathophysiology of scleral melanocytosis and aiding in the differentiation of benign pigmentation from malignant changes.
Innovative Treatment Approaches
While scleral melanocytosis is typically benign and does not require active treatment, novel treatment approaches are being investigated to address cosmetic concerns and potential complications.
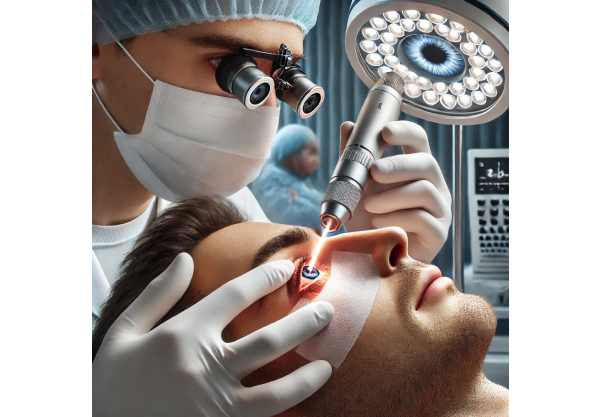
- Laser Therapy: Laser therapy is emerging as a viable treatment option for reducing scleral pigmentation in cases where cosmetic concerns are severe. Q-switched Nd:YAG lasers and picosecond lasers are being studied for their effectiveness in targeting and breaking down melanin deposits in the sclera. Early research indicates that laser therapy can effectively lighten pigmentation with few side effects, providing a non-invasive option for cosmetic management.
- Topical Treatments: Researchers are working to create topical treatments that can reduce scleral pigmentation. These treatments may include depigmenting agents like hydroquinone or retinoids, which are widely used in dermatology to lighten skin pigmentation. While topical treatments for scleral melanocytosis are still in the experimental stage, they show promise as a non-invasive way to address cosmetic concerns.
- Gene Therapy: Because scleral melanocytosis is congenital, gene therapy may be a viable treatment option for the underlying genetic defects. Gene therapy involves delivering functional copies of genes to affected cells in order to correct genetic abnormalities. While this approach is still in the research stage, advances in gene editing technologies, such as CRISPR-Cas9, are opening the door to potential future applications in treating congenital ocular conditions such as scleral melanocytosis.
Personalized Medicine
Personalized medicine involves tailoring treatment strategies to each patient’s unique characteristics, such as genetic makeup, disease profile, and response to therapy. Advances in genomics and molecular diagnostics are allowing for more precise and targeted approaches to treating scleral melanocytosis.
- Genetic Testing: Genetic testing can identify specific mutations linked to congenital ocular melanocytosis, allowing for more targeted treatments. Understanding a patient’s genetic profile enables personalized treatment plans that target the underlying cause of pigmentation and potential complications.
- Biomarker-Guided Therapy: Biomarkers are quantifiable indicators of disease status or treatment outcome. Identifying biomarkers associated with scleral melanocytosis progression and treatment efficacy can aid in tailoring therapies to individual patients, improving outcomes while minimizing side effects.
- Precision Therapeutics: Advances in data analytics and machine learning improve the ability to integrate and interpret large datasets, resulting in more precise and effective treatment strategies. Precision therapeutics is the use of detailed patient data to create personalized treatment plans that address each patient’s specific needs.
Surgical Innovations
In rare cases where scleral melanocytosis is associated with significant ocular abnormalities or complications, surgical intervention may be required. Surgical technique advancements enhance the safety and efficacy of these procedures.
- Minimally Invasive Surgery: Advances in minimally invasive surgical techniques are improving the safety and efficacy of treatments for scleral melanocytosis. These techniques use smaller incisions and less trauma to the eye, which promotes faster recovery and lowers the risk of complications. Minimally invasive scleral patch grafting and reinforcement techniques are being developed and refined to improve patient outcomes.
- Robotic-Assisted Surgery: Robotic systems are being investigated for use in delicate ocular surgeries, such as those to treat scleral melanocytosis complications. Robotic-assisted surgery improves precision and control, allowing surgeons to perform intricate maneuvers with high accuracy. This technology has the potential to increase the success rate of complex surgical procedures for scleral melanocytosis while lowering the risk of complications and improving visual outcomes.






