Introduction to Best Disease
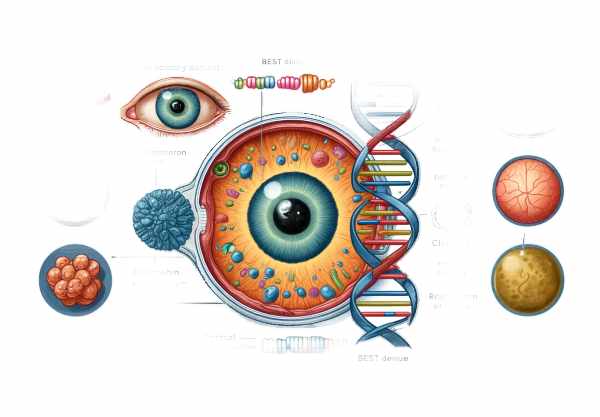
Best disease, also known as vitelliform macular dystrophy, is a genetic eye disorder that primarily affects the macula, the central part of the retina that allows for sharp, central vision. This condition is named after Friedrich Best, a German ophthalmologist who first described it in the early twentieth century. Best disease usually appears in childhood or adolescence and is characterized by the accumulation of lipofuscin, a yellowish pigment in the macula. This accumulation causes a distinct “egg yolk” appearance in the retina. Although the disease progresses slowly, it can eventually result in significant visual impairment. Understanding Best disease is critical for early detection and treatment, preserving vision and quality of life.
Understanding The Condition
Best disease is an autosomal dominant genetic disorder, which means that it can be caused by a single gene mutation inherited from either parent. BEST1, which encodes the protein bestrophin-1, is the most commonly associated gene with Best disease. This protein is essential for the proper function of the retinal pigment epithelium (RPE), a layer of cells that supports the retina’s photoreceptors (rods and cones).
Pathophysiology
The pathophysiology of Best disease includes bestrophin-1 dysfunction, which impairs the RPE’s ability to handle metabolic waste products. As a result, photoreceptor cell turnover produces lipofuscin, which accumulates in the RPE cells. This accumulation causes the macula to develop the characteristic vitelliform lesion. Over time, the accumulation of lipofuscin and other debris can cause RPE cells to degenerate, resulting in photoreceptor damage and eventual vision loss.
Stages of Best Disease
Best disease progresses through several stages, each with unique clinical features:
- Previtelliform Stage: This early stage usually occurs in childhood and can be asymptomatic. There are no visible abnormalities in the retina, but electro-oculography (EOG) can detect subtle changes by measuring the electrical potential of the RPE.
- Vitelliform Stage: At this stage, the “egg yolk” lesion appears in the macula. The lesion is typically round and yellowish, and it is easily visible during a fundoscopic examination. At this point, your vision may be relatively normal.
- ** Pseudohypopyon Stage**: As the disease progresses, the vitelliform lesion may break up and settle, resulting in a layered appearance similar to pseudohypopyon (an accumulation of inflammatory cells in the anterior chamber of the eye). During this stage, your vision may start to deteriorate.
- Vitelliruptive Stage: The lesion continues to break apart, resulting in a “scrambled egg” appearance. Vision usually deteriorates as the structural integrity of the macula is further compromised.
- Atrophic Stage: During the final stage, the RPE and photoreceptors in the macula degenerate, resulting in atrophy. This stage is characterized by significant vision loss and the formation of central scotomas (blind spots).
Symptoms
The symptoms of Best disease differ depending on the stage of the condition, but generally include:
- Blurry or Distorted Vision: Patients’ central vision may become blurred or distorted, making it difficult to read or recognize faces.
- Metamorphopsia is a visual distortion that causes straight lines to appear wavy or curved.
- Reduced Visual Acuity: As the disease progresses, patients may notice a gradual deterioration in their vision.
- Central Scotomas: Blind spots can develop in the central field of vision, affecting daily activities significantly.
