What is Corneal Ectasia?
Corneal ectasia is a progressive eye disorder characterized by thinning and bulging of the cornea, the clear, dome-shaped surface that covers the front of the eyeball. This condition causes distorted vision and can significantly reduce a person’s quality of life. Corneal ectasia can develop naturally, as in keratoconus, or as a complication of refractive surgery, such as LASIK or PRK. Understanding the underlying causes, risk factors, and progression of corneal ectasia is critical for developing effective management and treatment plans. This article delves into the complexities of corneal ectasia, examining all aspects to provide a thorough understanding of this ocular condition.
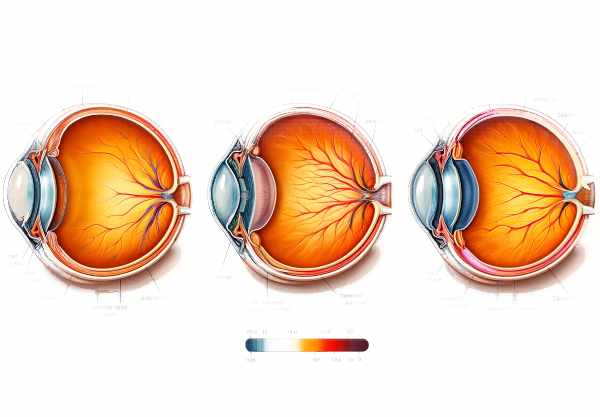
Corneal Ectasia Detailed Examination
Corneal ectasia includes keratoconus, pellucid marginal degeneration, and post-surgical ectasia. Each of these conditions has the same feature: corneal thinning and protrusion, resulting in a cone-like deformation that disrupts the cornea’s normal curvature and refractive properties.
Types of Corneal Ectasia
- Keratoconus: The most common type of corneal ectasia, keratoconus usually starts in adolescence and progresses over time. The central cornea thins gradually and forms a cone-like protrusion. The exact cause of keratoconus is unknown, but it is thought to be a combination of genetic and environmental factors. Symptoms include blurred vision, glare, and halos around lights.
- Pellucid Marginal Degeneration: This condition is similar to keratoconus, but it affects the lower periphery of the cornea, resulting in a crescent-shaped band of thinness. It usually appears later in life than keratoconus. Patients frequently experience significant astigmatism and visual distortion.
- Post-Surgical Ectasia: This type of ectasia can occur as a complication of refractive surgery, such as LASIK or PRK. The surgical alteration of the cornea’s structure can cause destabilization, resulting in progressive thinning and bulging. Pre-existing corneal abnormalities, insufficient residual stromal bed thickness, and high myopia all increase the risk of post-surgical ectasia.
Pathophysiology
The pathophysiology of corneal ectasia includes structural and biomechanical changes to the cornea. The cornea consists of five layers: the epithelium, Bowman’s layer, stroma, Descemet’s membrane, and endothelium. The stroma, which accounts for approximately 90% of corneal thickness, is critical to maintaining the cornea’s shape and strength.
- Collagen Fibril Disorganization: In corneal ectasia, the collagen fibrils in the stroma become disorganized, weakening the corneal structure. This disorganization reduces the cornea’s biomechanical stability, making it more prone to deformation under intraocular pressure (IOP).
- Enzymatic Activity: Corneal ectasia has been linked to increased enzyme activity, including matrix metalloproteinases (MMPs). These enzymes degrade extracellular matrix components, which contribute to corneal thinning and weakening.
- Genetic Factors: Genetic predisposition plays an important role in the development of keratoconus and other types of ectasia. Mutations in genes involved in collagen synthesis and extracellular matrix maintenance have been linked to these conditions. Keratoconus familial clustering suggests a hereditary component, but the precise genetic mechanisms are unknown.
Symptoms and Clinical Features
The symptoms of corneal ectasia differ according to the severity and progression of the condition. Common symptoms include:
- Blurred Vision: As the cornea thins and protrudes, its refractive properties shift, resulting in blurred and distorted vision. Patients may experience difficulty with activities that require sharp vision, such as reading or driving.
- Astigmatism: Irregular astigmatism is characteristic of corneal ectasia. The cornea’s uneven curvature causes light to focus at multiple points on the retina, resulting in distorted and blurred vision.
- Glare and Halos: Many patients report seeing glare and halos around lights, especially at night. This symptom is caused by the irregular corneal surface, which scatters light.
