What is Canaliculitis?
Canaliculitis is a rare but serious infection of the canaliculi, which are small channels in the eyelids that drain tears from the eye’s surface to the lacrimal sac. This condition is frequently caused by bacterial, fungal, or viral infections, with the most common culprit being the bacterium Actinomyces israelii. Canaliculitis can produce a number of symptoms, including chronic eye redness, discharge, and localized tenderness. Canaliculitis is frequently misdiagnosed due to its rarity and the subtlety of the initial symptoms, resulting in prolonged discomfort and potential complications. Understanding the underlying causes and manifestations is critical for timely and effective treatment.
Detailed Guide to Canaliculitis
Canaliculitis is a chronic inflammation of the canaliculi, which are tiny ducts in the lacrimal system that drain tears from the eye’s surface into the nose. The condition primarily affects adults and can be difficult to diagnose due to its vague and frequently mild symptoms. An in-depth understanding of canaliculitis entails investigating its anatomy, pathophysiology, causes, symptoms, and effects on patients’ lives.
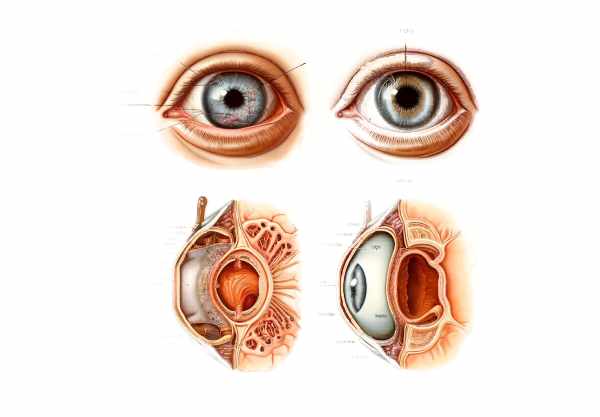
Anatomy and Function of the Canaliculus
The lacrimal system consists of several parts, including the lacrimal glands, puncta, canaliculi, lacrimal sac, and nasolacrimal duct. Canaliculi are small ducts in the upper and lower eyelids that measure approximately 8-10 mm in length. Each eye has two canaliculi, which join to form the common canaliculus and drain into the lacrimal sac. These ducts play an important role in tear drainage, ensuring that tears, debris, and microorganisms are efficiently removed from the eye surface.
Pathophysiology
Canaliculitis’ pathophysiology includes infection and subsequent inflammation of the canaliculi. This condition usually starts when infectious agents like bacteria, fungi, or viruses enter the canaliculi via the puncta. The infection causes the canaliculi to become inflamed and swollen, resulting in obstruction and poor tear drainage. As the infection progresses, dacryoliths (concretions) form within the canaliculi, exacerbating the obstruction and inflammation.
Causes of Canaliculitis
Canaliculitis can be caused by several pathogens, the most common of which are bacteria. Primary causative agents include:
- Bacterial Infections: The most common bacterium found in canaliculitis is Actinomyces israelii, which is a Gram-positive anaerobic bacteria. Other bacteria that can cause the condition include Staphylococcus aureus, Streptococcus species, and Propionibacterium acnes.
- Fungal Infections: Fungal canaliculitis is less common but can occur, especially in immunocompromised people. Candida and Aspergillus are common fungal pathogens.
- Viral Infections: Although viral canaliculitis is uncommon, viruses like herpes simplex virus (HSV) and varicella-zoster virus (VZV) can cause it.
- Parasitic Infections: Although parasitic infections are extremely rare causes of canaliculitis, they do occur in some endemic areas.
Symptoms and Clinical Presentation
Canaliculitis symptoms can vary in severity and often appear gradually, making early diagnosis difficult. Common symptoms include:
- Chronic Redness: Persistent redness in the inner corner of the eye is a common sign of canaliculitis. The redness may be more noticeable in the affected eye.
- Discharge: Patients frequently describe a chronic mucopurulent discharge from the affected eye, which may be worse in the morning. The discharge can be sticky and cause crusting around the eyelids.
- Tearing (Epiphora): Because the canaliculi are obstructed, tears do not drain properly, resulting in excessive tearing and watery eyes.
- Localized Swelling and Tenderness: The inner corner of the eyelid near the punctum may swell and feel tender when touched. This area can also show pouting, in which the punctum appears to be turned outward.
