Experiencing Diogenes syndrome can feel like being trapped in your own world, where the line between cherished possessions and overwhelming clutter blurs, and basic self-care becomes a distant memory. Often emerging in later life, this complex condition combines profound self-neglect, extreme hoarding, and social withdrawal, leaving individuals and their loved ones overwhelmed and unsure where to turn. In this in-depth guide, we’ll explore Diogenes syndrome’s origins, its hallmark presentations, the factors that increase vulnerability, how professionals arrive at a diagnosis, and the most effective, compassionate treatment approaches. By weaving together real-life examples, practical advice, and scientific insights, we aim to shed light on this challenging disorder and offer clear paths toward hope and recovery.
Table of Contents
- A Comprehensive Examination
- Identifying Core Signs
- Factors Elevating Risk & Preventive Strategies
- Assessing & Pinpointing
- Intervention Strategies
- Common Queries Answered
A Comprehensive Examination
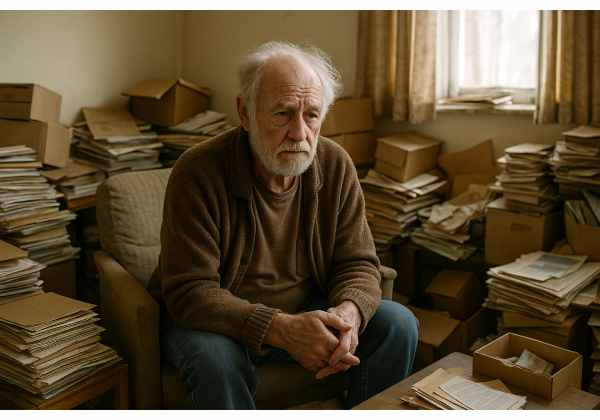
Imagine wearing an invisibility cloak that slowly dulls your connection to the world around you—friends, family, even basic routines fade until only you and your possessions remain. That’s a glimpse into Diogenes syndrome, a disorder marked by pronounced self-neglect, squalor, and hoarding, often accompanied by social isolation and refusal of help. Named after the ancient Greek philosopher Diogenes of Sinope—who famously rejected materialism—this syndrome twists the ideal of living simply into a harmful spiral of abandonment.
Origins and History
First described in psychiatric literature in the 1970s, Diogenes syndrome was recognized among older adults living in extreme domestic squalor. Clinicians noted patterns of:
- Severe Self-Neglect: Personal hygiene, nutrition, and medical care abandoned.
- Domestic Squalor: Homes overflowing with garbage, decaying matter, or hoarded items.
- Social Withdrawal: Avoidance of visitors, cessation of social activities.
Over time, research expanded to include middle-aged individuals and those with cognitive impairments, revealing that Diogenes syndrome is not exclusively an “elderly problem” but often intersects with dementia, depression, and other neuropsychiatric conditions.
Who’s Affected?
- Age: Most common in those over 60, though cases in younger adults occur, especially with underlying psychiatric or neurological issues.
- Gender: Early reports suggested equal prevalence, but some studies note a slight male predominance.
- Living Situation: Frequently identified in individuals living alone without a supportive network.
Why It Matters
Diogenes syndrome carries high health and safety risks:
- Medical Complications: Malnutrition, infections, pressure ulcers, insect infestations.
- Fire and Structural Hazards: Obstructions and accumulated flammable materials increase risk of house fires.
- Social and Economic Burdens: Strained relationships, frequent emergency interventions, and high public service costs.
Understanding the full scope of Diogenes syndrome—from its philosophical namesake to modern clinical definitions—lays the groundwork for spotting its early tremors and intervening before crises escalate. In the next section, we’ll explore the specific signs that often herald this condition’s descent.
Identifying Core Signs
Diogenes syndrome presents with a cluster of interrelated features that span physical, behavioral, and social domains. While individual experiences vary, certain hallmark signs frequently emerge.
1. Profound Self-Neglect
- Personal Hygiene Decline: Infrequent bathing, unkempt hair, and soiled clothing become the norm.
- Neglected Health Needs: Missed medical appointments, unmanaged chronic illnesses, and untreated wounds.
- Poor Nutrition: Skipped meals or reliance on spoiled food, leading to weight loss or vitamin deficiencies.
2. Extreme Hoarding and Squalor
- Accumulation of Items: From newspapers and empty containers to broken appliances—homes become labyrinths of clutter.
- Unsanitary Conditions: Garbage piles, mold growth, and pest infestations often coexist.
- Refusal to Discard: Strong emotional attachment or indifference prevents clearing or organizing possessions.
3. Social Withdrawal and Isolation
- Avoidance of Visitors: Fear of judgment or embarrassment keeps individuals from opening their doors.
- Cessation of Social Roles: No longer participating in hobbies, family events, or community activities.
- Communication Breakdown: Phone calls and letters go unanswered, and friendships wane.
4. Psychological and Cognitive Features
- Lack of Insight: Many lack awareness of the severity of their living conditions or personal neglect.
