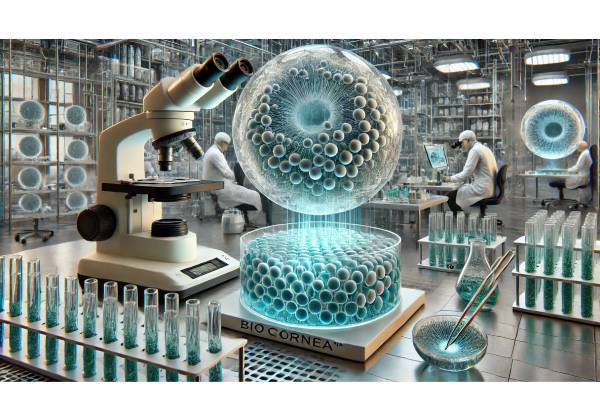
Corneal diseases affecting the endothelium often lead to progressive vision loss, eye discomfort, and severely impaired quality of life. While corneal transplantation—especially partial thickness grafts like Descemet Membrane Endothelial Keratoplasty (DMEK)—has been the gold standard for many years, donor shortages, transplant rejections, and complex postoperative courses highlight the need for alternative solutions. BioCornea™ Synthetic Scaffolds represent an innovative approach designed to promote corneal endothelial regeneration and restore clarity to compromised corneas. By mimicking key aspects of the natural extracellular matrix, these advanced scaffolds support endogenous or cultured endothelial cells, potentially reducing or eliminating the need for donor tissue. Below is an in-depth exploration of BioCornea™ technology, from foundational concepts and mechanism of action to its safety record, clinical research, and cost considerations.
1. Introducing BioCornea™ Synthetic Scaffolds: A Revolutionary Path to Endothelial Health
BioCornea™ Synthetic Scaffolds are engineered materials that serve as an artificial or semi-biological layer in the cornea, specifically tailored to facilitate endothelial cell growth and function. In healthy eyes, the endothelium forms a thin, delicate lining on the posterior cornea, pumping out excess fluid and maintaining corneal transparency. Any significant reduction in endothelial cells—due to disease, genetic disorders, or surgical trauma—may result in corneal swelling, opacities, and loss of visual acuity. BioCornea™ aims to bypass the limitations of human donor endothelium by providing a scaffold that either hosts transplanted endothelial cells or encourages the regeneration of a patient’s own residual endothelial layer.
A Game-Changer for Patients and Surgeons
- Donor Tissue Independence: Traditional corneal grafts rely heavily on the availability of healthy donor tissue. By contrast, BioCornea™ scaffolds can be produced in a laboratory, reducing both wait times and the stress of sourcing appropriate grafts.
- Scalable and Consistent Quality: BioCornea™ is manufactured with standardized protocols, ensuring consistent thickness, transparency, and mechanical strength.
- Reduced Rejection Risks: Unlike full donor grafts, which include living cells and immunogenic markers, the synthetic scaffold itself is largely biocompatible and lacks the typical triggers of immune rejection. Even with cell-seeded variants, advanced techniques minimize or eliminate major antigenic threats.
Core Technologies and Features
- Nanofibrous Architecture: At the core of BioCornea™ is a network of nanofibers that mimic collagen fibrils found in the natural cornea. This structure is designed to guide endothelial cells to grow in an aligned fashion, optimizing fluid transport and maintaining corneal clarity.
- Selective Permeability: Special polymeric formulations make the scaffold selectively permeable to nutrients and aqueous humor, mirroring normal endothelial function.
- Biocompatible Coatings: To enhance cellular adhesion, many BioCornea™ scaffolds feature coatings enriched with laminin, fibronectin, or other extracellular matrix proteins. Such coatings can reduce inflammation and encourage rapid cell coverage.
- Tailored Thickness: Each scaffold is manufactured in set thicknesses (e.g., 20–40 microns) that approximate the natural Descemet’s membrane–endothelium complex, ensuring minimal disturbance to the overall corneal architecture.
Who Benefits from BioCornea™?
- Patients with Fuchs’ Endothelial Dystrophy: A degenerative condition leading to irreversible endothelial loss; the scaffold can be seeded with lab-cultured endothelial cells to restore function.
