Introduction to Chikungunya Fever
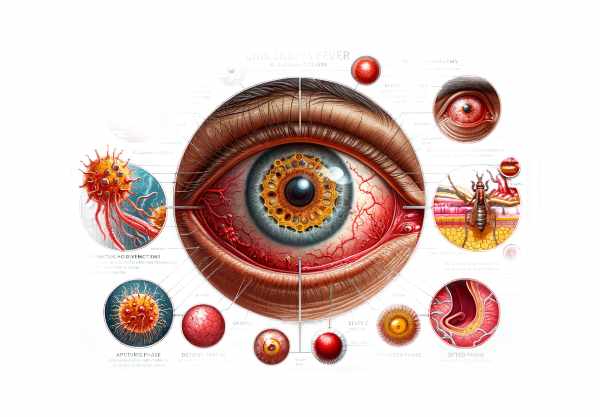
Chikungunya fever is a viral disease transmitted by mosquitos and caused by the Chikungunya virus. It is primarily transmitted by Aedes aegypti and Aedes albopictus mosquitos. While the disease is most commonly associated with severe joint pain, fever, and rash, it can also cause a variety of ocular manifestations. These eye-related symptoms can have a significant impact on one’s quality of life and, in severe cases, cause long-term visual impairment. Understanding the ocular manifestations of Chikungunya fever is critical for timely diagnosis and management, thereby preventing complications and preserving vision in affected individuals.
Understanding The Condition
Chikungunya fever can affect the eyes in a variety of ways, from mild to severe. Ocular manifestations can appear during the acute phase of the infection or weeks to months after the initial illness. These manifestations are diverse and can affect various parts of the eye, including the anterior, posterior, and optic nerves.
Acute anterior uveitis
Acute anterior uveitis is one of the most common ocular manifestations of Chikungunya fever. It causes inflammation in the uveal tract, specifically the iris and ciliary body. Patients frequently report symptoms such as redness, pain, photophobia, and blurred vision. Slit-lamp examination frequently reveals cells and flares in the anterior chamber, indicating inflammation. In severe cases, hypopyon (pus accumulation in the anterior chamber) may be observed.
Retinitis and choroiditis
Chikungunya fever causes significant posterior segment manifestations such as retinitis (retinal inflammation) and choroiditis (choroid inflammation). If not treated promptly, these conditions can lead to vision loss. Symptoms include floaters, blurred vision, and scotomas (blind spots). Retinal hemorrhages, cotton wool spots, and inflammatory infiltrates are typical findings on a fundoscopic examination. Optical coherence tomography (OCT) and fluorescein angiography are effective diagnostic tools for determining the extent of retinal and choroidal involvement.
Optic Neuritis
Optic neuritis, or inflammation of the optic nerve, is a serious complication that can result in sudden vision loss. Patients with optic neuritis frequently report eye pain, decreased visual acuity, and color vision deficits. Fundoscopy may reveal swelling in the optic disc, whereas OCT can help determine the extent of optic nerve damage. Magnetic resonance imaging (MRI) of the brain and orbits is frequently used to confirm a diagnosis and rule out other possibilities.
Conjunctivitis
Conjunctivitis, or inflammation of the conjunctiva, is a common and typically mild ocular manifestation of Chikungunya fever. The symptoms include redness, itching, tearing, and discharge. While conjunctivitis is usually self-limiting, it can be extremely uncomfortable and is frequently accompanied by other systemic symptoms of Chikungunya fever.
Episcleritis and Scleritis
Episcleritis, inflammation of the episclera (a thin layer of tissue that covers the sclera), and scleritis, inflammation of the sclera itself, are less common but significant ocular manifestations of Chikungunya fever. Episcleritis is characterized by mild pain and redness, whereas scleritis is distinguished by severe pain, redness, and potential vision loss. Both conditions must be carefully evaluated to rule out other causes of ocular inflammation.
Keratitis
Keratitis, or corneal inflammation, can develop in patients with Chikungunya fever. This condition is distinguished by pain, redness, photophobia, and blurred vision. Slit-lamp examinations frequently reveal corneal infiltrates, edema, and epithelial defects. Keratitis requires immediate treatment to avoid complications like corneal scarring and vision loss.
Neuroretinitis
Neuroretinitis is an inflammatory condition that affects both the retina and the optic nerve, resulting in visual disturbances. Patients with neuroretinitis may have a sudden loss of vision, usually in one eye. Fundoscopic findings include optic disc swelling and a distinctive “macular star” pattern of exudates. This condition is frequently associated with systemic infections, such as Chikungunya fever, and requires prompt treatment to maintain vision.
Immune-mediated uveitis
Chikungunya fever can sometimes cause immune-mediated uveitis, which is characterized by persistent or recurrent inflammation of the uveal tract. This chronic inflammation can lead to complications like cataracts, glaucoma, and macular edema, all of which can severely impair vision. Immune-mediated uveitis is frequently treated with long-term immunosuppressive therapy.
Maculopathy
Chikungunya fever can cause maculopathy, which is defined as macular edema or inflammation. The macula is responsible for central vision, and any disruption can result in significant visual impairment. Patients may describe blurred vision, distorted vision (metamorphopsia), and central scotomas. OCT is a critical tool for diagnosing macular involvement and assessing treatment outcomes.
Vascular occlusions
Chikungunya fever can also cause vascular occlusions in the retina, including branch retinal vein occlusion (BRVO) and central retinal vein occlusion (CRVO). These conditions occur when blood clots or inflammation block the retinal veins, causing sudden vision loss. Symptoms include a sudden, painless loss of vision, which is often accompanied by retinal hemorrhages and macular edema visible under fundoscopic examination.
Ocular Complications of Systemic Involvement
Chikungunya fever can cause systemic inflammation, which indirectly affects the eyes. For example, severe systemic vasculitis can result in ischemic optic neuropathy, whereas encephalitis can cause neuro-ophthalmic complications such as cranial nerve palsies. These conditions necessitate a multidisciplinary approach to treatment that includes both ophthalmologists and other specialists.
Long-Term Sequels
The long-term ocular consequences of Chikungunya fever can be severe, especially if inflammation is not adequately controlled. Chronic uveitis, glaucoma, cataracts, and macular degeneration are all long-term complications that can cause permanent vision loss. Regular follow-up and early intervention are critical for preventing these outcomes.
Key Tips for Chikungunya Prevention
- Mosquito Control: Use insect repellent, protective clothing, and mosquito nets to reduce the risk of Chikungunya virus transmission.
- Eliminate Breeding Sites: To eliminate mosquito breeding sites, remove standing water around homes and communities where Aedes mosquitos lay their eggs.
- Community Awareness: Educate communities on the symptoms of Chikungunya fever and the importance of seeking medical attention right away to avoid complications.
- Travel Precautions: If visiting areas with known Chikungunya outbreaks, take extra precautions to avoid mosquito bites, such as wearing insect repellent and staying in well-screened or air-conditioned accommodations.
- Personal Protection: Wear long-sleeved shirts, long pants, and socks, especially during peak mosquito activity hours (early morning and late afternoon).
- Regular Health Check-ups: Regular health check-ups for people in endemic areas can aid in the early detection and treatment of Chikungunya fever and its complications.
- Monitor Symptoms: Be alert for new or worsening symptoms, especially ocular symptoms, and seek immediate medical attention if they occur.
- Prompt Treatment: Treating Chikungunya fever as soon as possible can help alleviate symptoms and lower the risk of serious ocular complications.
- Supportive Care: Provide assistance in managing fever and joint pain, which can improve overall health and potentially reduce the severity of ocular symptoms.
- Vaccination Research: Stay up to date on current research and potential developments in vaccines against the Chikungunya virus, which could provide long-term prevention in the future.
Diagnostic methods
The ocular manifestations of Chikungunya fever are diagnosed using clinical evaluation, laboratory tests, and advanced imaging techniques. Accurate diagnosis is critical for effective treatment and avoiding long-term visual impairment.
Clinical Evaluation: The first step in diagnosing ocular complications of Chikungunya fever is a thorough clinical examination. An ophthalmologist will take a thorough patient history to record symptoms like redness, pain, blurred vision, photophobia, and visual disturbances. A thorough eye examination, which includes visual acuity tests, slit-lamp examination, and fundoscopy, is required to detect signs of inflammation, hemorrhages, and other abnormalities.
Laboratory Tests: A variety of tests can be used in the laboratory to confirm Chikungunya virus infection. Polymerase chain reaction (PCR) tests can detect viral RNA in blood samples, especially in the early stages of infection. Serological tests, such as the enzyme-linked immunosorbent assay (ELISA), can detect IgM and IgG antibodies to the Chikungunya virus, indicating a recent or previous infection. These tests help to confirm the diagnosis and rule out other possible causes of ocular symptoms.
Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic nerve. It is extremely useful for diagnosing and monitoring diseases like retinitis, choroiditis, maculopathy, and optic neuritis. OCT can detect subtle changes in retinal thickness, edema, and structural abnormalities, which helps with early diagnosis and treatment planning.
Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and taking a series of photographs of the retina. It aids in the visualization of retinal and choroidal blood flow, as well as the identification of leakage areas and vascular occlusions. Fluorescein angiography is especially useful for diagnosing retinitis, choroiditis, and retinal vascular occlusions caused by Chikungunya fever.
Fundus Photography: Fundus photography provides detailed images of the retina, optic disc, and macula. It is an effective tool for documenting baseline results and tracking disease progression. Fundus photographs can reveal retinal hemorrhages, cotton wool spots, and other signs of inflammation or vascular involvement.
Electroretinography (ERG) measures the retina’s electrical response to light stimulation. It aids in the assessment of retinal function and the detection of abnormalities that would otherwise go undetected during clinical examination or imaging. ERG is useful for determining the degree of retinal involvement in conditions like retinitis and choroiditis.
Magnetic Resonance Imaging (MRI): In cases of suspected optic neuritis or neuroretinitis, an MRI of the brain and orbits can produce detailed images of the optic nerve and surrounding structures. MRI confirms the diagnosis, assesses the extent of inflammation, and rules out other possible causes such as multiple sclerosis or tumors.
Ultrasound Biomicroscopy (UBM): UBM uses high-frequency ultrasound to visualize the eye’s anterior segment, which includes the cornea, iris, and ciliary body. It is especially useful for diagnosing keratitis, uveitis, and other anterior segment conditions caused by Chikungunya fever.
Treatment
Treating ocular manifestations of Chikungunya fever entails addressing the underlying inflammation, managing symptoms, and avoiding complications. A multidisciplinary approach, including ophthalmologists, infectious disease specialists, and other healthcare providers, is frequently required for optimal care.
Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are frequently used to reduce inflammation and relieve symptoms. Topical corticosteroid eye drops are frequently prescribed to treat anterior uveitis, conjunctivitis, and keratitis. Corticosteroids may be administered orally or intravenously in cases of severe or posterior segment inflammation, such as retinitis, choroiditis, and optic neuritis. Corticosteroid dosage and duration should be carefully monitored to avoid potential side effects.
Antiviral Therapy: There is no specific antiviral treatment for Chikungunya fever, but supportive care and symptomatic management are essential. If the ocular manifestations are severe or do not respond to anti-inflammatory therapy, antiviral medications such as ribavirin or interferon may be considered, though their efficacy is unknown. Research into targeted antiviral treatments for the Chikungunya virus is ongoing.
Immunosuppressive Therapy: Patients with immune-mediated uveitis or other chronic inflammatory conditions may benefit from immunosuppressive medications such as methotrexate, azathioprine, or cyclosporine. These medications help to reduce inflammation and prevent recurrence. Regular monitoring and follow-up are critical for managing potential side effects and ensuring effective treatment.
Surgical Interventions: If there are severe ocular complications, surgical interventions may be required. For example, vitrectomy, which removes the vitreous gel from the eye, can be used to treat retinal detachment, vitreous hemorrhage, or persistent inflammation. Laser photocoagulation can be used to treat retinal vascular occlusions and prevent additional vision loss.
Intravitreal Injections: Corticosteroids or anti-VEGF (vascular endothelial growth factor) agents can be injected directly into the eye to treat macular edema, choroiditis, and other posterior segment inflammations. These injections deliver high concentrations of medication directly to the source of inflammation, resulting in quick and effective relief.
Supportive Care: Treating systemic symptoms of Chikungunya fever, such as fever, joint pain, and fatigue, is critical for overall recovery. Adequate hydration, rest, and pain management can help the patient’s overall health and reduce the severity of ocular symptoms.
Emerging Therapies: Investigations into new treatments for Chikungunya fever are ongoing. Monoclonal antibodies, antiviral agents, and immunomodulatory drugs are being studied for their ability to treat both systemic and ocular symptoms of the disease. Advances in gene therapy and biologics may provide new hope for patients with severe or refractory conditions in the future.
Trusted Resources
Books
- “Chikungunya and Other Emerging Viruses” by Stephen Higgs
- “Infectious Diseases of the Eye” by P. K. Mukherjee
- “Ocular Inflammatory Disease and Uveitis Manual” by John J. Huang and James P. Dunn