- Paranoid or Suspicious Thoughts: Some worry that others intend to harm their belongings or evict them.
- Mood Disturbances: Co-occurring depression, anxiety, or apathy can deepen withdrawal and neglect.
5. Complicating Factors
- Cognitive Impairment: Dementia or executive function deficits undermine planning and decision-making.
- Physical Disabilities: Mobility challenges exacerbate difficulties in home maintenance and self-care.
- Financial Strain: Limited resources restrict access to cleaning services, medical care, or social supports.
Real-World Snapshot
Consider Mrs. P, an 82-year-old widow living alone after her husband’s death. Over months, her neighbors noticed uncollected mail and foul odors. When social services finally entered her home, they found knee-deep piles of newspapers, rotting food, and no working utilities. Mrs. P insisted she was “fine” and refused help, illustrating the classic lack of insight that perpetuates Diogenes syndrome.
Recognizing these intertwined symptoms early is critical. If you notice a loved one struggling with hygiene, unmanageable clutter, and social retreat, it may be time to gently explore whether Diogenes syndrome is at play—and seek professional guidance.
Factors Elevating Risk & Preventive Strategies
Understanding why some people develop Diogenes syndrome helps us craft targeted prevention and early intervention measures.
Predisposing Risk Factors
- Advanced Age and Living Alone: Reduced social contacts and mobility challenges heighten vulnerability.
- Personality Traits: Lifetime tendencies toward introversion, emotional detachment, or stubborn independence can escalate into severe neglect under stress.
- Cognitive Decline: Dementia, stroke, or traumatic brain injury impair executive functions—planning, organizing, and self-monitoring.
- Mental Health Conditions: Chronic depression, obsessive-compulsive traits, or psychotic disorders may co-occur and complicate presentations.
Environmental and Social Contributors
- Bereavement and Loss: Death of a spouse or close friend can trigger withdrawal and loss of motivation for self-care.
- Economic Hardship: Inadequate funds for home maintenance, utilities, or healthcare encourage gradual decline.
- Isolation: Lack of neighbors, community engagement, or family support removes vital safety nets.
Preventive Approaches
- Community Outreach and Screening
- Home Visits: Regular check-ins by social workers, nurses, or volunteers for older adults living alone.
- Neighborhood Watch Programs: Encouraging neighbors to share concerns respectfully and refer at-risk individuals for assessment.
- Social Engagement Initiatives
- Senior Centers and Clubs: Offering transportation and activities to maintain connections and monitor well-being.
- Intergenerational Programs: Pairing youth volunteers with older adults to foster mutual support.
- Health and Wellness Monitoring
- Mobile Clinics: Bringing healthcare services directly into communities to catch early signs of neglect or illness.
- Telehealth Options: Virtual check-ins for those with mobility or transportation barriers.
- Educational Campaigns
- Awareness Workshops: Informing community leaders, clergy, and service providers about Diogenes syndrome.
- Resource Guides: Distributing information on local support services, cleaning crews, and mental health helplines.
- Support for Caregivers
- Respite Services: Preventing burnout among family members caring for isolated adults.
- Training Programs: Teaching communication and de-escalation techniques to approach reluctant individuals.
Analogy
Just as preventive maintenance—like regular oil changes and tire rotations—extends a car’s lifespan, early social, medical, and environmental checks can keep individuals from spiraling into the deep neglect of Diogenes syndrome. Building robust community networks and outreach pipelines acts as that maintenance schedule, catching small issues before they become crises.
By addressing both individual vulnerabilities and systemic gaps, we can reduce the incidence and severity of Diogenes syndrome, promoting safer, healthier living environments for at-risk populations.
Assessing & Pinpointing
Diagnosing Diogenes syndrome requires a sensitive, multi-dimensional approach that honors autonomy while ensuring safety.
1. Comprehensive Clinical Interview
- Historical Context: Explore life events—losses, traumas, lifestyle changes—that might precipitate neglect.
- Daily Living Assessment: Discuss routines around hygiene, meals, and home upkeep to gauge functional abilities.
- Insight Evaluation: Gauge awareness of health, hygiene, and environmental conditions.
2. Home Environment Evaluation
- Collaborative Visits: Whenever possible, involve trusted family members or social workers to gain permission and support.
- Safety Inspection: Identify fire hazards, fall risks, pest infestations, and unsanitary conditions.
- Clutter Quantification: Note items blocking exits or utilities, and assess living space usability.
3. Cognitive and Psychiatric Testing
- Cognitive Screens: Mini-Mental State Examination (MMSE) or Montreal Cognitive Assessment (MoCA) to detect dementia or executive dysfunction.
- Psychiatric Scales: Geriatric Depression Scale (GDS) or Anxiety Inventories to uncover mood or anxiety disorders.
4. Medical Workup
- Physical Examination: Evaluate for malnutrition signs, infections, skin breakdown, or dehydration.
- Laboratory Tests: Basic metabolic panel, complete blood count, and infection markers to rule out treatable medical issues.