- Concretions (Dacryoliths): In chronic cases, patients may develop dacryoliths within the canaliculi, which can be felt as hard lumps along the canaliculi’s length.
- Punctal Pouting: A clinical examination can reveal that the punctum is swollen and everted (pouting).
Effects on Quality of Life
Canaliculitis can have a significant impact on a patient’s quality of life, especially if the condition is misdiagnosed or undertreated. Chronic symptoms like redness, discharge, and tearing can be uncomfortable and embarrassing, interfering with daily activities and social interactions. Patients may seek medical attention frequently due to persistent symptoms, which can be frustrating and anxiety-inducing. Furthermore, untreated canaliculitis can cause complications such as infection spreading to nearby structures, such as the lacrimal sac and orbit, potentially leading to more serious conditions like dacryocystitis or orbital cellulitis.
Epidemiology
Canaliculitis is a rare condition that affects approximately 2% of patients with lacrimal system disorders. It can affect people of any age, but it is most common in adults, especially those over the age of 50. Canaliculitis affects both men and women equally. The incidence may be higher in populations with a higher prevalence of chronic blepharitis or other ocular surface diseases that predispose people to canaliculitis.
Differential Diagnosis
Canaliculitis symptoms can overlap with those of other ocular conditions, emphasizing the importance of differential diagnosis. Conditions that can mimic canaliculitis are:
- Chronic Conjunctivitis: Chronic inflammation of the conjunctiva can cause similar symptoms such as redness and discharge.
- Dacryocystitis: Inflammation of the lacrimal sac can cause tearing, discharge, and swelling, but it is usually characterized by pain and swelling below the medial canthus, distinguishing it from canaliculitis.
- Blepharitis: Inflammation of the eyelid margins can cause chronic redness and discharge, but it primarily affects the eyelids, not the canaliculi.
- Nasolacrimal Duct Obstruction (NLDO): Although nasolacrimal duct obstruction can cause tearing and discharge, it rarely causes localized swelling and tenderness at the inner corner of the eyelid.
Understanding canaliculitis entails comprehending its anatomy, pathophysiology, causes, symptoms, and impact on patients’ lives. Accurate diagnosis and effective management are critical for alleviating symptoms and preventing complications, thereby improving the overall quality of life for affected people.
Tips to Avoid Canaliculitis
- Maintain Proper Eyelid Hygiene: Cleaning the eyelids and eyelashes on a regular basis can help prevent infections that lead to canaliculitis. To remove debris and bacteria from the eyelids, use gentle cleansers or prescribed scrubs.
- Manage Chronic Blepharitis: If you have chronic blepharitis, consult with your ophthalmologist to help you manage the condition effectively. Treating underlying eyelid inflammation can help lower the risk of canaliculitis.
- Avoid Eye Trauma: Wear safety glasses when participating in activities that may cause eye trauma. Injuries can introduce pathogens into the canaliculi, causing infection.
- Promptly Treat Eye Infections: If you have an eye infection or inflammation, seek immediate treatment. Early intervention can help prevent infection from spreading to the canaliculi.
- Regular Eye Examinations: Regular eye exams can aid in the early detection of canaliculitis and other ocular conditions. Early diagnosis and treatment can help to avoid complications.
- Avoid Contaminated Water: Use caution when swimming in contaminated water or using non-sterile contact lens solutions. Contaminated water can carry pathogens that cause eye infections, such as canaliculitis.
- Proper Contact Lens Care: Follow the contact lens hygiene guidelines, which include regular cleaning and replacement. Poor contact lens hygiene can result in infections that spread to the canaliculi.
- Control Systemic Conditions: Treat systemic conditions such as diabetes and immune deficiencies, which can raise the risk of infection. Keeping these conditions under control can help you avoid ocular infections.
- Educate and Inform: Increase awareness of canaliculitis and its risk factors among family and friends. Educating others can help with early detection and treatment of the condition.
Diagnostic methods
Canaliculitis is diagnosed using a combination of clinical evaluation and specific diagnostic tests in order to accurately identify the infection and its causative agents. The following are the standard and innovative diagnostic techniques used to evaluate canaliculitis:
- Clinical Examination: A detailed patient history and a thorough clinical examination are required. Ophthalmologists look for signs of redness, swelling, and discharge in the inner corner of the eye. Palpation of the canaliculi may reveal tenderness or purulent discharge, which is characteristic of canaliculitis.
