What is Choroidal Osteoma?
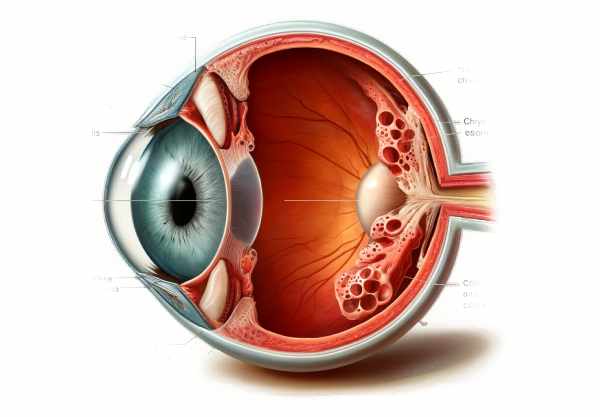
Choroidal osteoma is a rare, benign ossifying tumor of the eye that causes mature bone to form within the choroid, the eye’s vascular layer located between the retina and the sclera. Choroidal osteoma, which was first described in 1978, primarily affects young females and usually appears in their second or third decade of life. This condition can be unilateral or bilateral, and it frequently leads to progressive visual impairment. Understanding the pathophysiology, risk factors, and clinical manifestations of choroidal osteoma is critical for early detection and effective treatment, preserving vision and improving the quality of life for those affected.
Insights into Choroidal Osteoma
roidal osteoma is an uncommon ocular condition characterized by the presence of calcified, mature bone tissue within the choroid. The exact cause of choroidal osteoma is unknown, but it is thought to stem from osseous metaplasia of mesenchymal cells within the choroid. The condition has a strong preference for young females, with about 90% of cases occurring in women. It is most commonly diagnosed in the second or third decade of life, though cases have been reported at various ages.
Pathophysiology
Choroidal osteoma develops when choroidal stromal cells differentiate into osteoblasts, which then produce bone matrix. This bone matrix mineralizes to form mature bone. The causes of this osseous metaplasia are unknown, but hormonal factors may play a role due to its higher prevalence in females.
Features
Choroidal osteomas are usually yellow-white or orange, well-defined, and flat to slightly elevated lesions. Their diameters range from a few millimeters to several centimeters. These lesions are typically found in the juxtapapillary region or the macula, which are critical areas for central vision, explaining the significant visual impairment that is frequently associated with this condition.
Clinical Manifestations
The clinical presentation of choroidal osteoma varies greatly depending on the size and location of the lesion. Common symptoms include:
- Decreased Visual Acuity: Choroidal osteoma is characterized by progressive loss of central vision, particularly in the macula.
- Metamorphopsia: Patients may have distorted vision, with straight lines appearing wavy or bent, especially if the osteoma affects the macular region.
- Scotomas: Blind spots in the visual field may appear, which correspond to areas of choroidal bone formation.
- Photopsia: Flashes of light or shimmering lights may be reported, indicating retinal traction or subretinal fluid.
- Color Vision Changes: The lesion may cause altered color perception, particularly if it affects the macula.
Complications
Choroidal osteoma can cause a variety of complications that worsen visual impairment:
- Choroidal Neovascularization (CNV): Abnormal blood vessels grow from the choroid into the subretinal space, which is a serious complication. CNV can cause hemorrhage, fluid leakage, and additional damage to retinal structures, resulting in rapid vision loss.
- Retinal Detachment: In severe cases, traction from the lesion or associated CNV can cause retinal detachment, which is a sight-threatening condition that requires immediate attention.
- Subretinal Fluid Accumulation: Fluid can accumulate beneath the retina, resulting in serous retinal detachment and additional visual distortion.
- Atrophy: Over time, the retinal pigment epithelium (RPE) and photoreceptors above the osteoma may atrophy, resulting in permanent vision loss.
Epidemiology
Choroidal osteoma is a rare condition that affects approximately one in every one million people. The majority of cases are diagnosed in young adults, with a clear female predominance. There is no known genetic or ethnic predisposition to this condition.
