What is a Lacrimal Fistula?
Lacrimal fistulas are abnormal connections between the lacrimal sac and the skin or another epithelial surface. This condition allows tears to drain directly from the lacrimal sac to the skin, avoiding the normal nasolacrimal duct. This can lead to persistent tearing, recurring infections, and discharge. Lacrimal fistulas can be congenital or acquired, and are frequently the result of infections, trauma, or surgical complications. Understanding the underlying causes and symptoms is critical to effective diagnosis and treatment.
Thorough Analysis of Lacrimal Gland Prolapse
Lacrimal fistula, while relatively uncommon, poses significant clinical challenges due to its impact on ocular health and patient quality of life. The condition is characterized by the formation of an abnormal epithelial-lined tract between the lacrimal sac and the overlying skin, which results in inappropriate tear drainage and potential complications.
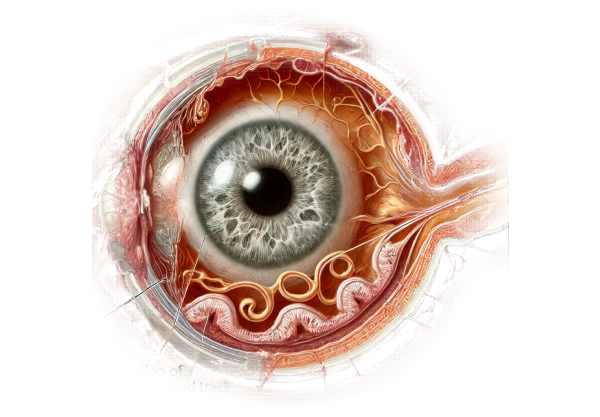
Anatomy and Physiology of the Lacrimal System
The lacrimal system produces, distributes, and drains tears. It consists of the lacrimal glands, which produce tears, as well as the lacrimal drainage apparatus, which includes the puncta, canaliculi, lacrimal sac, and nasolacrimal duct. The lacrimal glands, which are located in the upper outer part of each eye, produce tears. They flow across the eye’s surface, providing both lubrication and protection. Excess tears drain through the puncta on the inner corners of the upper and lower eyelids. Tears leave the puncta and travel through the canaliculi to the lacrimal sac, where they enter the nasolacrimal duct, which empties into the nasal cavity.
Pathophysiology of Lacrimal Fistulas
A lacrimal fistula alters the normal flow of tears by providing an alternate route for tear drainage. This abnormal tract develops due to a variety of etiologies and causes external drainage of tears, frequently resulting in visible and persistent tear overflow on the skin.
Types of Lacrimal Fistulas
- Congenital Lacrimal Fistula: Congenital lacrimal fistulas appear at birth and are typically located near the inner canthus (corner of the eye). These fistulas are caused by developmental anomalies in embryogenesis, which result in the formation of an abnormal epithelial-lined tract between the lacrimal sac and skin. They could be asymptomatic or cause intermittent tearing and discharge.
- Acquired Lacrimal Fistula: Acquired lacrimal fistulas can develop for a variety of reasons, including:
- Infections: Chronic dacryocystitis (infection of the lacrimal sac) can result in the formation of a fistula as the inflamed sac erodes the skin.
- Trauma: Facial injuries or surgeries involving the lacrimal apparatus can cause fistula formation.
- Surgical Complications: Procedures like dacryocystorhinostomy (DCR) can occasionally result in the formation of a fistula, particularly if the surgical site becomes infected or heals improperly.
Symptoms of the Lacrimal Fistula
The symptoms of a lacrimal fistula vary depending on its size, location, and underlying cause. Common symptoms include:
- Epiphora (Excessive Tearing): Consistent tearing that drains externally rather than into the nasal cavity.
- Discharge: Mucous or purulent discharge from the fistula’s opening, particularly if an infection exists.
- Swelling and Redness: Inflammation around the fistula site, usually accompanied by tenderness.
- Recurrent Infections: Frequent cases of dacryocystitis or conjunctivitis caused by an abnormal drainage pathway.
- Visible Fistula Opening: A small skin opening near the inner canthus that allows for the observation of tears and discharge.
Complications of Lacrimal Fistula
If left untreated, lacrimal fistulas can cause a variety of complications, including:
- Chronic Infections: Persistent dacryocystitis and conjunctivitis caused by prolonged exposure of the lacrimal sac to external pathogens.
- Skin Irritation: Continuous tear flow and discharge can result in skin maceration, irritation, and secondary infections near the fistula opening.
- Cosmetic Concerns: The visible tear overflow and fistula opening can be upsetting for patients, causing cosmetic and psychological issues.
Epidemiology
Lacrimal fistulas are uncommon, with congenital forms occurring less frequently than acquired ones. Congenital lacrimal fistulas are typically diagnosed in infancy or early childhood, whereas acquired fistulas can develop at any age, depending on the underlying cause. There is no clear gender preference for lacrimal fistulas.
Risk Factors
Several factors can increase the risk of developing a lacrimal fistula:
- Chronic Dacryocystitis: Recurrent or chronic infections of the lacrimal sac can result in fistula formation.
- Trauma or Surgery: Facial injuries or surgical procedures involving the lacrimal system can lead to the development of fistulas.
- Inflammatory Conditions: Chronic inflammatory conditions of the lacrimal apparatus can predispose people to developing fistulas.
Understanding the detailed anatomy, pathophysiology, and clinical presentation of lacrimal fistulas is critical for a correct diagnosis and treatment. Identifying the underlying cause and treating the symptoms can significantly improve patients’ outcomes and quality of life.
Diagnostic methods
Lacrimal fistulas are diagnosed using a combination of clinical examination, imaging techniques, and, in some cases, laboratory tests. Accurate diagnosis is critical for determining the best treatment plan.
Clinical Examination
- History and Symptom Assessment: The diagnostic process begins with taking a detailed patient history to determine the onset, duration, and nature of symptoms. Questions about recurrent infections, trauma, previous surgeries, and the presence of visible discharge are all important.
- Physical Examination: A thorough physical examination of the eye and surrounding structures is conducted. The examiner looks for signs of epiphora, swelling, redness, and a visible fistula near the inner canthus.
Diagnostic Tests
- Fluorescein Dye Test: Instill fluorescein dye into the conjunctival sac and observe the tear drainage pattern. The presence of dye at the fistula opening suggests an abnormal drainage pathway.
- Probing and Irrigation: Using a thin, flexible probe, you can detect blockages or abnormalities in the lacrimal drainage system. Irrigation with saline can reveal whether the nasolacrimal duct is patent or blocked.
- Dacryocystography (DCG): This imaging technique involves injecting a contrast medium into the lacrimal drainage system and obtaining X-ray images. DCG provides detailed information about the anatomy of the lacrimal apparatus and can determine the location and size of the fistula.
- Dacryoscintigraphy uses a radioactive tracer to assess tear drainage. A gamma camera tracks the tracer’s movements through the lacrimal system, highlighting any blockages or abnormal pathways.
Imaging Studies
- Computer Tomography (CT): CT scans can produce detailed cross-sectional images of the lacrimal system and its surrounding structures. This imaging technique is useful in detecting anatomical abnormalities, infections, and tumors.
- Magnetic Resonance Imaging (MRI): MRI provides high-resolution images of soft tissues and can be used to evaluate the lacrimal system and identify associated conditions.
- Ultrasound: High-frequency ultrasound can detect structural abnormalities or obstructions in the lacrimal sac and duct.
Lab Tests
- Microbiological Cultures: If an infection is suspected, cultures of the fistula discharge can help identify the causative organisms and guide appropriate antibiotic treatment.
Lacrimal Fistula Treatment
Lacrimal fistula treatment aims to correct the abnormal drainage pathway, alleviate symptoms, and prevent complications like recurring infections. The underlying cause, the severity of the symptoms, and the patient’s overall health all influence the treatment decision. Here, we look at different treatment options and highlight innovative and emerging therapies.
Conservative Treatments
- Observation and Hygiene: In some cases, especially with mild congenital fistulas that are asymptomatic or cause minimal discomfort, careful observation and good eye hygiene may suffice. This approach entails cleaning the fistula area on a regular basis to prevent infections and keeping an eye out for any symptoms changes.
