Introduction to Chronic Lacrimal Canaliculitis
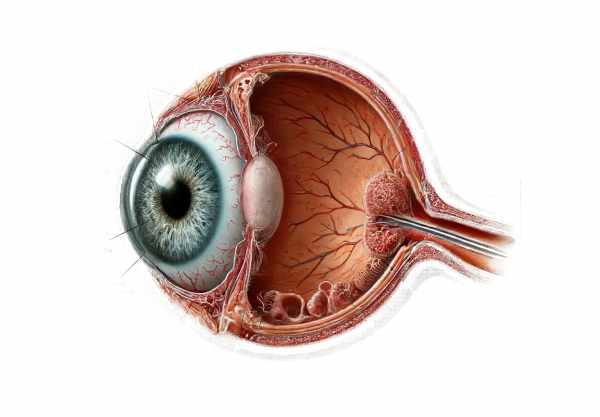
Chronic Lacrimal Canaliculitis is a persistent infection of the lacrimal canaliculi, which are small channels in the eyelids that drain tears from the eye into the lacrimal sac. Bacterial, fungal, or viral pathogens are commonly responsible for this condition, which causes inflammation and canaliculi blockage. Symptoms include redness, swelling, discharge, and, on occasion, a palpable mass in the affected area. Due to its chronic nature, the condition can be difficult to diagnose and treat, necessitating specialized care. Understanding the causes and progression of chronic lacrimal canaliculitis is critical for effective treatment and avoiding complications.
Chronic Lacrimal Canaliculitis: Insights
Chronic Lacrimal Canaliculitis is a complex and multifaceted ocular condition that necessitates a thorough understanding of its causes, pathophysiology, and clinical manifestations. This infection primarily affects the canaliculi, which play an important role in tear drainage. If left untreated, chronic inflammation in this area can lead to a variety of complications.
Etiology and Pathophysiology
Chronic lacrimal canaliculitis is primarily caused by bacteria, fungi, and viruses. Actinomyces israelii is a common bacterial pathogen, as are other anaerobic and aerobic bacteria such as Streptococcus species and Staphylococcus aureus. Fungal infections are uncommon but can be caused by Candida species and Aspergillus. Herpes simplex and Herpes zoster are two rare but notable viral causes.
These pathogens typically colonize the canaliculi, which is where the infection begins. This colonization results in the formation of biofilms, which are complex communities of microorganisms that adhere to canalicular walls and are embedded in their own matrix. Biofilms protect pathogens from the host immune response and antimicrobial treatments, which contributes to the infection’s chronicity.
The presence of these pathogens and biofilms causes an inflammatory response. The inflammation causes swelling of the canaliculi, which leads to obstruction. Chronic inflammation can result in fibrosis and scarring, narrowing the canalicular lumen and exacerbating the obstruction.
Clinical Manifestations
Patients with chronic lacrimal canaliculitis frequently present with a variety of symptoms that can vary in severity. Common symptoms include:
- Persistent Discharge: Chronic mucopurulent discharge from the punctum is a defining feature of chronic lacrimal canaliculitis and can be mistaken for conjunctivitis or other ocular surface infections.
- Redness and Swelling: Canaliculi inflammation results in localized redness and swelling around the affected punctum. The swelling may be accompanied by tenderness.
- Epiphora: Because tears cannot drain properly through the obstructed pathways, canaliculi blockage causes tearing, also known as epiphora.
- Pouting Punctum: The underlying swelling and blockage may cause the affected punctum to appear everted or pouting.
- Canalicular Masses: Chronic inflammation and infection can cause granulomas or dacryoliths (concretions) within the canaliculi, which can be palpable or visible.
Differential Diagnosis
Diagnosing chronic lacrimal canaliculitis from other causes of tearing and discharge is critical. Conditions that can mimic canaliculitis are:
- Acute Dacryocystitis: A lacrimal sac infection that causes similar symptoms but with more widespread redness and swelling around the medial canthal area.
- Conjunctivitis: Inflammation of the conjunctiva that can cause discharge and redness but lacks the localized swelling and tenderness seen in canaliculitis.
- Dry Eye Syndrome is characterized by tear film instability and ocular surface irritation, which leads to reflex tearing but lacks an infectious component.
- Nasolacrimal Duct Obstruction (NLDO): A blockage further downstream in the tear drainage system that causes tearing but not localized canaliculitis.
Pathology and Chronicity
Chronic lacrimal canaliculitis is caused by several key factors that contribute to its persistence and recurrence.