Natural History and Prognosis
The natural history of choroidal osteoma varies. Some lesions remain stable for many years, while others gradually enlarge and calcify. The prognosis is largely determined by the lesion’s location and the presence of complications such as CNV. Because of the macula’s critical role in central vision, lesions affecting it are associated with a poor visual prognosis.
Associated Conditions
While choroidal osteoma is typically a single finding, it can be linked to other ocular or systemic conditions. Patients with choroidal osteoma should have a comprehensive systemic evaluation to rule out any underlying syndromes or diseases.
Pathologic Characteristics
Choroidal osteomas are histologically composed of mature lamellar bone, which frequently contains bone marrow. The overlying RPE may exhibit changes such as hyperplasia, atrophy, or degeneration, which contribute to the visual symptoms and complications associated with the disorder. The presence of CNV, hemorrhage, and subretinal fluid exacerbates the histopathological picture.
Differential Diagnosis
Other intraocular conditions with similar clinical features should be considered when diagnosing choroidal osteoma. These conditions include the following:
- Choroidal Hemangioma: A benign vascular tumor that resembles choroidal osteoma but does not contain calcification.
- Choroidal Melanoma: A malignant tumor that can appear as pigmented lesions but has distinct growth patterns and characteristics on imaging.
- Sclerochoroidal Calcification: This condition causes calcification of the sclera and choroid, but it typically affects older people and has distinct imaging features.
- Osteoma of the Sclera: This condition, which is similar in composition to choroidal osteoma but occurs in the sclera, can be distinguished by its location and imaging findings.
Prevention Tips
- Regular Eye Examinations: Seek comprehensive eye exams from an ophthalmologist, especially if you have risk factors for ocular conditions or notice any vision changes.
- Monitor for Symptoms: Be aware of any new visual disturbances, such as blurriness, metamorphopsia, or photopsia, and notify your eye care provider right away.
- Protect Your Eyes from UV Radiation: Wear sunglasses that completely block UVA and UVB rays to protect your eyes from potential damage.
- Maintain a Healthy Lifestyle: A well-balanced diet high in antioxidants, regular exercise, and quitting smoking can all help improve overall eye health.
- Avoid Prolonged Sun Exposure: To reduce the risk of UV-induced eye damage, limit your exposure to direct sunlight, particularly during peak hours.
- Use Protective Eyewear: Wear appropriate protective eyewear when participating in activities that could result in eye injury, such as sports or certain occupations.
- Know Your Family History: If you have a family history of ocular conditions, speak with your eye doctor to see if more frequent monitoring is required.
- Manage Chronic Conditions: Properly manage systemic conditions such as hypertension, diabetes, and inflammatory diseases to lower the risk of eye complications.
- Stay Informed: Learn the signs and symptoms of choroidal osteoma and other eye conditions so that you can seek medical attention as soon as possible if necessary.
- Follow Up Diligently: Follow your eye doctor’s recommendations for follow-up visits and imaging tests to monitor the osteoma and detect any early signs of complications.
Diagnostic Methods for Choroidal Osteoma
gnosing choroidal osteoma requires a combination of clinical examination and advanced imaging techniques to accurately assess the lesion and track any changes over time.
Clinical Examination
The first step in diagnosing choroidal osteoma is a comprehensive clinical examination by an ophthalmologist. This includes a dilated fundus examination, which allows for direct visualization of the retina and choroid. The osteoma usually appears as a well-defined, yellow-white to orange lesion in the posterior pole of the eye. The lesion can be flat or slightly elevated, and it is often found near the optic disc or macula.
Fundus Photography
Fundus photography is an important tool for capturing the appearance of a choroidal osteoma. High-resolution images of the retina and choroid serve as a baseline for future comparisons, allowing researchers to track any changes in the lesion’s size, shape, or pigmentation over time.
Optical Coherence Tomography(OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique for obtaining cross-sectional images of the retina and choroid. OCT can detect subtle changes in the structure of the retina, such as thinning or disruption of the retinal layers that cover the osteoma. Enhanced depth imaging (EDI-OCT) provides detailed visualization of the choroidal lesion, making it easier to distinguish from other conditions.