5. Differential Diagnosis
Ensure symptoms are not solely attributable to:
- Primary Hoarding Disorder: Compulsive acquisition and inability to discard, without self-neglect.
- Severe Depression or Psychosis: Where squalor may be secondary to mood or thought disturbances.
- Substance Use Disorders: Neglect and disorganization driven by addiction.
6. Multidisciplinary Case Conference
- Team Composition: Primary care physician, psychiatrist, social worker, occupational therapist, public health nurse.
- Goal Setting: Develop a shared formulation of factors driving the syndrome and coordinate interventions.
7. Ethical and Legal Considerations
- Capacity Assessment: Determine the individual’s ability to make informed decisions about living conditions and treatment.
- Guardianship or Supported Decision-Making: In cases of impaired capacity, explore legal frameworks to ensure safety while respecting autonomy.
Accurate assessment resembles mapping a complex tapestry: clinical insights, environmental observations, cognitive data, and ethical considerations all weave together to form a comprehensive picture. This foundation guides personalized, practical care plans.
Intervention Strategies
Treating Diogenes syndrome demands patience, creativity, and respect. Abrupt clean-outs or forced hospitalizations often backfire—trust and collaboration are key.
1. Building Rapport and Insight
- Motivational Interviewing: Engage individuals in conversations that elicit their own reasons for change, rather than imposing directives.
- Small, Achievable Goals: Begin with minor tasks—clearing a path to the front door or washing dishes—then build on successes.
2. Environmental Intervention
- Gradual Decluttering:
- Stepwise Approach: Tackle one room or even one drawer at a time to avoid overwhelm.
- Involvement of the Individual: Let them decide what to keep, fostering ownership.
- Professional Cleaning Services:
- Work alongside social services to schedule trusted teams who respect personal belongings.
- Ensure ongoing maintenance plans are in place.
3. Psychosocial Support
- Case Management: Coordinate medical, social, and housing services to provide comprehensive support.
- Therapeutic Groups: Offer peer support for self-neglect and hoarding behaviors, reducing isolation.
- Family Therapy: Educate and involve relatives to sustain gains and monitor relapses.
4. Medical and Psychiatric Treatment
- Medication Management:
- Antidepressants or Antipsychotics: When co-occurring mood disorders or psychosis are present.
- Regular Reviews: Monitor for side effects that could hamper motivation or cognition.
- Health Monitoring: Scheduled nurse visits for wound care, nutrition checks, and vital sign assessments.
5. Skill-Building Interventions
- Occupational Therapy: Teach daily living skills—meal preparation, personal hygiene routines, and home organization techniques.
- Cognitive Remediation: Exercises to improve planning, problem-solving, and memory for those with cognitive deficits.
6. Housing and Safety Planning
- Supported Housing Models: Single-room occupancy with on-site support or shared housing with regular check-ins.
- Emergency Plans: Clear protocols if conditions deteriorate—fire drills, medical alert systems, and response teams.
7. Long-Term Maintenance and Relapse Prevention
- Booster Sessions: Periodic check-ins to reinforce skills and address new stressors.
- Community Integration: Encourage participation in neighborhood activities or volunteer programs to build social capital.
- Early Warning Systems: Identify subtle signs of regression—missed appointments, clutter creeping back—and intervene promptly.
Effective intervention is like gardening: you prepare the soil (building trust), plant seeds (small tasks), nurture growth (ongoing support), and weed regularly (prevent relapse). With holistic, person-centered care, many individuals reclaim safe, dignified living.
Common Queries Answered
What triggers Diogenes syndrome?
Diogenes syndrome often arises from a combination of factors: advanced age, cognitive decline, chronic mental illness (depression, schizophrenia), bereavement, social isolation, and certain personality traits (emotional detachment, stubborn independence).
How is it different from hoarding disorder?
While both involve clutter, Diogenes syndrome features severe self-neglect and squalor. Individuals with hoarding disorder typically care about their possessions and home upkeep, unlike those with Diogenes who abandon basic hygiene and living conditions.
Can Diogenes syndrome be reversed?
Yes, with gradual, respectful intervention. Building trust, engaging in small cleaning tasks, providing psychosocial support, and addressing underlying health conditions can lead to significant improvements in self-care and living environments.
Who should lead the intervention?
A multidisciplinary team—social workers, mental health clinicians, occupational therapists, and trusted family members—should collaborate. Clear leadership by a case manager ensures coordination of medical, environmental, and social supports.
When is hospitalization necessary?
Hospitalization is considered when immediate risks arise—severe malnutrition, infections, fire hazards, or inability to care for oneself. Even then, brief inpatient stays focused on medical stabilization are preferred, followed by community-based support.
Disclaimer: This article is for educational purposes only and does not replace personalized medical advice. If you or someone you know is exhibiting severe self-neglect, squalor, or distressing hoarding behaviors, please seek evaluation from a qualified healthcare professional.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred platform—and follow us for more mental health resources. Your support helps us continue offering compassionate, evidence-based content.