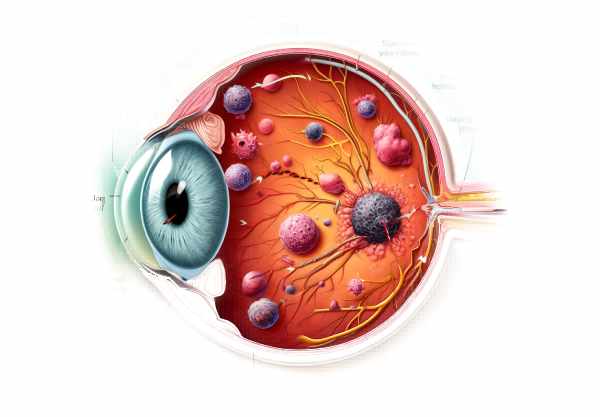
What is Choroidal Metastasis?
Choroidal metastasis is the spread of cancer cells to the choroid, the vascular layer of the eye located between the retina and the sclera. This condition is relatively uncommon, but it is the most common type of intraocular malignancy in adults. The choroid’s abundant vascular supply makes it an ideal target for metastatic cancer cells, which are most commonly derived from breast and lung carcinomas. Patients with choroidal metastasis may experience symptoms such as blurred vision, visual field defects, and eye pain, but some may be asymptomatic at first. Early detection and intervention are critical for managing this condition and maintaining vision.
Choroidal Metastasis Insights
Choroidal metastasis occurs when cancer cells spread from the primary tumor to the choroid. Breast and lung cancers are the most common causes of choroidal metastases, accounting for the vast majority of cases. Other cancers that can spread to the choroid are gastrointestinal tract cancers, prostate cancer, kidney cancer, and cutaneous melanoma. The metastatic process consists of several steps: cancer cells detach from the primary tumor, enter the bloodstream or lymphatic system, survive the circulatory journey, and eventually adhere to and invade choroidal tissue.
Pathophysiology
Choroidal metastasis is characterized by complex interactions between circulating tumor cells and the choroidal microenvironment. The choroid’s extensive vascular network creates an ideal environment for tumor cell lodgement and proliferation. Key stages in the metastatic cascade include:
- Detachment and Dissemination: Tumor cells from the primary site enter blood vessels or lymphatics via processes such as epithelial-mesenchymal transition (EMT), allowing them to become mobile and invasive.
- Survival in Circulation: Tumor cells in the bloodstream must evade immune detection and withstand shear stress. Some cells form emboli by aggregating with platelets, which helps them survive.
- Extravasation and Colonization: When tumor cells enter the choroidal vasculature, they adhere to endothelial cells, migrate through the vessel wall (extravasation), and invade the choroidal stroma. Growth factors and chemokines in the choroidal tissue promote the proliferation and colonization of these cells.
- Angiogenesis and Tumor Growth: Metastatic cells secrete angiogenic factors like VEGF to promote the formation of new blood vessels (angiogenesis). This neovascularization promotes tumor growth and contributes to clinical manifestations.
Clinical Manifestations
The presentation of choroidal metastasis varies according to the size, location, and number of metastatic lesions. Common clinical characteristics include:
- Visual Symptoms: Common initial complaints include blurry vision, scotomas (blind spots), and metamorphopsia (distorted vision). These symptoms are caused by the tumor’s effects on the retinal architecture and subretinal fluid accumulation.
- Visual Field Defects: Depending on the location of the lesion, patients may experience peripheral or central vision loss.
- Photopsia: Patients may report seeing flashes of light caused by retinal traction or detachment.
- Pain and Discomfort: Although many cases are painless, some patients may experience ocular discomfort or pain, particularly if the tumor causes significant inflammation or raises intraocular pressure.
- Redness and Swelling: Tumors extending into the anterior segment can cause visible redness and swelling of the eye.
Complications
If left untreated, choroidal metastasis can cause a number of serious complications:
- Retinal Detachment: Serous retinal detachment occurs when fluid collects beneath the retina, resulting in vision loss.
- Neovascularization: Tumor-induced angiogenesis can lead to abnormal blood vessel growth, increasing the risk of hemorrhage and visual impairment.
- Secondary Glaucoma: Increased intraocular pressure caused by tumor growth or secondary inflammation can progress to glaucoma, resulting in optic nerve damage and irreversible vision loss.
- Ocular Melanocytosis: This rare complication involves the proliferation of melanocytes in the eye, which can worsen pigmentation disorders and increase the risk of melanoma.