Genetic Basis
The vast majority of Best disease cases are caused by mutations in the BEST1 gene. The BEST1 gene, located on chromosome 11q13, encodes the bestrophin-1 protein. Bestrophin-1 plays a role in chloride ion transport and contributes to RPE homeostasis. Mutations in BEST1 impair the function of bestrophin-1, resulting in the pathological changes seen in Best disease.
In addition to BEST1, mutations in other genes, such as PRPH2, have been linked to macular dystrophies. However, BEST1 remains the primary gene linked to classical Best disease.
Inheritance Pattern
Best disease has an autosomal dominant inheritance pattern. This means that an affected individual has a 50% chance of passing on the mutated gene to their offspring. Families affected by Best disease should seek genetic counseling to better understand the risks and implications of the genetic mutation.
Differential Diagnosis
Several other conditions can present with similar clinical features to Best disease, so differential diagnosis is critical. These conditions include the following:
- Adult-Onset Foveomacular Vitelliform Dystrophy: This condition has similar vitelliform lesions but usually develops later in life and has a more benign course.
- Stargardt Disease: This is the most common inherited macular dystrophy, and it is distinguished by the accumulation of lipofuscin in the RPE, similar to Best disease. However, it has an autosomal recessive inheritance pattern and distinct genetic causes.
- Central Serous Chorioretinopathy: This condition causes fluid accumulation beneath the retina, resulting in visual distortion and blurred vision. It is usually self-limiting and does not involve the genetic mutations found in Best disease.
Effects on Quality of Life
Best disease can have a significant impact on quality of life, especially in its later stages. Vision loss can impair daily activities such as reading, driving, and recognizing faces, resulting in decreased independence and socialization. Early diagnosis and appropriate management are critical in assisting patients to adapt to changes in their vision and maintain their quality of life.
Essential Preventive Tips
- Regular Eye Examinations: Schedule regular eye exams with an ophthalmologist to track the progression of Best disease and detect vision changes early.
- Protective Eyewear: Wear sunglasses with UV protection to protect your eyes from harmful ultraviolet rays, which can worsen retinal damage.
- Healthy Diet: Eat a well-balanced diet high in antioxidants, vitamins, and minerals to promote overall eye health. Fish and leafy green vegetables are good sources of omega-3 fatty acids.
- Don’t Smoke: Smoking can hasten the progression of retinal diseases. Avoiding tobacco smoke is critical for maintaining vision.
- Manage Systemic Health: Keep systemic conditions like hypertension and diabetes under control, as they can have a negative impact on retina health.
- Stress Management: Use stress-reduction techniques like yoga, meditation, and deep breathing exercises to manage stress, which can have an impact on overall health.
- Family History Awareness: If your family history includes Best disease, seek genetic counseling. Understanding your genetic risk can help with early detection and management.
- Use of Visual Aids: Use magnifying glasses, large-print books, and other visual aids to help you cope with vision loss and stay independent.
- Stay Informed: Learn more about Best disease and its progression. Staying informed can help you make better choices about your eye health and treatment options.
- Regular Physical Activity: Regular physical activity promotes overall health and well-being, which can have an indirect benefit on eye health.
Diagnostic methods
Best disease (Vitelliform Macular Dystrophy) is diagnosed through a combination of clinical evaluation, imaging techniques, and genetic testing to confirm the presence of characteristic features and underlying genetic mutations.
Clinical Evaluation
An ophthalmologist conducts a comprehensive eye examination to begin the diagnostic process. During this evaluation, the ophthalmologist will obtain a thorough patient history, including any family history of macular dystrophy. Visual acuity tests are used to determine the level of vision impairment.
Fundus Examination
An ophthalmologist can visualize the retina by performing a fundus examination with an ophthalmoscope or a fundus camera. In the vitelliform stage of Best disease, the macula exhibits a distinct yellowish lesion resembling an egg yolk. As the disease progresses, this lesion may break up and become scrambled in appearance.
Optical Coherence Tomography(OCT)
Optical Coherence Tomography (OCT) is a non-invasive imaging technique that produces high-resolution cross-sections of the retina. OCT is extremely useful for detecting the structural changes associated with Best disease, such as lipofuscin accumulation and retinal thinning. It aids in monitoring disease progression and determining the efficacy of treatments.