- Antibiotic Therapy: For fistulas caused by infections, topical or systemic antibiotics may be prescribed to control bacterial growth and inflammation. This treatment is frequently used in combination with other procedures to control infection and prevent recurrence.
Surgical Treatments
- Fistula Excision: This procedure involves surgically removing the fistula tract and suturing the surrounding tissues to promote healing. It is frequently prescribed for congenital fistulas that cause excessive tearing or infection.
- Dacryocystorhinostomy (DCR): DCR is the most common surgical procedure for lacrimal fistulas caused by chronic dacryocystitis. The surgery opens up a new path for tear drainage from the lacrimal sac to the nasal cavity, avoiding the obstructed nasolacrimal duct. DCR can be done externally with a small skin incision or endoscopically through the nasal passage, with the latter being less invasive and leaving no visible scarring.
- Conjunctivodacryocystorhinostomy (CDCR): When both the upper and lower canaliculi are clogged, CDCR involves creating a new drainage channel from the conjunctiva to the nasal cavity with a glass or silicone tube (Jones tube). This procedure is usually reserved for complex cases in which standard DCR is not feasible.
- Reconstructive Surgery: For fistulas caused by trauma or previous surgeries, reconstructive procedures may be required to repair the lacrimal drainage system and surrounding tissues. These surgeries are custom-made for each patient’s anatomy and the extent of the damage.
Innovative and Emerging Therapies
- Laser-Assisted Surgery: Laser-assisted dacryocystorhinostomy is a minimally invasive procedure that utilizes laser energy to create a new tear drainage pathway. The precision of the laser reduces tissue trauma, promotes faster healing, and lowers the risk of postoperative complications.
- Endoscopic Techniques: Advanced endoscopic procedures enable improved visualization and treatment of the lacrimal drainage system. Microendoscopic tools enable surgeons to perform delicate maneuvers with greater accuracy, resulting in better surgical outcomes.
- Drug-Eluting Stents: Studies on drug-eluting stents that release anti-inflammatory or antimicrobial agents during implantation are ongoing. These stents aim to reduce the risk of infection while also promoting healing, making them a promising option for complex cases.
- Regenerative Medicine: Regenerative medicine research aims to repair or replace damaged lacrimal duct tissues through stem cell or tissue engineering techniques. These approaches may provide long-term solutions to lacrimal fistula and other lacrimal system disorders.
Healthcare providers can provide comprehensive treatment options for patients with lacrimal fistula by combining established surgical techniques and innovative therapies, with the goal of restoring normal tear drainage and improving quality of life.
Effective Methods for Improving and Avoiding Lacrimal Fistula
- Maintain Eye Hygiene: Wash your hands frequently before touching your face or eyes, and clean the area around your eyes with clean, sterile materials.
- Prevent Eye Trauma: Wear appropriate protective eyewear when participating in activities that pose a risk of facial or ocular trauma, such as sports or hazardous work environments.
- Prompt Treatment of Infections: If you notice any symptoms of an eye infection, such as redness, swelling, pain, or discharge, seek medical attention right away to avoid complications that could lead to fistula formation.
- Manage Chronic Conditions: Treat chronic conditions such as sinusitis or allergic rhinitis, which can cause inflammation and increase the risk of lacrimal duct obstruction and fistula.
- Avoid Excessive Eye Rubbing: Avoid vigorously rubbing your eyes, which can cause trauma to the delicate lacrimal structures and increase the risk of a fistula.
- Regular Eye Exams: Schedule regular eye exams to detect early signs of lacrimal system problems and receive prompt treatment.
- Post-Surgical Care: If you have surgery for a lacrimal duct obstruction or fistula, carefully follow the postoperative care instructions to avoid complications and promote proper healing.
- Stay Hydrated: Stay hydrated to promote overall eye health and proper tear production.
- Use Humidifiers: In dry environments, use a humidifier to moisten the air and prevent dryness of the eyes and nasal passages.
- Avoid Smoking: Smoking can worsen inflammation and increase the risk of infection, which can lead to the formation of lacrimal fistulas.
Trusted Resources
Books
- “Diseases of the Lacrimal System” by John D. Dartt
- “Principles and Practice of Lacrimal Surgery” by Mohammad Javed Ali