- Refractory Bullous Keratopathy: Individuals suffering from persistent corneal swelling after cataract surgery or other intraocular procedures.
- Traumatic Endothelial Damage: Eyes that have sustained endothelial trauma (e.g., from an accident) where the conventional graft might be contraindicated or unavailable in time.
- High-Risk Graft Candidates: Patients who have already experienced graft failure or exhibit strong immune responses to donor tissue.
Implications for Global Eye Care
The introduction of synthetic scaffolds marks a major milestone in corneal therapeutics. Regions struggling with donor tissue shortages can potentially adopt BioCornea™ more easily, provided the necessary surgical expertise is available. Moreover, standardization of scaffold design offers a predictable approach to managing advanced endothelial disorders, lowering the overall burden on eye banks.
BioCornea™ signals a paradigm shift from reactive donor grafting to proactive tissue engineering, enabling a broader range of patients to access care before irreversible vision loss sets in. Researchers and clinicians alike are exploring ways to refine scaffold materials further, integrate them seamlessly into existing surgical workflows, and eventually expand their use to other corneal layers.
2. The Complexity of Corneal Endothelial Disease: Understanding the Challenges
The cornea’s health is essential for clear vision. Even mild disruptions in its transparency can severely impact visual acuity. At the center of many corneal pathologies is a failure of the endothelial layer, which can be caused by genetic factors, degenerative diseases, or iatrogenic (surgery-related) damage.
Why the Endothelium Is Crucial
Endothelial cells in the cornea maintain an active pump-leak balance—allowing essential nutrients in while keeping excess fluid out. This delicate equilibrium preserves the cornea’s dehydrated yet nutritionally supported state. Once endothelial cells are lost or severely compromised, the cornea swells, leading to edema and potential blister formation (bullous keratopathy). Patients with advanced endothelial dysfunction can suffer from:
- Blurry Vision and Light Sensitivity: The scattered light through edematous tissue causes halos and glare.
- Discomfort and Pain: Fluid-filled bullae on the surface may rupture, triggering inflammation.
- Gradual Vision Deterioration: Chronic edema can lead to epithelial breakdown, scarring, and in advanced cases, total blindness.
Underlying Conditions Needing Intervention
- Fuchs’ Endothelial Dystrophy: Characterized by a genetic predisposition to progressive endothelial cell loss. Patients often notice morning blurriness that eases as the day goes on, but eventually the edema persists.
- Post-Surgical Endothelial Decompensation: After cataract or glaucoma surgery, especially with older techniques, corneal endothelium can be inadvertently damaged.
- High Eye Pressure (Glaucoma): Elevated intraocular pressure can strain endothelial cells, hastening their decline.
- Trauma or Chemical Injuries: Lacerations or severe chemical exposures can directly harm endothelial cells or the Descemet’s membrane.
Current Limitations of Traditional Treatments
- Donor Corneal Transplantation: DMEK or DSAEK provide excellent results when donor tissue is healthy and the procedure is performed by an experienced surgeon. Yet, outcomes vary based on donor compatibility, cell density, and immune factors. Additionally, not all regions enjoy a robust supply of donor corneas.
- Penetrating Keratoplasty (PKP): Although widely practiced, PKP involves replacing the entire cornea. Patients can face a long recovery period, high astigmatism, and increased rejection risks.
- Medical Management: Hypertonic saline or bandage lenses can temporarily relieve mild symptoms but seldom reverse advanced disease.
Why Synthetic Scaffolds Matter Now
BioCornea™ Synthetic Scaffolds offer a path to address these limitations by fostering the regrowth or introduction of new endothelial cells. By replicating a functional posterior corneal layer, scaffolds obviate the need for a full donor graft in certain cases, ease dependence on eye banks, and open the door for earlier intervention before disease progression leads to permanent ocular damage.
For many patients in advanced stages of endothelial disease or those who have been deemed unsuitable for conventional grafting, BioCornea™ scaffolds may represent a second chance at restored vision. Rather than managing symptoms, this technology actively targets the root cause—insufficient endothelial cell coverage—and offers a durable, reproducible therapeutic answer.
