What is Coloboma?
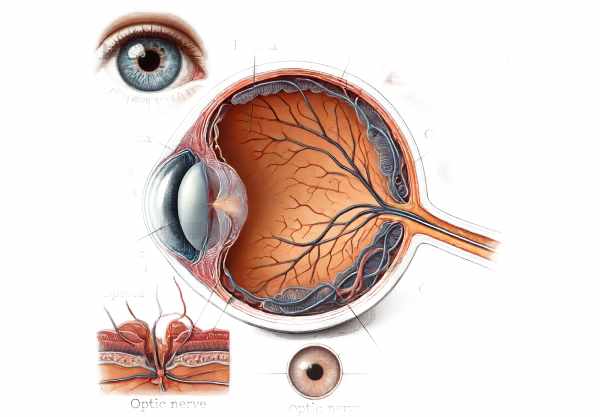
Coloboma is a congenital eye condition characterized by missing tissue from the eye’s structures. This defect occurs when the embryonic fissure fails to close completely during development, resulting in gaps or notches in various parts of the eye. These can affect the iris, retina, choroid, or optic disc, and the severity of vision loss varies with the location and size of the coloboma. Coloboma can affect one or both eyes and can be a standalone condition or part of a larger syndrome affecting other parts of the body. Understanding coloboma is critical for early detection, treatment, and prevention of complications.
Coloboma Insights
Coloboma is a group of ocular abnormalities that can impair visual function and quality of life. The term “coloboma” comes from the Greek word for “curtailed” or “defective,” which accurately describes the nature of this condition. The condition develops during early fetal development when the optic fissure fails to completely close, leaving a segmental absence of ocular tissue. This section discusses the various aspects of coloboma, such as its types, causes, clinical manifestations, and possible complications.
Types of Coloboma
Coloboma can affect multiple areas of the eye, resulting in a variety of clinical presentations. The most common types are:
- Iris Coloboma: This type appears as a keyhole or notch in the iris, usually located in the lower part of the iris. While it can cause cosmetic concerns, it has little effect on vision unless it is combined with other ocular abnormalities.
- Retinal and Choroidal Coloboma: These types have missing tissue in the retina and choroid, resulting in visual field defects and possible vision loss. The extent of visual impairment is determined by the size and location of the coloboma.
- Optic Nerve Coloboma: This form affects the optic nerve, which can result in significant vision loss and an increased risk of retinal detachment.
- Lens Coloboma: Rarely, the lens may have a notch or defect, which can cause refractive errors and impair vision.
- Eyelid Coloboma: This type has a notch or defect in the eyelid, which can cause exposure-related complications like dryness and corneal ulcers.
Causes and Risk Factors
Coloboma is primarily a congenital condition, with genetic and environmental factors influencing its development. The exact cause is frequently complex, involving interactions between genes and environmental factors.
- Genetic Factors: Coloboma can be inherited as autosomal dominant, autosomal recessive, or X-linked. Several genetic mutations have been discovered, including those that affect the PAX6, CHD7, and SOX2 genes, which are essential for eye development.
- Environmental Factors: Exposure to certain environmental factors during pregnancy, such as alcohol, drugs, or infections, can increase the risk of developing colobomas. These teratogens can disrupt the normal closure of the optic fissure.
- Syndromic Associations: Coloboma is frequently associated with multiple syndromes, including CHARGE syndrome, Cat Eye syndrome, and Treacher Collins syndrome. These syndromes affect multiple organ systems, and coloboma is one of many manifestations.
Clinical Manifestations
The clinical manifestations of coloboma differ greatly depending on the type, location, and severity of the defect. Some people may have minor symptoms, while others may have severe visual impairment.
- Visual Acuity: The impact on visual acuity is determined by the coloboma’s size and location. Retinal and choroidal colobomas can cause significant vision loss if they affect the macula or central retina. Optic nerve colobomas also carry a high risk of severe vision impairment.
- Visual Field Defects: Colobomas can cause local or widespread visual field defects. Patients may experience blind spots (scotomas) or peripheral vision loss, which impairs their ability to navigate their surroundings.
- Photophobia: Light sensitivity is common, particularly in people with large iris colobomas. The absence of a portion of the iris may allow excessive light to enter the eye, causing discomfort.
- Strabismus: Patients with coloboma may experience eye misalignment, also known as strabismus, as a result of disrupted ocular development and function. This can cause double vision (diplopia) and impaired depth perception.
- Nystagmus: Some people with coloboma may develop nystagmus, a condition marked by involuntary, rhythmic eye movements. Nystagmus can further impair visual stability and acuity.