- Biofilm Formation: As previously stated, biofilms play an important role in protecting pathogens from host defenses and treatments. These biofilms can last for a long time, making the infection difficult to eradicate.
- Anatomical Considerations: The canaliculi’s narrow and tortuous anatomy creates an ideal environment for pathogens and biofilms to persist, facilitating chronic infection.
- Incomplete Treatment: Initial treatments, often with topical antibiotics, may fail to penetrate the canaliculi or address the biofilm, resulting in incomplete infection eradication.
- Host Factors: Patients with weakened immune systems, systemic diseases like diabetes, or local conditions like chronic blepharitis are more likely to develop chronic infections.
Complications
Chronic lacrimal canaliculitis can cause a number of complications if not treated:
- Infection Spread: The infection has the potential to spread to adjacent structures, resulting in dacryocystitis, orbital cellulitis, or abscesses.
- Fibrosis and Scarring: Chronic inflammation can cause permanent scarring and narrowing of the canaliculi, resulting in continuous tearing and discomfort.
- Recurrent Infections: Because the condition is chronic, patients may experience recurrent bouts of infection, each of which could cause additional damage to the lacrimal drainage system.
- Surgical Challenges: The presence of fibrosis and scarring can complicate surgical interventions aimed at restoring normal tear drainage, necessitating more involved procedures.
Effects on Quality of Life
Chronic lacrimal canaliculitis has a significant impact on patients’ quality of life. Persistent tearing and discharge can be both socially and physically uncomfortable. The recurring nature of the condition frequently necessitates repeated medical consultations and treatments, putting a financial and emotional strain on patients. Furthermore, the possibility of complications and the need for surgical interventions increases the overall morbidity associated with the condition.
Healthcare providers must understand the complexities of chronic lacrimal canaliculitis, including its etiology and pathophysiology, clinical manifestations, and potential complications. This knowledge allows for timely diagnosis, effective treatment, and the prevention of long-term complications, ultimately improving patient outcomes.
Prevention Tips
Several strategies are used to prevent chronic lacrimal canaliculitis, with the goal of reducing risk factors and promoting early detection. Here are some key preventive measures:
- Maintain good ocular hygiene
To reduce the risk of bacterial colonization, clean the eyelid margins and eyelashes on a regular basis. Use gentle cleansers instead of harsh chemicals. - Quickly Treat Acute Infections:
- Treat acute infections of the eyelids or conjunctiva right away to prevent pathogens from spreading to the lacrimal canaliculi.
- Manage the Underlying Conditions:
- Manage systemic diseases like diabetes, which can predispose people to infections. Regular medical examinations and proper treatment of these conditions are required.
- Avoid Contaminated Eye Makeup.
- Do not share eye makeup, and replace it on a regular basis to avoid bacterial contamination. Use hypoallergenic and preservative-free products whenever possible.
- **Protect Against Trauma:
- Avoid activities that could cause trauma to the eyelids and canaliculi. When engaging in activities that put your eyes at risk, wear protective eyewear.
- Regular Eye Examination:
- Set up regular eye exams, especially if you have a history of ocular infections or other risk factors. Canaliculitis can be treated early to avoid long-term complications.
- Promote Symptom Awareness:
- Be aware of the symptoms of lacrimal canaliculitis, which include persistent discharge, redness, and swelling, and seek medical attention immediately if they occur.
- Stick to Treatment Plans:
- Strictly adhere to the prescribed ocular infection treatments. Completing the entire course of antibiotics or other medications helps to ensure that the infection is completely eliminated.
- Healthy Lifestyle Options:
- Eat a healthy diet, exercise frequently, and avoid smoking. These lifestyle choices promote overall health, including the health of your eyes.
Diagnostic methods
Chronic Lacrimal Canaliculitis is diagnosed using a combination of clinical evaluation, imaging techniques, and lab tests. Accurate diagnosis is critical for successful treatment and management of the condition.
Clinical Evaluation
The first step in diagnosing chronic lacrimal canaliculitis is a comprehensive clinical evaluation by an ophthalmologist. Key elements of the evaluation include:
- Patient History: A thorough history is obtained to identify symptoms such as persistent discharge, redness, swelling, and tearing. Data on previous ocular infections and treatments is also collected.
- Physical Examination A thorough examination of the eyelids and puncta is conducted. Pouting puncta, localized swelling, and discharge are detected. Expressing the puncta may produce mucopurulent material, a telltale sign of canaliculitis.
- Dye Disappearance Test: This test evaluates tear drainage by instilling fluorescein dye in the eye. The dye’s delayed disappearance suggests an obstruction in the lacrimal drainage system.