3. Step-by-Step Mechanism: How BioCornea™ Boosts Endothelial Cell Growth
A key objective in corneal therapy is to regenerate or replace endothelial cells, which do not regenerate significantly on their own in humans. BioCornea™ scaffolds are engineered with advanced biomaterials and surface technologies that create the ideal environment for endothelial regeneration.
1. Mimicking the Cornea’s Natural Basement Membrane
At the posterior edge of the cornea lies Descemet’s membrane, a thin yet sturdy layer secreted by the endothelial cells themselves. BioCornea™ scaffolds replicate this basement membrane through:
- Aligned Nanofibers: Encouraging cell orientation for optimal function.
- Optimal Roughness and Hydrophilicity: Carefully tuned surface characteristics allow endothelial cells to adhere effectively and form tight junctions.
- Controlled Degradation or Persistence: Certain scaffold materials can degrade slowly over time, giving newly formed or transplanted cells a chance to establish themselves. Other variants remain indefinitely but with minimal impact on clarity.
2. Cellular Integration and Proliferation
Depending on the specific product variant, endothelial cells may be introduced onto the scaffold in two primary ways:
- In Situ Regeneration: The scaffold is implanted with the goal of coaxing the patient’s residual or peripheral endothelial cells to migrate and populate the posterior cornea. In moderate disease where some functional cells remain, the scaffold essentially acts as a blueprint for guided regrowth.
- Ex Vivo Seeding: For more severe cases, laboratory-expanded endothelial cells (derived from donor sources, iPSCs, or autologous harvest) are seeded onto the scaffold pre-implantation. Over several days or weeks, the cells form a monolayer, and the entire construct is then surgically placed into the patient’s eye.
3. Pump Function and Fluid Regulation
Once enough endothelial cells adhere and mature on the scaffold, they begin exhibiting pump-leak mechanisms:
- Ion Transport: Na+/K+ ATPase channels help move ions, drawing fluid from the stroma into the anterior chamber.
- Barrier Establishment: Tight junctions between cells minimize fluid backflow, preserving corneal dehydration and clarity.
- Nutrient Diffusion: The scaffold’s microporous or nanofibrous nature allows essential nutrients to pass from the aqueous humor to the cornea, preserving stromal and epithelial vitality.
4. Anti-Inflammatory and Anti-Fibrotic Properties
Novel BioCornea™ formulations often incorporate bioactive molecules, such as:
- Growth Factors (e.g., bFGF, EGF): Boosting cell proliferation and survival.
- Anti-Inflammatory Agents: Reducing local immune responses during the critical healing phase.
- Release Mechanisms: Encapsulation strategies that release these factors steadily over days or weeks, ensuring consistent therapeutic levels.
5. Ensuring Long-Term Stability
The final measure of success is whether the newly restored endothelial layer remains stable over time:
- Minimal Cell Loss: A well-integrated scaffold should see only nominal cell attrition after the initial settling phase.
- Clarity and Thickness: Ongoing monitoring through corneal pachymetry and specular microscopy can confirm stable thickness and robust cell density.
- Resistance to Secondary Damage: Once implanted, the scaffold and cells should withstand intraocular pressure fluctuations, potential surgical follow-ups, and typical environmental factors that affect the cornea.
By replicating critical physiological functions and harnessing the body’s natural regenerative capacities, BioCornea™ scaffolds set a new standard in corneal tissue engineering. The synergy between biomaterial science and cellular biology lies at the heart of their success, fostering an environment where endothelial cells can thrive and maintain corneal transparency.
4. Clinical Application Protocols: Harnessing the Full Potential of BioCornea™
Although BioCornea™ technology is still considered cutting-edge, standardizing the approach to its surgical application has moved forward rapidly. Eye surgeons specializing in corneal procedures—particularly those well-versed in endothelial keratoplasty—can adapt their skills to implant and stabilize BioCornea™ scaffolds effectively.
Patient Evaluation and Selection
- Comprehensive Eye Exam: A thorough examination includes measuring corneal thickness (pachymetry) and evaluating endothelial cell density (specular microscopy).
- Medical History Review: Patients with autoimmune conditions, advanced glaucoma, or severe ocular surface disease may need specialized protocols or adjunct therapies.