- Slit-Lamp Biomicroscopy: This tool enables a detailed examination of the eye at high magnification. Slit-lamp biomicroscopy can detect punctal pouting, canalicular swelling, and the presence of dacryoliths or concretions.
- Canaliculus Probing and Irrigation: Using a fine instrument, probe the canaliculi to determine the canalicular system’s patency. Saline irrigation can help with diagnosis by flushing out debris and pus. If irrigation is obstructed, this indicates canalicular blockage, which is a sign of canaliculitis.
- Microbiological Cultures: A sample of the expressed discharge for microbiological culture and sensitivity testing is required. This aids in identifying the specific pathogen responsible for the infection and guiding appropriate antibiotic therapy. Gram staining is also useful for quickly identifying bacterial infections.
- Imaging Studies: When the diagnosis is uncertain or there are complications, imaging studies like dacryocystography or dacryoscintigraphy may be used. These imaging techniques help to visualize the canalicular and lacrimal sac structures, confirming the presence of obstructions or dacryoliths.
- Advanced Imaging Techniques: Newer imaging modalities, such as optical coherence tomography (OCT) and ultrasound biomicroscopy (UBM), produce high-resolution images of the canaliculi and surrounding tissue. These methods can aid in determining the severity of the infection and any associated structural abnormalities.
- Histopathological Examination: In refractory cases or if malignancy is suspected, a canalicular tissue biopsy may be performed. A histopathological examination can reveal chronic inflammation, granulomas, or neoplastic changes, resulting in a definitive diagnosis.
Combining these diagnostic methods allows for a more thorough assessment of canaliculitis, ensuring accurate identification of the infection and its causative agents, which is critical for effective treatment.
Exploring Canaliculitis Treatments
Canaliculitis treatment aims to eradicate the infection, alleviate symptoms, and restore normal tear drainage. The following are the standard and innovative therapies for canaliculitis:
- Medications: – Antibiotics: Antibiotics are essential for treating bacterial canaliculitis effectively. Topical antibiotics like tobramycin or ciprofloxacin eye drops are widely used. Systemic antibiotics, such as penicillin or amoxicillin, may be required for severe or refractory infections, especially those caused by Actinomyces israelii.
- Antifungals: For fungal infections, antifungal medications such as topical natamycin or oral fluconazole may be prescribed. Treatment times are frequently extended to ensure complete pathogen eradication.
- Antivirals: Antiviral medications like acyclovir or valacyclovir are used to treat viral canaliculitis caused by the herpes simplex or varicella-zoster virus.
- Surgical Interventions: – Canaliculotomy: An incision in the canaliculus removes dacryoliths and drains infection. It is frequently combined with curettage to remove any remaining infected tissue. Canaliculotomy provides immediate relief while also restoring normal tear drainage.
• Dacryocystorhinostomy (DCR): When canaliculitis is associated with nasolacrimal duct obstruction, DCR may be performed. This procedure opens up a new drainage pathway from the lacrimal sac to the nasal cavity, avoiding the obstructed canaliculi and nasolacrimal duct. - Innovative and Emerging Therapies: – Minimally Invasive Techniques: Endoscopic and laser-assisted surgeries provide less invasive treatments for canaliculitis. Endoscopic dacryocystorhinostomy (endo-DCR) involves performing DCR through a nasal endoscope, which reduces surgical trauma and recovery time.
- Drug-Eluting Stents: These stents are placed in the canaliculi to maintain patency while delivering antibiotics or antifungals directly to the infection site. This method ensures consistent drug delivery and can help prevent recurrence.
- Photodynamic Therapy: This novel technique employs light-activated compounds to target and eliminate pathogens within the canaliculi. Photodynamic therapy has shown promise for treating resistant infections and reducing inflammation.
Canaliculitis should be treated promptly and appropriately to avoid complications and restore normal lacrimal function. A combination of medical and surgical therapies, tailored to the pathogen and patient needs, can achieve the best results.
Trusted Resources
Books
- “Diseases of the Lacrimal System” by Adam J. Cohen
- “Oculoplastic Surgery Atlas” by Geoffrey J. Gladstone
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski










