What is Congenital Glaucoma?
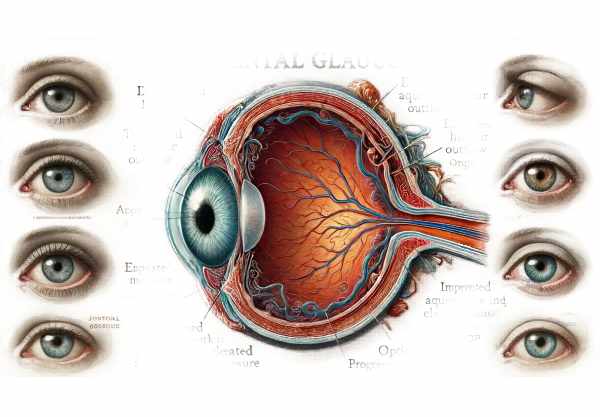
Congenital glaucoma, also known as primary congenital glaucoma (PCG), is a rare but severe eye disease that affects infants and young children. This disorder is distinguished by abnormal development of the eye’s drainage system, which results in elevated intraocular pressure (IOP), optic nerve damage, and vision loss. Congenital glaucoma can occur at birth or develop during the first few years of life. Early detection and treatment are critical for preventing irreversible visual impairment. Understanding the causes, symptoms, and implications of congenital glaucoma is critical for effective treatment and improved outcomes for affected children.
Congenital Glaucoma Insights
Congenital glaucoma is caused by a developmental anomaly in the eye’s trabecular meshwork and anterior chamber angle, both of which are necessary for aqueous humor outflow. This impaired drainage causes elevated intraocular pressure (IOP), which damages the optic nerve and leads to progressive vision loss. The condition can be inherited or develop spontaneously, and its severity varies greatly among affected individuals.
Etiology and Pathophysiology
The primary cause of congenital glaucoma is abnormal development of the eye’s drainage system. Key factors include:
- Genetic Mutations: – CYP1B1 Gene: Congenital glaucoma is primarily caused by mutations in the CYP1B1 gene. This gene encodes an enzyme that regulates the metabolism of various substances in the eye. Mutations can disrupt normal eye development, resulting in reduced aqueous outflow.
- LTBP2 Gene: Mutations in the LTBP2 gene, which regulates the structural integrity of the extracellular matrix, have been linked to congenital glaucoma.
- Developmental Anomalies: The trabecular meshwork and Schlemm’s canal, which facilitate aqueous humor drainage, can develop abnormally, resulting in decreased outflow and increased IOP. These anomalies can occur sporadically or as a result of genetic predisposition.
Clinical Presentation
The clinical presentation of congenital glaucoma can vary, but common signs and symptoms are:
- Enlarged eyes (Buphthalmos): – An abnormal enlargement of the eyes is a defining feature of congenital glaucoma. This happens when the IOP rises, causing the sclera and cornea to stretch and expand, resulting in a larger eye.
- Corneal Edema: Elevated IOP can cause corneal edema, resulting in a hazy or cloudy appearance. This may be one of the first signs detected by parents or healthcare providers.
- Photophobia: Children with congenital glaucoma may experience increased sensitivity to light (photophobia) due to corneal haze and elevated eye pressure.
- Excessive Tearing (Epiphora): – Children with congenital glaucoma often experience increased tear production and overflow, which can cause discomfort and secondary infections.
- Optic Nerve Cupping: An ophthalmoscopic examination may show increased cupping of the optic nerve head, indicating damage from high IOP.
- Visual Impairment: As the disease progresses, affected children may exhibit visual impairment, such as poor object tracking and delayed milestones.
Epidemiology
Congenital glaucoma is a rare condition that affects approximately one in every 10,000 to 20,000 live births. The condition may appear at birth or within the first few years of life. It affects both genders, with males having a slightly higher prevalence. The incidence may differ by geographic region and population, with higher rates observed in specific ethnic groups due to genetic factors.