Complications
Coloboma can cause a variety of complications, particularly if it affects the deeper structures of the eye. These complications can exacerbate visual impairment, necessitating immediate medical attention.
- Retinal Detachment: Patients with retinal and optic nerve colobomas are at a higher risk of retinal detachment, a serious condition that can result in permanent vision loss if not treated promptly. Coloboma patients are more likely to develop this complication due to their abnormal retinal structure.
- Amblyopia: Amblyopia, also known as “lazy eye,” occurs when one eye is significantly more affected than the other. The brain may prefer the better-seeing eye, resulting in impaired development of the affected eye’s visual pathway.
- Cataracts: Although less common, colobomas of the lens can increase the risk of cataract formation, resulting in further vision loss.
- Glaucoma: Colobomas may be associated with structural anomalies that increase the risk of developing glaucoma. Elevated intraocular pressure can harm the optic nerve and exacerbate visual impairment.
Effects on Quality of Life
Coloboma can have a significant impact on quality of life, particularly for those with severe visual impairment. Daily tasks such as reading, driving, and recognizing faces can be difficult. Children with coloboma may experience difficulties in school and social interactions, necessitating additional assistance and accommodations.
- Educational Challenges: Children with coloboma may require specialized educational resources and assistance to address visual impairments. Early intervention and individualized education plans (IEPs) can help to improve learning and development.
- Psychosocial Impact: The visible nature of some colobomas, particularly iris and eyelid colobomas, can result in low self-esteem and social stigma. Individuals can cope with these challenges with the help of family and friends, as well as counseling.
Prevention Tips
While coloboma cannot be completely avoided due to its congenital nature, certain precautions can help reduce the risk of complications and improve outcomes for those affected.
- Pre-natal Care:
- Ensure that the mother and developing fetus receive regular prenatal care. Early detection of potential problems can help to manage risks and improve outcomes.
- Avoiding Teratogens:
- Pregnant women should avoid known teratogens such as alcohol, tobacco, recreational drugs, and certain medications that can impair fetal growth.
- Genetic counseling:
- Families with a history of coloboma or similar genetic conditions should seek genetic counseling. This can provide information about the risks and inheritance patterns, allowing prospective parents to make informed decisions.
- A Healthy Lifestyle:
- Maintain a healthy lifestyle during pregnancy, which includes a well-balanced diet high in essential nutrients, regular exercise, and plenty of rest. Good maternal health promotes optimal fetal development.
- Folic Acid Supplements:
- Folic acid supplementation before conception and during early pregnancy can lower the risk of neural tube defects, which are linked to ocular and other developmental abnormalities.
- Early Eye Examination:
- Schedule early and regular eye exams for children, especially if there is a family history of coloboma or other ocular diseases. Early detection can help to manage complications and promote visual development.
- Protective eyewear:
- Wear protective eyewear during activities that could result in eye injuries. Preventing eye trauma is critical for coloboma patients, who are already at a higher risk of complications.
- Educational support:
- Offer educational support and resources to children with coloboma so they can succeed academically and socially. Early intervention and individualized education plans are effective ways to address visual impairments.
- Regular monitoring:
- Coloboma management requires regular visits to an ophthalmologist. Monitoring for complications such as retinal detachment, glaucoma, and amblyopia can aid in preventing further vision loss.
- Awareness & Advocacy:
- Increase awareness of coloboma and advocate for research and resources to help affected people. Increased awareness can lead to better comprehension.
Diagnostic Techniques for Coloboma
Coloboma is diagnosed using a combination of clinical examination, imaging studies, and genetic testing to determine the severity of the defect and its impact on vision.
Clinical Examination
The diagnostic process begins with an ophthalmologist performing a thorough clinical examination. The key components of the examination are:
- Visual Acuity Test: This test assesses the clarity of vision in each eye and helps determine how the coloboma affects visual function.
- Slit-Lamp Examination: A slit-lamp microscope allows the ophthalmologist to closely examine the eye’s anterior structures, such as the iris, lens, and cornea. Iris colobomas are easily identified during this examination.
- Fundoscopy: Also known as ophthalmoscopy, this technique uses an ophthalmoscope to examine the retina, choroid, and optic disc. Retinal, choroidal, and optic nerve colobomas can be visualized, allowing the doctor to determine the size and location of the defects.
Imaging Techniques
Advanced imaging techniques provide detailed views of the eye’s internal structures, which aid in the diagnosis and treatment of coloboma.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for creating high-resolution cross-sectional images of the retina. It is especially useful for evaluating retinal and choroidal colobomas, determining retinal thickness, and detecting any fluid or cysts.
