Introduction to Choroidal Hemangioma
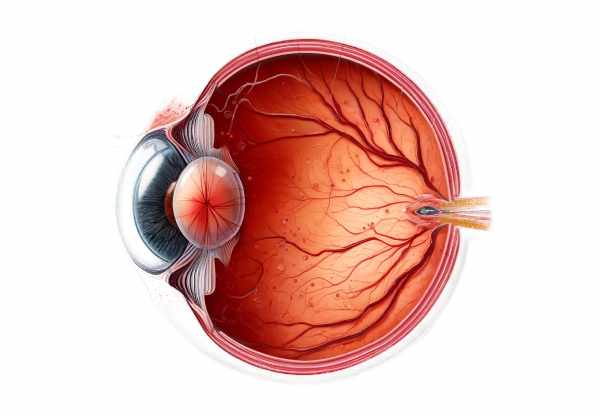
Choroidal hemangioma is a benign vascular tumor that develops in the choroid, which is a layer of blood vessels between the retina and the sclera. This condition can be congenital or acquired, and it frequently appears as an incidental finding during a routine eye examination. While a choroidal hemangioma is usually asymptomatic in its early stages, it can cause significant visual loss if it causes retinal detachment or other complications. These tumors are divided into two categories: circumscribed and diffuse. Circumscribed choroidal hemangiomas are well-defined and typically found in the posterior pole, whereas diffuse choroidal hemangiomas are linked to systemic conditions such as Sturge-Weber syndrome and cover a larger area of the choroid. Understanding the nature, implications, and management of choroidal hemangiomas is critical for avoiding vision loss and receiving timely treatment.
Choroidal Hemangioma Insights
Choroidal hemangiomas are benign tumors that develop from the vascular tissue of the choroid. They are uncommon and can be difficult to diagnose due to their asymptomatic nature in the early stages. These tumors consist of abnormal blood vessels and are classified into two types: circumscribed and diffuse. Each type has distinct clinical characteristics and implications.
Circumscribed choroidal hemangioma.
Circumscribed choroidal hemangiomas are localized vascular tumors that appear as round or oval, orange-red lesions in the eye’s posterior pole. They are frequently discovered during routine eye exams or when patients report symptoms such as blurred vision or visual field defects. The exact cause of circumscribed choroidal hemangiomas is unknown, but they are thought to be congenital or develop spontaneously without any hereditary characteristics.
Clinical Presentation
Patients with circumscribed choroidal hemangiomas may exhibit a variety of symptoms, depending on the size and location of the tumor. Common clinical presentations include the following:
- Visual Disturbances: Common complaints include blurry vision, metamorphopsia (distorted vision), and scotomas (blind spots).
- Retinal Detachment: Large or centrally located hemangiomas can cause serous retinal detachment, in which fluid accumulates beneath the retina, resulting in significant vision loss.
- Photopsia: Patients may experience flashes of light as a result of retinal traction.
- Hyperopia: Farsightedness can result from a tumor causing the retina to shift forward.
Diffuse Choroidal Hemangioma
Diffuse choroidal hemangiomas are vascular lesions that cover a large area of the choroid. They are frequently linked to systemic conditions like Sturge-Weber syndrome, a neurocutaneous disorder marked by facial port-wine stains, leptomeningeal angiomas, and ocular abnormalities.
Clinical Presentation
The clinical presentation of diffuse choroidal hemangiomas includes the following:
- Severe Visual Impairment: Diffuse hemangiomas, because they are widespread, can cause significant and progressive vision loss.
- Retinal Detachment: Like circumscribed hemangiomas, diffuse hemangiomas can cause serous retinal detachment, exacerbating visual symptoms.
- Glaucoma: Angle abnormalities or hemangioma-related secondary effects can cause increased intraocular pressure.
- Strabismus: Misalignment of the eyes can occur, particularly in cases of Sturge-Weber syndrome.
Pathophysiology
The pathophysiology of choroidal hemangiomas involves the growth of abnormal blood vessels within the choroid. These vessels may leak fluid, resulting in retinal detachment and other complications. The precise mechanisms underlying the formation of these tumors are unknown, but genetic and developmental factors are thought to play a role.
Complications
If left untreated, choroidal hemangiomas can cause a number of complications, including:
- Serious Retinal Detachment: An accumulation of subretinal fluid can cause the retina to detach, resulting in severe vision loss.
- Macular Edema: Fluid leakage can cause swelling in the macula, which is the central part of the retina responsible for detailed vision.
- Secondary Glaucoma: Intraocular pressure increases due to angle closure or other mechanisms, which can cause optic nerve damage.
- Choroidal Neovascularization: In some cases, abnormal blood vessel growth can result in additional retinal damage and vision loss.
Differential Diagnosis
Differentiating choroidal hemangiomas from other ocular conditions is critical for proper diagnosis and treatment. Other conditions that may present with similar characteristics include:
- Choroidal Melanoma: A malignant tumor with a hemangioma-like appearance. Melanoma has the potential to be malignant, so differentiation is critical.
- Central Serous Chorioretinopathy (CSCR) is a condition characterized by fluid accumulation beneath the retina, similar to serous retinal detachment caused by hemangiomas.
- Choroidal Metastases: Secondary tumors of systemic malignancies that can cause similar visual symptoms.
- Age-Related Macular Degeneration (AMD), especially the wet form, which causes abnormal blood vessel growth and fluid leakage.
Prevention Tips
Choroidal hemangiomas can be prevented by reducing risk factors and scheduling regular eye exams. Here are some important preventive measures and risk-reduction tips:
- Regular Eye Exams: Routine eye exams can detect early signs of choroidal hemangiomas before symptoms appear, allowing for prompt treatment.