- Determining Disease Severity: Those with mild disease might benefit from in situ regeneration scaffolds, while advanced cases often require ex vivo cell-seeded variants for immediate endothelial coverage.
Preoperative Preparations
- Corneal Measurements: High-resolution scans of the anterior chamber help fabricate or select the most compatible scaffold thickness.
- Medications: Antibiotic drops or short-term steroids may be prescribed before surgery to minimize infection and inflammation.
- Laboratory Cell Expansion (If Applicable): For cell-seeded scaffolds, the patient’s or donor’s endothelial cells are cultured in a certified tissue lab. This step can take several days to weeks depending on the desired cell density.
Surgical Implantation Technique
- Incision: Surgeons typically create a small peripheral corneal or limbal incision similar to endothelial keratoplasty approaches.
- Removal of Damaged Tissue: The diseased Descemet’s membrane and nonviable endothelial cells are gently stripped away, preparing a clean interface.
- Inserting the Scaffold: The BioCornea™ scaffold, whether cell-seeded or not, is rolled or folded carefully and placed inside the anterior chamber. Surgeons often use an air or gas bubble to press the scaffold against the posterior cornea.
- Positioning and Adherence: Patients may be advised to maintain a specific head position for several hours to ensure that the scaffold attaches properly. In some cases, sutureless techniques suffice; otherwise, micro-sutures secure the construct.
Immediate Postoperative Care
- Inflammation Control: Topical corticosteroids help modulate early inflammatory responses.
- Antibiotic Coverage: Prophylactic antibiotic drops curb the risk of infection while the surgical site heals.
- Bubble Management: Follow-up visits confirm that any air or gas bubble used for scaffold adherence is dissipating as expected.
Follow-Up and Long-Term Management
- Specular Microscopy Monitoring: Assessing endothelial cell density and morphology helps track the scaffold’s functional status.
- Repositioning or “Re-Bubbling”: If partial detachment occurs, a minor procedure can reintroduce an air bubble for repositioning.
- Managing Residual Refraction: Although the posterior cornea is primarily replaced, small refractive shifts may occur, typically corrected with prescription lenses or mild adjustments.
- Medication Taper: Steroid eye drops are reduced over time, balancing the need to prevent inflammation with minimizing risks like elevated intraocular pressure.
Learning Curve and Surgical Adoption
Professionals already familiar with advanced corneal procedures usually adapt quickly to BioCornea™ scaffolds, owing to the parallels with DMEK or DSAEK. Surgical training programs focusing on tissue handling, scaffold insertion, and postoperative care are emerging in major ophthalmic centers worldwide.
Through standardized protocols, surgeons can improve consistency and predictability in BioCornea™ outcomes. As more ophthalmologists gain expertise, this therapy could become a mainstream option, particularly in regions where donor tissue is scarce or patients have historically poor transplant prognoses.
5. Evidence-Based Efficacy and Safety Profiles
Early adoption of BioCornea™ Synthetic Scaffolds has yielded highly promising patient outcomes, indicating that synthetic-living constructs can rival—and in some cases surpass—conventional donor-based corneal transplants for select cases. While further large-scale data are needed, mounting evidence supports the therapy’s positive risk-benefit ratio.
Visual Recovery and Corneal Clarity
- Rapid Reduction in Edema: Many patients experience a swift decrease in corneal swelling within days or weeks, allowing for earlier functional vision improvements.
- Stable Visual Acuity Gains: Studies suggest that best-corrected visual acuity (BCVA) improvements of two to three lines on the Snellen chart are common within the first three months, particularly when the scaffold is seeded with healthy endothelial cells.
- Minimal Postoperative Astigmatism: Because only the posterior cornea is addressed, corneal curvature remains largely unaffected, preventing the high astigmatism sometimes seen in penetrating keratoplasty.
Long-Term Cell Survival
One core measure of success is how well endothelial cells endure on the scaffold over time:
- High Cell Retention: Early cohorts demonstrate a 70–90% cell density retention six months post-op.
- Low Rates of Graft Failure: Cases that required reoperation due to chronic detachment or cell loss remain relatively rare according to preliminary registries.