B-Scan Ultrasonography
B-scan Ultrasonography is used to assess the thickness and reflectivity of choroidal osteomas. This imaging modality aids in the differentiation of benign osteomas from more suspicious lesions, which may necessitate closer monitoring or intervention. The characteristic high reflectivity of the lesion on B-scan is an important diagnostic feature.
Fundus Autofluorescence (FAF)
Fundus autofluorescence (FAF) imaging detects the natural fluorescence produced by lipofuscin in the retinal pigment epithelium (RPE). FAF can detect areas of RPE atrophy or damage associated with the osteoma, providing additional information about the retinal health above the lesion.
Fluorescein Angiography(FA)
Fluorescein angiography (FA) involves injecting fluorescein dye into the bloodstream to visualize blood flow in the retina and choroidal vessels. This technique can aid in the detection of any leakage or abnormal vascular patterns associated with the osteoma, especially if choroidal neovascularization (CNV) is suspected.
Indocyanine green angiography (ICG)
Indocyanine green angiography (ICG) uses a different dye to better visualize the choroidal vasculature. ICG is especially useful for detecting CNV or other abnormalities that may be associated with osteoma, as it provides detailed images of the deeper choroidal blood vessels.
Innovative Treatments for Choroidal Osteoma
preserve vision, choroidal osteoma is managed by monitoring the lesion for signs of progression or complications, as well as treating associated symptoms.
Observation and Monitoring
Most patients with choroidal osteoma only require regular observation and monitoring. This includes regular eye exams and imaging studies to monitor any changes in the size, shape, or appearance of the osteoma. Patients are typically re-evaluated every 6 to 12 months, depending on the lesion’s characteristics and the presence of any potential complications.
Anti-VEGF Therapies
Anti-vascular endothelial growth factor (anti-VEGF) therapy is the primary treatment for choroidal neovascularization (CNV) caused by choroidal osteoma. Intravitreal injections of anti-VEGF agents such as ranibizumab (Lucentis), aflibercept (Eylea), or bevacizumab (Avastin) can help reduce neovascular growth and fluid leakage while improving or stabilizing vision. Regular injections may be required to keep CNV under control.
Photodynamic therapy (PDT)
Photodynamic therapy (PDT) consists of administering a photosensitizing agent (verteporfin) intravenously before applying a non-thermal laser to the affected area. The activated drug generates reactive oxygen species, which selectively damage abnormal blood vessels and reduce CNV activity. PDT is used less frequently than anti-VEGF therapy, but it remains an option in some cases.
Laser Photocoagulation.
Laser photocoagulation employs thermal laser energy to coagulate and seal abnormal blood vessels. This treatment is better suited for well-defined, extrafoveal CNV lesions that pose a lower risk of damaging central vision. However, it is less commonly used due to the efficacy of anti-VEGF therapy.
Surgery
In rare cases where the choroidal osteoma has caused serious complications such as retinal detachment, surgical intervention may be required. Vitrectomy is a procedure that can be used to repair retinal detachment and remove any subretinal fluid or hemorrhage.
Emerging Therapies
The search for new treatments for choroidal osteoma and its complications is ongoing. Advances in genetic therapy, targeted molecular treatments, and immunotherapy point to more effective and less invasive options in the future. These new treatments aim to selectively target abnormal cells while reducing side effects and preserving vision.
Low-Vision Aids
Patients with significant vision loss caused by choroidal osteoma can benefit from low vision aids such as magnifiers, specialized glasses, and electronic devices. Vision rehabilitation services can offer patients training and resources to help them adjust to their visual limitations.
Trusted Resources
Books
- Intraocular Tumors: An Atlas and Textbook by Jerry A. Shields and Carol L. Shields
- Clinical Ophthalmic Oncology: Uveal Tumors by Arun D. Singh and Bertil E. Damato
- Retina by Stephen J. Ryan, SriniVas R. Sadda, David R. Hinton