- Fluorescein Angiography is an imaging technique that involves injecting a fluorescent dye into the bloodstream and photographing the retina. Fluorescein angiography can detect abnormal blood vessels, areas of leakage, and the extent of retinal involvement in coloboma.
- Ultrasound B-Scan: When the retina is difficult to see due to media opacities or significant structural abnormalities, an ultrasound B-scan can produce detailed images of the posterior segment. This technique is useful in determining the presence of retinal detachment and other associated abnormalities.
Genetic Testing
Genetic testing can reveal important information about the underlying causes of coloboma, particularly in patients with a family history or associated syndromic conditions.
- Chromosomal Microarray Analysis: This test looks for chromosomal abnormalities that could be associated with coloboma, such as deletions or duplications.
- Next-Generation Sequencing (NGS): NGS enables comprehensive analysis of multiple genes at once. It can detect mutations in genes known to be associated with coloboma, including PAX6, CHD7, and SOX2.
Differential Diagnosis
Differentiating coloboma from other ocular conditions with similar symptoms is critical for proper diagnosis and treatment.
- Retinal Detachment: In cases of retinal coloboma, distinguishing between congenital and acquired retinal detachment is critical because management strategies differ.
- Persistent Fetal Vasculature (PFV): PFV can present with similar retinal abnormalities but requires a different treatment approach.
By combining these diagnostic methods, healthcare providers can accurately diagnose coloboma, assess its impact on vision, and devise effective treatment plans to address the condition and its complications.
Effective Treatments for Coloboma
Coloboma treatment is tailored to the condition’s type and severity, as well as the symptoms and complications that may arise. The primary goals are to improve visual function, avoid complications, and promote overall eye health.
Optical Correction
- Glasses and Contact Lenses: Astigmatism, myopia, and hyperopia are all refractive errors associated with coloboma that can be corrected with glasses or contact lenses. Optical correction enhances visual acuity and reduces visual strain.
Surgical Interventions
Certain types of coloboma may require surgical treatment to address structural defects and avoid complications.
- Strabismus Surgery: When coloboma is associated with strabismus (eye misalignment), surgical correction can help to align the eyes, improve binocular vision, and reduce double vision.
- Ptosis Surgery: For patients with severe ptosis (drooping eyelids) that impairs vision, surgical correction can improve both field of vision and cosmetic appearance.
- Retinal Detachment Repair: In cases of retinal coloboma and associated retinal detachment, surgical repair, such as vitrectomy, scleral buckle, or laser photocoagulation, is required to reattach the retina and preserve vision.
Pharmacologic Treatments
Medications can be used to treat associated conditions or complications.
- Anti-Inflammatory Medications: Topical or systemic anti-inflammatory medications can help manage coloboma-related inflammation and lower the risk of secondary complications.
- Anti-VEGF Therapy: Intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) agents can be used to manage neovascularization and associated complications, such as macular edema, in coloboma patients.
Low Vision Aids and Rehabilitation
Individuals with significant visual impairment caused by coloboma can benefit greatly from low vision aids and rehabilitation services.
- Low Vision Aids: Magnifiers, telescopic lenses, and electronic visual aids can help coloboma patients make the best use of their remaining vision for daily activities.
- Vision Rehabilitation Services: Occupational therapy and vision rehabilitation services offer training and resources to help people with coloboma adjust to their visual limitations and maintain their independence.
Emerging Therapies
Research into novel and emerging therapies shows promise for improving coloboma management and its complications.
- Gene Therapy: Experimental gene therapy approaches aim to correct the genetic mutations that cause coloboma at the molecular level. This novel treatment has the potential to offer long-term solutions for managing coloboma.
- Stem Cell Therapy: Stem cell-based treatments are being researched for their ability to regenerate damaged retinal tissue and restore vision in patients with retinal coloboma.
- Advanced Imaging and Surgical Techniques: Advances in imaging technologies and minimally invasive surgical techniques are improving the diagnosis and treatment of coloboma, resulting in better patient outcomes.
Using a combination of these treatment strategies, healthcare providers can effectively manage coloboma, optimize visual function, and improve affected individuals’ quality of life.
Trusted Resources
Books
- Inherited Chorioretinal Dystrophies by Bernard Puech
- Pediatric Retina by James D. Reynolds
- Genetics for Ophthalmologists by Graeme C.M. Black
Online Resources
- American Academy of Ophthalmology
- National Eye Institute
- Genetics Home Reference
- MedlinePlus
- Orphanet