- Frequent Prescription Changes: As the condition progresses and the corneal shape changes, patients with corneal ectasia frequently need to have their eyeglass or contact lens prescriptions changed.
- Eye Irritation: Thinning and protrusion of the cornea can cause chronic eye irritation and discomfort. This can be exacerbated by the use of contact lenses, which may not fit properly on the irregular corneal surface.
Risk Factors
Several factors raise the risk of developing corneal ectasia.
- Genetics: Having a family history of keratoconus or other corneal ectasias significantly increases your chances of developing these conditions.
- Age: Keratoconus usually appears in adolescence or early adulthood, and progression slows or stops by middle age. Pellucid marginal degeneration usually appears late in life.
- Chronic eye rubbing has been linked to the development and progression of keratoconus. Mechanical trauma may exacerbate corneal weakness and thinning.
- Connective Tissue Disorders: Because of inherent abnormalities in collagen and extracellular matrix components, conditions like Marfan syndrome, Ehlers-Danlos syndrome, and others increase the risk of corneal ectasia.
- Refractive Surgery: Patients undergoing refractive surgery, particularly those with pre-existing corneal abnormalities or thin corneas, have a higher risk of developing post-surgical ectasia.
Progress and Impact on Vision
The progression of corneal ectasia can differ greatly between individuals. Keratoconus often progresses for 10-20 years before stabilizing. Some patients experience rapid progression, resulting in significant visual impairment within a few years.
The degree and location of corneal thinning and protrusion determine the impact on vision. Mild cases may cause minor visual disturbances that can be corrected with glasses or contact lenses, whereas severe cases may result in significant vision loss requiring surgical intervention.
Psychological and Quality of Life Impacts
The chronic and progressive nature of corneal ectasia can significantly affect a patient’s psychological well-being and quality of life. The constant need to change visual aids, frequent medical appointments, and the possibility of significant vision loss can cause anxiety, depression, and a lower overall quality of life.
Prevention Tips
- Avoid Eye Rubbing: Avoid rubbing your eyes, as this can worsen corneal thinning and contribute to the progression of conditions such as keratoconus.
- Regular Eye Exams: Schedule routine comprehensive eye exams to detect early signs of corneal ectasia and track any changes. Early detection can help to manage symptoms and slow their progression.
- Use Protective Eyewear: Wear protective eyewear when participating in activities that may result in eye injury, such as sports or working with hazardous materials.
- Manage Allergies: Allergies can cause itchy eyes, which leads to rubbing. Managing allergies with medications and avoiding allergens can help reduce the desire to rub your eyes.
- Genetic Counseling: If you have a family history of corneal ectasia, seek genetic counseling to better understand your risk and take preventative measures.
- Watch for Early Signs: Keep an eye out for early symptoms like frequent prescription changes, visual distortion, and increased glare. If you notice any of these symptoms, contact your doctor right away.
- Avoid Overuse of Contact Lenses: Maintain proper contact lens hygiene and avoid overuse to reduce stress on the cornea. Ensure that your lenses fit properly and have been prescribed by an eye care professional.
- Stay Hydrated: Adequate hydration promotes overall eye health and prevents dryness, which can lead to corneal issues.
- Protect Against UV Exposure: Wear sunglasses that block 100% of UV rays to shield your corneas from harmful ultraviolet radiation, which can hasten the progression of certain corneal conditions.
- Follow Post-Surgical Care: If you have had refractive surgery, make sure to follow all of your surgeon’s post-operative care instructions to lower your risk of developing post-surgical ectasia.
Methods to Diagnose Corneal Ectasia
Diagnosing corneal ectasia requires a comprehensive approach that includes both standard and innovative techniques for assessing the corneal structure and detecting abnormalities. Here are the main diagnostic methods:
- Slit Lamp Examination: The first step in diagnosing corneal ectasia is to conduct a thorough slit lamp examination. This allows the ophthalmologist to examine the cornea with high magnification and light, detecting thinning, irregularities, and scarring. This examination aids in the initial assessment and determines the need for additional tests.
- Corneal Topography is a non-invasive imaging technique for mapping the curvature of the cornea. It is especially useful for diagnosing and monitoring keratoconus and post-surgical ectasia. The topography generates a detailed, color-coded map of the corneal surface’s shape and irregularities, which aids in the detection of early signs of ectasia and determining the severity of the condition.
- Pachymetry: This diagnostic test measures the thickness of the cornea, which is critical for detecting thinning areas associated with corneal ectasia. Pachymetry can be done with ultrasonic or optical devices, which provide precise thickness measurements that are critical for monitoring disease progression and planning treatment strategies.