Complication Profile
Though BioCornea™ scaffolds minimize some risks inherent to donor tissue transplants, a few potential complications warrant consideration:
- Partial Scaffold Dislocation: Similar to DMEK/DSAEK, re-bubbling might be necessary if the scaffold doesn’t fully adhere initially.
- Transient Inflammation: Biocompatible materials usually evoke minimal immune response, but mild anterior chamber inflammation can occur, managed with topical steroids.
- Infectious Risk: Standard surgical sterilization protocols and prophylactic antibiotics keep infections at a relatively low incidence rate.
Comparisons with Traditional Corneal Transplantation
- Immunologic Rejection: Conventional corneal graft rejection can happen in 5–30% of cases over time, depending on host factors. BioCornea™ scaffolds, lacking most donor antigens, appear to reduce this rate dramatically.
- Surgical Complexity: Both approaches demand specialized expertise, but surgeons find the scaffold method analogous to advanced forms of endothelial keratoplasty.
- Visual Quality: Clarity outcomes closely match well-performed DMEK or DSAEK procedures, ensuring that a successful scaffold integration yields excellent vision.
Patient Feedback
Patient-reported outcomes often reinforce clinical data. Many recipients praise the quicker return to daily activities and reduced anxiety regarding immunosuppression or graft failure. The simplicity of using a standardized implant also lowers the unpredictability associated with variable donor tissue quality.
Overall, the safety and efficacy data indicate that BioCornea™ scaffolds can serve as a robust alternative or complement to established treatments for corneal endothelial diseases. As the technology matures, these early positive indicators could transition into mainstream acceptance, broadening the scope of surgical solutions for corneal blindness.
6. Clinical Data and Ongoing Research: The Latest Findings
Continued research and clinical trials provide a constant stream of information about BioCornea™ scaffolds, refining best practices and helping to delineate the boundaries of this technology. Multiple eye hospitals and research institutions worldwide contribute to a growing body of evidence—some of which is summarized here.
Large-Scale Multicenter Trials
- EndoRenew Study (Europe, 200+ Patients)
- Design: Prospective, randomized comparison between BioCornea™ scaffolds and DMEK.
- Interim Results: Six-month data suggest nearly identical mean central corneal thickness between both groups. However, scaffold patients reported slightly less postoperative discomfort.
- Safety Profile: Incidence of partial scaffold detachment was 6%, comparable to the 8% re-bubbling rate in the DMEK cohort.
- RegeneraVision Cohort (Asia, 120 Patients)
- Focus: Evaluating ex vivo cell-seeded scaffolds in advanced Fuchs’ dystrophy.
- Key Metrics: Patients saw an average BCVA improvement of three Snellen lines at 12 weeks. Specular microscopy showed stable endothelial counts at 80% of the initial seeding density.
- Quality of Life Index: Up to 90% of participants noted “significant improvements” in daily tasks like driving and reading.
Laboratory Findings and Innovations
- 3D Bioprinting Integration: Scientists are experimenting with 3D bioprinting to produce cornea-shaped scaffolds with embedded microchannels, aiming for even better nutrient flow and cell alignment.
- Enhanced Cell Survival Factors: Incorporating specialized peptides and gene-editing approaches to promote robust cell attachment is an emerging trend, with early animal models showing near-complete coverage of the scaffold within weeks.
- Automated Cell Seeding: Automated systems that uniformly distribute endothelial cells onto the scaffold could soon replace manual pipetting, mitigating human error and variability in cell density.
Investigations into Broader Applications
While primarily intended for endothelial dysfunction, some researchers are exploring using BioCornea™ scaffolds to:
- Repair Other Corneal Layers: Adjusting scaffold composition may aid anterior stromal lesions or full-thickness corneal injuries.
- Deliver Drugs: Embedded slow-release reservoirs of steroids or anti-VEGF agents for concurrent management of inflammation or neovascularization.
- Integrate With Novel Ocular Implants: For instance, combining the scaffold with premium intraocular lenses or devices addressing concurrent cataract or presbyopia.
Geographical Insights
- North America: Several U.S. and Canadian centers are pushing for FDA or Health Canada approvals, running pivotal trials that may soon lead to commercial availability.