Risk Factors
Several factors raise the possibility of developing choroidal metastasis:
- Primary Cancer Type: Patients with breast and lung cancer are at the highest risk because these cancers are more likely to metastasize to the choroid.
- Advanced Cancer Stage: Metastatic disease is more common in patients with advanced or late-stage primary cancers.
- Systemic Metastases: The presence of metastatic spread to other organs raises the risk of ocular involvement.
- Genetic Predisposition: Genetic mutations and a family history of cancer with metastatic potential can increase the risk.
- Immune Status: Immunocompromised patients may be more vulnerable to metastatic spread due to inadequate immune surveillance.
Pathogenesis
Choroidal metastasis is caused by a number of molecular and cellular mechanisms, including:
- Cell Adhesion Molecules: Tumor cells’ integrins and selectins promote adhesion to endothelial cells in the choroidal vasculature.
- Proteolytic Enzymes: Matrix metalloproteinases (MMPs) break down extracellular matrix components, allowing tumor cells to invade and spread throughout tissues.
- Angiogenic Factors: VEGF and other angiogenic cytokines stimulate the formation of new blood vessels, which aids tumor growth and survival.
- Immune Evasion: Tumor cells use strategies to avoid immune detection, such as downregulating major histocompatibility complex (MHC) molecules and producing immunosuppressive cytokines.
Differential Diagnosis
Differentiating choroidal metastasis from other intraocular conditions is critical for proper diagnosis and treatment. Differential diagnosis includes:
- Choroidal Melanoma: A primary malignant tumor of the choroid that can present with similar symptoms but has a distinct growth pattern and clinical course.
- Central Serous Chorioretinopathy (CSCR) is characterized by subretinal fluid accumulation and can resemble metastatic lesions.
- Choroidal Hemangioma: A benign vascular tumor that can be mistaken for metastatic lesions based on fundoscopic appearance.
- Age-Related Macular Degeneration (AMD): Specifically, the wet form, which includes choroidal neovascularization and fluid leakage.
- Inflammatory Conditions: Uveitis and other inflammatory disorders can produce similar ocular findings and must be distinguished using clinical and imaging studies.
Prevention Tips
Preventing choroidal metastasis entails taking proactive measures to manage primary cancers and reduce the risk of metastatic spread. Here are some important preventive measures and risk-reduction tips:
- Early Cancer Detection: Regular screenings and early detection of primary cancers, such as mammograms for breast cancer and low-dose CT scans for lung cancer, can help lower the risk of metastasis.
- Effective Cancer Treatment: Comprehensive and timely treatment for primary cancers, such as surgery, chemotherapy, and radiation, can reduce the risk of metastatic spread.
- Monitoring High-Risk Patients: Patients with a history of cancers that have metastasized to the choroid should undergo regular eye exams to detect early signs of ocular involvement.
- Genetic Counseling: People with a family history of metastatic cancer should seek genetic counseling and testing to identify potential risks and develop effective surveillance strategies.
- Lifestyle Changes: Living a healthy lifestyle, which includes a balanced diet, regular exercise, and abstaining from smoking and excessive alcohol consumption, can improve overall health and potentially lower cancer risk.
- Managing Chronic Conditions: Proper management of chronic diseases such as diabetes and hypertension can boost overall health and resilience to cancer-related complications.
- Immune System Support: Maintaining a healthy immune system through proper nutrition, stress management, and regular medical check-ups can assist the body in fighting cancer spread.
- Awareness and Education: Educating patients on the signs and symptoms of choroidal metastasis, as well as the importance of regular follow-up, can result in earlier detection and better outcomes.
- Research Participation: Patients may wish to participate in clinical trials that investigate new treatments and preventive measures for metastatic cancers, thereby contributing to the advancement of medical knowledge and therapies.
Diagnostic methods
Diagnosing choroidal metastasis requires a combination of clinical examination and advanced imaging techniques to accurately identify and assess metastatic lesions.
Clinical Examination
Ophthalmologists conduct a thorough clinical examination, including a detailed patient history, to detect any primary malignancies. A dilated fundus examination with an ophthalmoscope is required to visualize the choroidal lesions. These lesions usually appear as yellowish-white, elevated masses in the choroid, with or without retinal detachment or subretinal fluid.