Genetic Inheritance
Congenital glaucoma can have different inheritance patterns, including autosomal recessive and, less commonly, autosomal dominant:
- Autosomal Recessive Inheritance: – Most cases are inherited in an autosomal recessive manner. Both parents must carry one copy of the mutated gene, and if both parents are carriers, their children have a 25% chance of being affected.
- Autosomal Dominant Inheritance: – In some cases, a single mutated gene is enough to cause the disorder. Affected people have a 50% chance of passing on the condition to their children.
Complications
If left untreated, congenital glaucoma can cause a number of serious complications:
- Permanent Vision Loss: Prolonged elevated IOP can cause irreversible damage to the optic nerve, leading to blindness.
- Corneal Scarring: Persistent corneal edema and high IOP can cause scarring, impairing vision and increasing the risk of infection.
- Globe Rupture: – Severe cases with significantly elevated IOP can cause globe rupture due to excessive stretching of ocular tissues, resulting in catastrophic loss of vision and structural integrity of the eye.
Prognosis
The prognosis for children with congenital glaucoma is determined by several factors, including the severity of the condition at diagnosis, the timing and effectiveness of treatment, and ongoing management. Early detection and treatment are critical for maintaining vision and avoiding complications. Many children with congenital glaucoma can live normal, active lives with proper treatment.
Prevention Tips
Preventing congenital glaucoma entails reducing risk factors and ensuring early detection and intervention. Here are some important preventive measures and risk reduction tips:
- Genetic Counseling: Families with a history of congenital glaucoma should seek genetic counseling to assess their risks and discuss reproductive options, such as prenatal testing and preimplantation genetic diagnosis.
- Prenatal Care: – Prioritize prenatal care to prevent complications that could worsen ocular conditions. Regular prenatal check-ups can help monitor fetal development and detect anomalies early.
- Early Detection: Promptly recognizing and diagnosing symptoms can lead to timely intervention and reduce the risk of complications, including permanent vision loss.
- Regular Eye Examinations: – Children at risk should have regular eye exams to monitor their visual development and detect any abnormalities early.
- Healthy Pregnancy: – Maintaining a healthy lifestyle during pregnancy, including proper nutrition and avoiding harmful substances, promotes fetal development.
- Awareness and Education: – Educate parents and caregivers on the signs and symptoms of congenital glaucoma to promote early medical intervention.
- Avoiding Infections: Pregnant women should practice good hygiene and avoid contact with infectious individuals to prevent infections that may affect fetal development.
- Monitoring High-Risk Infants: – Infants born to parents with a history of congenital glaucoma or other risk factors should be closely monitored for early symptoms.
Congenital Glaucoma Diagnostic Techniques
Congenital glaucoma requires a multifaceted approach that includes clinical examination, imaging techniques, and, in some cases, genetic testing to confirm the diagnosis and plan appropriate treatment. Early detection is critical for preventing irreversible damage to the optic nerve and maintaining vision.
Clinical Examination
- Visual Inspection and History: – The initial evaluation includes a thorough history and visual inspection. Enlarged corneas, photophobia, excessive tearing, and corneal cloudiness may indicate congenital glaucoma.
- Tonometry: – Measuring intraocular pressure (IOP) is necessary. Goldmann applanation tonometry is the gold standard for older children, while handheld tonometers such as Perkins or Tono-Pen are used for infants and young children.
- Gonioscopy: – This technique uses a special lens to examine the anterior chamber angle of the eye, which is frequently abnormal in congenital glaucoma. It aids in determining the drainage angle for abnormalities such as angle dysgenesis.
- Slit-Lamp Examination: A slit-lamp microscope examines the anterior segment of the eye, providing detailed views of the cornea, anterior chamber, iris, and lens. Corneal diameter and clarity, as well as iris anomalies, can be measured.
- Fundus Examination: Using ophthalmoscopy to examine the optic nerve head is crucial. Glaucomatous damage is characterized by increased cupping of the optical disc.
Imaging Techniques
1) Ultrasound Biomicroscopy (UBM):
- UBM produces high-resolution images of the anterior segment structures, which aid in the assessment of the drainage angle and ciliary body abnormalities that may contribute to elevated IOP.