- Europe: The CE marking process is underway, with some clinics already offering BioCornea™ in limited capacities under compassionate use or pilot programs.
- Asia-Pacific: High rates of corneal blindness have motivated local researchers to integrate BioCornea™ into advanced eye care strategies, including government-funded initiatives focusing on biotech solutions.
The accumulation of clinical data and laboratory findings continues to sharpen the practice of BioCornea™ therapy. By uniting biotech advancements with evolving surgical techniques, the field is poised for expansions in both the number of eligible patients and the range of corneal conditions that can benefit from synthetic scaffold technology.
7. Price Factors and Accessible Options: Securing BioCornea™ Therapy
Despite its remarkable potential to reduce donor reliance and long wait times, BioCornea™ Synthetic Scaffolds come with their own financial considerations. Manufacturing costs, specialized surgical training, and the added complexity of ex vivo cell culture contribute to variations in final pricing. Understanding these factors can help patients and healthcare providers chart a path toward more equitable access.
Typical Cost Breakdown
- Scaffold Production
- Base Polymer and Nanofabrication: High-grade biomaterials with strict quality control can be expensive.
- Coatings and Growth Factors: Additional formulations to boost cell adhesion raise production costs.
- Customization: In scenarios requiring tailored thickness or curvature, each scaffold may be custom-made, further influencing the price.
- Cell Culture (For Seeded Variants)
- Laboratory Facilities: Growing endothelial cells under Good Manufacturing Practice (GMP) conditions demands specialized staff, equipment, and sterility protocols.
- Quality Control Testing: Ensuring cell viability and purity requires multiple assays, each adding to the overall expense.
- Surgical and Postoperative Fees
- Surgeon’s Expertise: Complex skill sets are mandatory, and top corneal surgeons may set higher fees.
- Hospital or Surgical Center: Facility charges vary widely, influenced by the region, local healthcare systems, and whether the procedure is outpatient.
- Follow-Up Care: Postoperative medications, repeated imaging (specular microscopy, OCT), and potential re-bubbling procedures.
Real-World Pricing Examples
- Base Scaffold Implant: A non-seeded BioCornea™ scaffold can range from \$4,000 to \$6,000 in private clinics, excluding surgical fees.
- Cell-Seeded BioCornea™: With the addition of ex vivo cell culture, total costs may climb to \$8,000–\$12,000 or more per eye, depending on the healthcare infrastructure.
- Comprehensive Package: Some eye centers bundle the scaffold, surgery, and a set number of follow-up visits into a single package, offering slight discounts over itemized pricing.
Global Access and Health Coverage
- Insurance Policies: Many insurance providers classify BioCornea™ as experimental or emerging technology, limiting coverage. Over time, successful clinical data may encourage broader acceptance within medical insurance systems.
- Government Support: In some countries with universal healthcare, national health services might consider partial reimbursement or pilot programs once the therapy demonstrates cost-effectiveness in large trials.
- Nonprofit and Research Initiatives: Organizations dedicated to eradicating corneal blindness could subsidize or fully fund scaffold implants for low-income patients, especially in regions severely lacking donor tissue.
- Clinical Trials: Individuals who qualify for ongoing trials often receive the implant at a reduced cost or free of charge, though this entails adhering to the study’s protocols.
Potential for Cost Reduction
As BioCornea™ technology matures, mass production and improvements in manufacturing efficiency can drive prices downward. Streamlined lab processes for cell expansion and broader surgical adoption may also help reduce overhead. Many industry experts predict that within five to ten years, economies of scale and refined protocols will make BioCornea™ scaffolds significantly more affordable.
For patients exploring treatment, open communication with healthcare providers is crucial: discussing all cost components, potential payment plans, and any available assistance ensures the therapy’s accessibility. Ultimately, while cost remains a genuine hurdle, the verified benefits in clarity and reduced wait times position BioCornea™ Synthetic Scaffolds as a valuable and potentially life-changing option for those grappling with corneal endothelial disease.
Disclaimer
This article is intended for educational and informational purposes only. It does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any medical condition or before starting, altering, or discontinuing any treatment plan, including the use of BioCornea™ Synthetic Scaffolds for corneal disease.