Ultrasoundography
Ultrasonography, specifically B-scan ultrasonography, is a non-invasive and widely used method for detecting intraocular tumors. It produces cross-sectional images of the eye, allowing researchers to determine the size, shape, and internal characteristics of choroidal lesions. Choroidal metastasis is typically seen in ultrasonography as a dome-shaped or plateau-like mass with low to medium internal reflectivity.
Optical Coherence Tomography(OCT)
OCT is a high-resolution imaging technique that can produce detailed cross-sectional images of the retina and choroid. It is especially effective at detecting subretinal fluid, retinal detachment, and other retinal changes caused by choroidal metastasis. Enhanced depth imaging (EDI) OCT can provide more detailed visualization of the choroid, assisting in the evaluation of metastatic lesions.
Fluorescein angiogram
Fluorescein angiography is performed by injecting fluorescein dye into the retinal and choroidal vasculature via an IV. This technique aids in determining the vascular properties of the lesions. Choroidal metastases usually have early hypofluorescence and late hyperfluorescence due to leakage from abnormal blood vessels within the tumor.
Indocyanine green angiography (ICG)
ICG angiography employs indocyanine green dye, which is particularly useful for visualizing choroidal circulation. This technique can help distinguish choroidal metastases from other conditions like choroidal melanomas or inflammatory lesions by providing detailed images of the choroidal vasculature.
Magnetic Resonance Imaging (MRI)
MRI can be used to determine the extent of intraocular and orbital involvement by metastatic tumors. It provides excellent soft tissue contrast, which is useful for assessing the disease’s spread beyond the eye.
Positron Emission Tomography(PET)
PET scans can be used alongside computed tomography (CT) to detect metastatic lesions throughout the body, including the eyes. This whole-body imaging technique aids in identifying the primary tumor and other metastatic sites, thereby guiding systemic treatment decisions.
Treatment Options for Choroidal Metastasis
treatment of choroidal metastasis is multifaceted, involving both local ocular therapies to preserve vision and systemic therapies to address the underlying cancer.
Standard Treatment Options:
- Radiation Therapy: External beam radiation therapy (EBRT) is one of the most commonly used treatments for choroidal metastases. It is effective at shrinking tumors and relieving symptoms like visual impairment. Another option for localized radiation treatment is plaque brachytherapy, which involves placing radioactive plaques near the tumor.
- Systemic Chemotherapy: This type of treatment focuses on the primary cancer as well as metastatic lesions throughout the body. The type of primary tumor determines which chemotherapeutic agents are used. For example, patients with breast cancer metastasis may be given anthracyclines or taxanes, whereas those with lung cancer may be given platinum-based regimens.
- Targeted Therapy: Targeted therapies are intended to disrupt specific molecular pathways involved in tumour growth and metastasis. Trastuzumab, for example, may benefit HER2-positive breast cancer patients, whereas erlotinib or osimertinib may benefit patients with EGFR-mutant lung cancer. These treatments can effectively reduce the size of choroidal metastases while improving visual outcomes.
- Hormonal Therapy: Hormonal therapy is used to treat hormone receptor-positive breast cancer. Tamoxifen and aromatase inhibitors can help control metastatic disease and potentially reduce choroidal involvement.
Innovative and Emerging Therapies
- Immunotherapy: Immunotherapies, such as immune checkpoint inhibitors pembrolizumab and nivolumab, have shown promise in treating a variety of cancers, including those with ocular metastasis. These therapies work by increasing the body’s immune response to cancer cells.
- Intravitreal Injections: Anti-VEGF (vascular endothelial growth factor) agents, such as bevacizumab, are being investigated for their ability to reduce subretinal fluid and improve visual acuity in patients with choroidal metastasis. This approach focuses on abnormal blood vessel growth and leakage.
- Photodynamic Therapy (PDT): PDT is the use of photosensitizing agents and light to selectively kill cancer cells. This technique is being studied for its efficacy in treating choroidal metastases, particularly those that do not respond to conventional therapies.
- Gene Therapy: Gene therapy is a newly emerging field that seeks to correct genetic abnormalities that contribute to cancer development. Research is being conducted to develop gene-based treatments for metastatic cancers, including those affecting the eye.
Trusted Resources
Books
- Ocular Tumors in Animals and Humans by Hans E. Grossniklaus, Amy C. K. Kuo, and Karla L. Riddle
- Clinical Ophthalmic Oncology: Uveal Tumors by Arun D. Singh and Bertil E. Damato
- Intraocular Tumors: An Atlas and Textbook by Jerry A. Shields and Carol L. Shields