- Optical Coherence Tomography (OCT):
- OCT is used to obtain detailed cross-sectional images of the retina and optic nerve head, which allows for the evaluation of optic nerve damage and retinal nerve fiber layer thickness.
- Pachymetry: – Measuring corneal thickness is crucial as it impacts IOP measurements. Thicker corneas may result in falsely high IOP measurements, whereas thinner corneas may result in falsely low measurements.
Genetic Testing
- Targeted Gene Panels: – Genetic testing for known mutations associated with congenital glaucoma, such as CYP1B1 and LTBP2, can confirm diagnosis and help understand inheritance patterns and recurrence risk in families.
- Whole Exome Sequencing (WES): In cases where targeted panels are inconclusive, WES can be used to identify novel mutations or other genetic causes of congenital glaucoma.
Electrophysiological tests
- Visual Evoked Potentials (VEP): – VEP measures the electrical response of the visual cortex to visual stimuli, revealing the functional integrity of the visual pathway.
- Electroretinography (ERG): – ERG measures the electrical activity of the retina and can distinguish between retinal conditions and optic nerve abnormalities.
Congenital Glaucoma Treatment Options
Congenital glaucoma is treated with a combination of medical and surgical interventions to lower intraocular pressure (IOP) and prevent optic nerve damage. Early and aggressive treatment is critical to preserving vision.
Medical Management
- Topical Medications: – Beta-Blockers: Medications like timolol reduce aqueous humor production and lower IOP.
- Carbonic Anhydrase Inhibitors: Drugs such as dorzolamide and brinzolamide reduce the production of aqueous humor.
- Prostaglandin Analogs: Medications like latanoprost increase aqueous outflow, which lowers IOP.
- Alpha Agonists: Brimonidine reduces aqueous humor production while increasing uveoscleral outflow.
- Systemic Medications: – Oral Carbonic Anhydrase Inhibitors: Acetazolamide can quickly reduce IOP in acute situations or when topical medications are insufficient.
Surgical Interventions
- Goniotomy is a surgical procedure that involves making an incision in the trabecular meshwork to improve aqueous outflow. This is often the first-line surgical treatment for congenital glaucoma, and it is done under general anesthesia.
- Trabeculotomy: – This procedure, like goniotomy, involves opening the trabecular meshwork while also creating an external approach. It is frequently used when a goniotomy is not effective or feasible.
- Trabeculectomy: – A drainage fistula is created to bypass the trabecular meshwork and reduce IOP. This procedure is more often used in older children or when other surgeries fail.
- Glaucoma Drainage Devices: – Implants such as the Ahmed or Baerveldt valve can provide an alternative route for aqueous humor drainage. These devices are typically used for refractory cases or when other surgeries fail.
Innovative and Emerging Therapies
- Minimal Invasive Glaucoma Surgery (MIGS): These procedures, which include the iStent and Hydrus Microstent, are intended to improve aqueous outflow while minimizing trauma to ocular tissues. Their use in congenital glaucoma is still being investigated.
- Gene Therapy: – Research is underway to develop gene therapy techniques that target the genetic mutations causing congenital glaucoma. This approach shows promise for curing or significantly altering the disease course.
- Stem Cell Therapy: – Stem cell therapies aim to regenerate damaged optic nerve cells and improve trabecular meshwork function.
Post-operative Care and Rehabilitation
- Regular monitoring is crucial for monitoring disease progression and managing complications. This includes regular IOP measurements and optic nerve assessments throughout life.
- Visual Rehabilitation: Early intervention with visual aids, low vision services, and educational support can help children with congenital glaucoma maximize their visual potential and improve quality of life.
Trusted Resources
Books
- “Pediatric Ophthalmology and Strabismus” by Kenneth W. Wright and Peter H. Spiegel
- “Glaucoma: Medical Diagnosis & Therapy” by Tarek M. Shaarawy, Mark B. Sherwood, Roger A. Hitchings, Jonathan G. Crowston
- “Clinical Pediatric Ophthalmology” by Richard W. Hertle and Ellis D. Avner