Imaging Techniques
Imaging is critical for confirming a diagnosis and determining the severity of the disease.
- Dacryocystography: In this imaging technique, a contrast dye is injected into the lacrimal drainage system and then X-rayed. It aids in the detection of blockages and anatomical abnormalities in the canaliculi and lacrimal sac.
- Ultrasound Biomicroscopy (UBM): UBM captures high-resolution images of anterior segment structures, including canaliculi. It is effective at detecting dacryoliths and granulomas.
- Computed Tomography (CT) Scan: A CT scan can be used to determine the severity of the infection and any associated orbital involvement.
Lab Tests
Laboratory tests are required to identify the causative pathogens and guide appropriate treatment.
- Microbial Culture: Discharge samples from the puncta are sent for microbial culture. This aids in the identification of the bacterial, fungal, or viral pathogens causing the infection.
- Histopathological Examination: After surgical intervention, tissue samples may be sent for histopathological examination to confirm the diagnosis and rule out malignancies.
Advanced Diagnostic Tools
Recent advances in diagnostic tools have increased the accuracy and efficiency of diagnosing chronic lacrimal canaliculitis.
- Polymerase Chain Reaction (PCR): PCR is an extremely sensitive technique for detecting bacterial and viral DNA in clinical samples. It is especially useful for detecting difficult-to-culture pathogens.
- Confocal Microscopy: This advanced imaging technique generates high-resolution images of the canaliculi, allowing for a thorough examination of the infection and biofilm presence.
Combining these diagnostic methods allows healthcare providers to accurately diagnose chronic lacrimal canaliculitis and devise an effective treatment plan.
Treatment
To prevent recurrence, Chronic Lacrimal Canaliculitis must be treated using a multifaceted approach that includes medical management, surgical interventions, and addressing underlying causes.
Medical Treatment
Topical and systemic antibiotics are frequently used as the first line of treatment to eradicate the infection.
- Topical Antibiotics: Broad-spectrum antibiotics, such as ciprofloxacin or ofloxacin, are frequently used to combat bacterial pathogens. These are applied directly to the affected area to reduce bacterial growth.
- Systemic Antibiotics: For more serious cases, oral or intravenous antibiotics may be required. Penicillin-based antibiotics are effective against the common causative agent, Actinomyces israelii.
Surgical Treatment
Surgery may be required in cases where medical treatment fails or there are anatomical obstructions that must be addressed.
- Canaliculotomy: This procedure entails making an incision in the canaliculus to remove infected material and dacryoliths. To ensure thorough cleaning, the canaliculus is irrigated with an antibiotic solution.
- Dacryocystorhinostomy (DCR): When the infection has spread to the lacrimal sac, DCR is used to open a new drainage pathway between the sac and the nasal cavity. This procedure assists in bypassing the obstructed canaliculi.
Innovative and Emerging Therapies
Recent advances in the treatment of chronic lacrimal canaliculitis provide promising alternatives to traditional approaches.
- Laser-Assisted Canaliculotomy: This minimally invasive procedure employs laser energy to precisely cut the canaliculus and remove obstructions. It has shorter recovery times and a lower risk of complications than conventional surgery.
- Biofilm Disruption Techniques: Methods for disrupting biofilms within canaliculi are being investigated to improve the efficacy of antibiotic treatments. Ultrasound and enzymatic agents have demonstrated potential for breaking down biofilms.
- Gene Therapy: Gene therapy is an experimental approach that aims to improve the body’s natural immune response to chronic infections. These therapies, which target specific genetic pathways, may provide long-term solutions for resistant canaliculitis.
Supportive Measures
In addition to direct treatments, supportive measures are required to manage symptoms and prevent recurrence.
- Warm Compresses: Placing warm compresses on the affected area can help reduce swelling and promote drainage.
- Lid Hygiene: Regularly cleaning the eyelid margins can help prevent reinfection and improve overall ocular health.
By combining these treatment strategies, healthcare providers can effectively manage chronic lacrimal canaliculitis, reduce symptoms, and improve patients’ quality of life.
Trusted Resources
Books
- The Lacrimal System: Diagnosis, Management, and Surgery by Adam J. Cohen, Michael Mercandetti, and Brian G. Brazzo
- Lacrimal Gland, Tear Film, and Dry Eye Syndromes by David A. Sullivan
- Principles and Practice of Ophthalmology by Daniel M. Albert and Frederick A. Jakobiec