- Management of Systemic Conditions: Proper management of systemic diseases, such as Sturge-Weber syndrome, can lower the risk of ocular complications.
- Protective Eyewear: Wearing protective eyewear during activities that may cause eye trauma can help prevent injuries that aggravate or reveal underlying ocular conditions.
- Genetic Counseling: For people who have a family history of systemic conditions linked to diffuse choroidal hemangiomas, genetic counseling can provide information and preventive measures.
- Awareness of Symptoms: Informing patients about the symptoms of choroidal hemangiomas, such as visual disturbances and flashes of light, can lead to earlier consultations and diagnosis.
- Monitoring High-Risk Individuals: Patients who have known risk factors or underlying conditions should be closely monitored for early ocular changes.
- Healthy Lifestyle: Maintaining a healthy lifestyle, which includes a well-balanced diet high in antioxidants, regular exercise, and quitting smoking, can benefit overall eye health and potentially lower the risk of ocular conditions.
- Early Intervention: Seeking medical attention right away if you notice any visual changes or symptoms can lead to an early diagnosis and better treatment outcomes.
Diagnostic Approaches for Choroidal Hemangioma
Choroidal hemangioma diagnosis requires a combination of clinical examination and advanced imaging techniques to accurately assess the tumor’s presence, size, and impact on ocular structures.
- Ophthalmoscopy: A thorough eye exam with a direct or indirect ophthalmoscope allows the clinician to see the fundus and identify the distinctive orange-red lesion of a choroidal hemangioma. This method offers a preliminary assessment of the tumor’s appearance and location.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and choroid. It aids in detecting subretinal fluid, retinal thickening, and structural changes caused by a hemangioma. OCT is especially useful for monitoring treatment responses.
- Fluorescein Angiography (FA): This procedure involves injecting a fluorescent dye into the bloodstream and taking sequential images of the retinal circulation. This technique identifies areas of leakage, vascular abnormalities, and the tumor’s impact on the retinal vessels. FA is essential for distinguishing hemangiomas from other vascular lesions.
- Ultrasound (B-scan): B-scan ultrasonography is a critical tool for assessing the internal structure of the eye when direct visualization is obstructed by media opacities. It measures the size, shape, and extent of the hemangioma and can detect retinal detachment or other complications.
Innovative Diagnostic Techniques
- Indocyanine Green Angiogram (ICGA): ICGA is similar to fluorescein angiography, but it uses indocyanine green dye to better highlight the choroidal vasculature. This technique provides detailed imaging of the choroidal circulation, allowing the hemangioma to be precisely localized and characterized.
- Enhanced Depth Imaging OCT (EDI-OCT): EDI-OCT enables better visualization of deeper ocular structures, such as the choroid. This advanced type of OCT provides more detail and contrast, which aids in determining the tumor’s depth and involvement with surrounding tissues.
- Fundus Autofluorescence (FAF): FAF imaging detects lipofuscin’s natural fluorescence in the RPE. Changes in autofluorescence patterns can indicate RPE damage or metabolic stress caused by the hemangioma, which aids in disease monitoring.
- Genetic and Molecular Testing: When a hereditary condition is suspected, genetic testing can reveal specific mutations linked to systemic syndromes such as Sturge-Weber syndrome. Molecular diagnostics allow for a better understanding of the genetic basis of diffuse choroidal hemangiomas.
Effective Treatments for Choroidal Hemangioma
The goal of choroidal hemangioma treatment is to alleviate symptoms, avoid complications, and preserve vision. Treatment strategies differ depending on the size, location, and impact of the tumor.
- Observation: Small, asymptomatic choroidal hemangiomas can be monitored without immediate treatment. Regular follow-up examinations are required to detect any changes in size or the onset of complications.
- Photodynamic Therapy (PDT): A photosensitizing agent is administered intravenously, followed by laser activation. This targeted therapy causes selective damage to the tumor’s blood vessels, resulting in reduced fluid leakage and tumor size. PDT is effective in treating circumscribed hemangiomas that cause serous retinal detachment or visual symptoms.
- Laser Photocoagulation: This technique creates burns on the hemangioma with focused laser energy, causing the abnormal blood vessels to coagulate. Laser photocoagulation is usually reserved for small tumors located away from the macula in order to reduce the risk of central vision loss.
- Radiotherapy: External beam radiotherapy or plaque brachytherapy uses localized radiation to shrink tumors and reduce fluid leakage. This method is used for larger or more aggressive hemangiomas and necessitates meticulous planning to minimize damage to surrounding healthy tissues.
Innovative and Emerging Therapies
- Anti-VEGF Therapy: Intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) agents, such as bevacizumab or ranibizumab, are used to reduce vascular permeability and edema caused by choroidal hemangiomas. Anti-VEGF therapy can be especially effective in treating macular edema and improving visual outcomes.
- Gene Therapy: Although still in the experimental stage, gene therapy has the potential to treat choroidal hemangiomas by targeting specific genetic mutations that cause tumor development. Research is being conducted to develop safe and effective gene therapies for ocular vascular tumors.
- Stem Cell Therapy: Stem cell therapy is used to regenerate damaged retinal and choroidal tissues. This emerging field has the potential to restore vision in patients suffering from severe structural damage caused by hemangiomas, though clinical applications are still being investigated.
- Combined Modalities: Using multiple treatment modalities, such as PDT and anti-VEGF injections or laser photocoagulation, can improve therapeutic outcomes. Multimodal approaches are tailored to each patient’s specific condition and response to initial treatments.
Trusted Resources
Books
- “Retina” by Stephen J. Ryan
- “Ocular Oncology” by Arun D. Singh
- “Clinical Ophthalmic Oncology: Retina and Vitreous” by Carol L. Shields and Jerry A. Shields