- Ocular Coherence Tomography (OCT) is an advanced imaging technique that produces high-resolution cross-sectional images of the cornea. It enables detailed visualization of the corneal layers, including thinning, scarring, and other structural changes. OCT is especially useful in diagnosing and monitoring the progression of ectasia and other corneal disorders.
- Scheimpflug Imaging: This technology produces detailed 3D images of the anterior segment of the eye, including the cornea. Scheimpflug imaging is useful for assessing corneal shape and thickness, detecting irregularities, and determining the cornea’s biomechanical properties. It is frequently used in conjunction with corneal topography to provide a thorough evaluation.
- Biomechanical Assessment: Tools like the Ocular Response Analyzer (ORA) and Corvis ST assess the cornea’s biomechanical properties. These tests aid in detecting changes in corneal stiffness and elasticity, which are early signs of ectasia. These devices provide valuable information about the cornea’s structural integrity by measuring its response to pressure.
- Genetic Testing: For hereditary forms of ectasia, such as keratoconus, genetic testing can reveal specific mutations linked to the condition. Genetic testing helps to confirm the diagnosis and provides insights into the risk factors. It also helps with genetic counseling for patients and families.
Using these diagnostic methods, eye care professionals can accurately diagnose corneal ectasia, determine its severity, and develop an appropriate treatment plan.
Corneal Ectasia: Treatment Methods
The goal of corneal ectasia treatment is to stabilize the cornea, improve vision, and prevent the condition from progressing. Here are the standard and innovative therapies:
Standard Treatments
- Glasses and Contact Lenses: In the early stages of corneal ectasia, glasses can help correct minor refractive errors. As the disease progresses, specially designed contact lenses, such as rigid gas permeable (RGP) lenses, scleral lenses, or hybrid lenses, improve vision correction by masking the irregular corneal surface.
- Corneal Cross-Linking (CXL) is a minimally invasive procedure that strengthens the cornea by increasing the number of cross-links between collagen fibers. This is accomplished by first applying riboflavin (vitamin B2) eye drops, followed by exposure to ultraviolet (UV) light. CXL slows the progression of keratoconus and other types of ectasia, saving vision and delaying the need for more invasive procedures.
- Intacs: Intacs are small, crescent-shaped plastic inserts that flatten the cornea and improve vision. This procedure is typically recommended for keratoconus patients who are unable to achieve adequate vision correction through contact lenses. Intacs can also help to stabilize the cornea and reduce astigmatism.
Innovative and Emerging Therapies
- Topography-Guided Photorefractive Keratectomy (PRK): This advanced laser treatment reshapes the cornea’s surface using precise topographic maps. When combined with CXL, it can improve vision by smoothing the corneal surface and ensuring long-term stability. Topography-guided PRK is especially beneficial for patients who have irregular astigmatism due to ectasia.
- Customized Contact Lenses: Advancements in contact lens technology have enabled the creation of highly customized lenses that are tailored to each patient’s unique corneal shape. These lenses provide superior comfort and vision correction, thereby improving the quality of life for patients with corneal ectasia.
- Intrastromal Corneal Ring Segments (ICRS): These are inserted into the cornea to change its curvature and provide structural support. This minimally invasive procedure can reduce the need for corneal transplantation while improving visual acuity in patients with moderate to severe ectasia.
- Artificial Corneas (Keratoprostheses): For patients with advanced corneal ectasia who are not eligible for traditional corneal transplants, artificial corneas offer an alternative. These synthetic implants can restore vision and are especially beneficial for people who have had multiple failed transplants.
- Gene Therapy: Researchers are working on gene therapy for corneal ectasia, which has the potential to correct underlying genetic defects and halt disease progression. While still experimental, gene therapy offers the prospect of a more targeted and long-term treatment approach.
- Stem Cell Therapy: Recent research is looking into the use of stem cells to regenerate damaged corneal tissue. Stem cell therapy shows promise in treating severe ectasia and restoring normal corneal structure and function.
By combining traditional and novel treatments, eye care professionals can effectively manage corneal ectasia, improve visual outcomes, and improve patients’ quality of life.
Trusted Resources
Books
- “Corneal Ectasia: Diagnosis and Treatment” by Ashok Garg
- “Keratoconus and Keratoectasia: Prevention, Diagnosis, and Treatment” by Ming Wang