Fundus Autofluorescence (FAF)
Fundus Autofluorescence (FAF) imaging detects the natural fluorescence produced by lipofuscin in the retinal pigment epithelium. This technique is especially useful for identifying and mapping the distribution of lipofuscin accumulation, which is characteristic of Best disease. FAF can help distinguish Best disease from other retinal conditions with similar clinical characteristics.
Electro-Oculography (EOG)
Electro-oculography (EOG) detects the electrical potential produced by the retinal pigment epithelium in response to light stimulation. The EOG of patients with Best disease typically shows a reduced light rise, indicating retinal pigment epithelium dysfunction. This test is especially useful in the early stages of the disease, when clinical signs may not be obvious.
Genetic Testing
Genetic testing can confirm the diagnosis of Best disease by detecting mutations in the BEST1 gene. A blood sample is collected from the patient, and the DNA is tested for known mutations associated with the condition. Affected families are frequently advised to seek genetic counseling to better understand the disease’s inheritance pattern and implications.
Best Disease Treatment Approaches
While there is no cure for Best disease, there are several treatments available to help manage symptoms and slow the condition’s progression. Treatment strategies are centered on preserving vision and addressing complications as they arise.
Monitoring and Observation
In the early stages of Best disease, when visual acuity is still relatively intact, the primary approach may be regular monitoring and observation. Patients should have regular eye exams to monitor the progression of the disease and detect any changes in the macula.
Low-Vision Aids
Low vision aids, such as magnifying glasses, large-print reading materials, and electronic reading devices, can assist patients with reduced visual acuity in maintaining independence and improving their quality of life. Occupational therapy and vision rehabilitation programs can offer additional assistance and training in the use of these aids.
Anti-VEGF Therapies
Anti-vascular endothelial growth factor (anti-VEGF) therapy is used to treat complications like choroidal neovascularization, which can occur in the late stages of Best disease. Anti-VEGF medications, such as bevacizumab (Avastin) and ranibizumab (Lucentis), are injected into the vitreous humor of the eye to prevent the formation of abnormal blood vessels and reduce fluid leakage.
Photodynamic therapy (PDT)
Another option for treating choroidal neovascularization is photodynamic therapy (PDT). PDT consists of administering a photosensitizing drug followed by laser activation to selectively target and destroy abnormal blood vessels. This therapy can help to stabilize vision and protect the macula from further damage.
Emerging and Innovative Therapeutics
Genetic Therapy
Gene therapy is a new treatment approach that shows promise in correcting the underlying genetic defect in Best disease. Researchers are looking into ways to deliver a functional copy of the BEST1 gene to retinal cells, which could restore normal function and prevent disease progression. While still in the experimental stage, gene therapy provides hope for a future cure.
Stem Cell Therapy
Stem cell therapy is another novel approach being studied for the treatment of retinal degeneration. Researchers hope to restore vision by transplanting healthy retinal cells derived from stem cells into damaged retinas. Early-stage clinical trials are currently underway to determine the safety and efficacy of this approach in Best disease.
Pharmaceutical Interventions
Pharmacological interventions aimed at the underlying mechanisms of Best disease are currently being investigated. Drugs that modulate lipofuscin accumulation or improve retinal pigment epithelial function are being investigated as potential treatments. These treatments are intended to slow the progression of the disease and preserve visual function.
Trusted Resources
Books
- “Inherited Retinal Disease: Diagnosis and Management” by Stephen H. Tsang
- “Retinal Dystrophies: Functional Genomics to Gene Therapy” by Gregory S. Hageman
- “Genetic Diseases of the Eye” by Elias I. Traboulsi
Online Resources
- National Eye Institute: https://www.nei.nih.gov
- American Academy of Ophthalmology: https://www.aao.org
- Foundation Fighting Blindness: https://www.fightingblindness.org
- Orphanet: https://www.orpha.net










