Introduction to Corneal Foreign Bodies
A corneal foreign body is any object or material that becomes lodged in the cornea, the clear front part of the eye. This condition is common, particularly in environments with a high concentration of airborne particles or small debris, such as construction sites, woodworking shops, or even outdoor settings with strong winds. Corneal foreign bodies can cause severe discomfort, pain, and vision problems. If not treated promptly and properly, they can lead to serious complications such as infections and permanent vision loss. Understanding the nature, causes, and risks associated with corneal foreign bodies is critical for successful prevention and management.
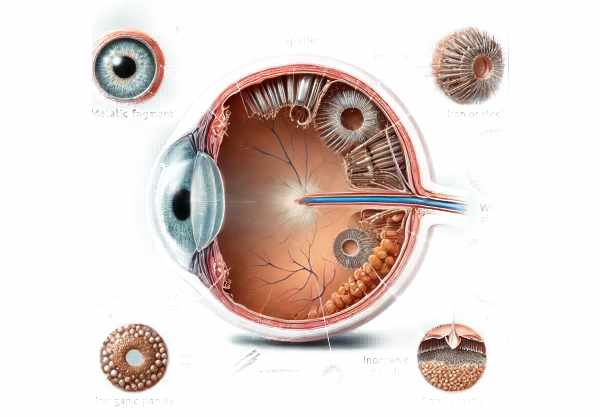
Corneal Foreign Body Detailed Examination
Corneal foreign bodies are a common cause of eye injuries and can come from a variety of sources. They are typically classified by their nature and origin, such as metallic (iron, steel), organic (wood, plant material), or inorganic (sand, plastic). The impact of a foreign body on the cornea is determined by a number of factors, including the material’s composition, the speed and force of the impact, and the amount of time it remains embedded.
Causes and Sources
- Occupational Hazards: Workers in industries such as construction, metalworking, and manufacturing are particularly vulnerable to corneal foreign bodies due to the nature of their work environments. Grinding, drilling, and welding can all generate high-velocity particles that can become embedded in the eye.
- Environmental Exposure: Outdoor activities, especially those in windy or dusty conditions, can result in foreign bodies such as sand, dust, or plant material entering the eye. Activities such as gardening, hiking, and cycling can raise this risk.
- Domestic Incidents: Everyday activities at home, such as cooking (particularly with splattering oil), cleaning, or using household tools, can all result in foreign bodies entering the eye.
- Sports and Recreation: High-speed sports, such as tennis, racquetball, and woodworking as a hobby, can increase the risk of corneal foreign bodies. Protective eyewear is frequently overlooked in these settings, increasing the risk of injury.
Symptoms and Clinical Presentation
The presence of a foreign body in the cornea usually produces immediate and noticeable symptoms, which can include:
- Pain and Discomfort: One of the most noticeable symptoms is a sharp, persistent pain in the eye, which is commonly described as feeling like something is stuck in the eye.
- Tearing: Reflex tearing is a common reaction as the eye attempts to flush out the foreign material. This can cause excessive watering of the eyes.
- Redness: The foreign body causes irritation and inflammation in the affected eye, causing it to turn red.
- Photophobia: Another common symptom is sensitivity to light (photophobia), which makes the patient uncomfortable in bright environments.
- Blurred Vision: Depending on the size and location of the foreign body, your vision may become temporarily blurred or impaired.
- Foreign Body Sensation: Patients frequently describe a persistent sensation that something is in their eye, even if the foreign body is not visible.
Complications
If a corneal foreign body is not treated promptly and appropriately, several complications may occur:
- Infection: Because the cornea is a highly sensitive and vascularized tissue, infections can occur if a foreign body remains lodged. Bacterial, fungal, or even amoebic infections can occur, resulting in severe ocular complications.
- Corneal Ulcer: Persistent irritation and the presence of a foreign body can cause a corneal ulcer, which is a painful open sore on the cornea that can impair vision.
- Scarring: Removing a foreign body can occasionally cause corneal scarring, which can impair vision, particularly if the scar is in the central visual axis.
- Perforation: In severe cases, especially with high-velocity impacts, a foreign body can perforate the cornea, causing more extensive damage to the eye and possibly vision loss.
Healing and Recovery
The cornea has an extraordinary capacity for healing, but the recovery process can vary depending on the nature and extent of the injury.
- Minor Injuries: Small, superficial foreign bodies that are removed quickly typically heal within a few days. Lubricating eye drops and antibiotic ointments may be recommended to promote healing and prevent infection.
- Moderate Injuries: Severe or extensive injuries may take longer to heal. Patients may require follow-up visits to monitor healing and rule out complications like infections or ulcers.
- Severe Injuries: When significant damage has occurred, such as perforation or deep corneal ulcers, more intensive treatment and longer recovery times are required. A surgical procedure may be required to repair the cornea and restore vision.
Risk Factors
Several factors can raise the risk of developing a corneal foreign body injury:
- Lack of Protective Eyewear: Not wearing protective eyewear while engaging in high-risk activities significantly increases the likelihood of foreign bodies entering the eye.
- High-Risk Occupations: Jobs that require exposure to flying debris, dust, or high-velocity particles have a higher risk of ocular injury.
- Outdoor Activities: Participating in activities in windy, dusty, or sandy environments without eye protection increases the risk of foreign bodies.
- Pre-existing Eye Conditions: People who have certain eye conditions, such as dry eyes or prior corneal injuries, may be more vulnerable to foreign bodies.
- Contact Lens Use: Wearing contact lenses can occasionally trap foreign objects against the cornea, increasing the risk of injury and infection.
Prevention Tips
- Wear Protective Eyewear: Always wear safety goggles or protective eyewear when participating in activities that could cause eye injury, such as construction work, metalworking, or sports involving high-speed objects.
- Use Eye Protection in Dusty Environments: When working or spending time in dusty, sandy, or windy conditions, wear protective glasses to keep foreign particles from entering your eyes.
- Follow Safety Protocols at Work: To reduce the risk of ocular injuries, follow workplace safety guidelines, which include the use of protective equipment.
- Handle Household Tools Safely: To avoid accidental eye injuries, wear protective eyewear when using household tools like hammers, drills, or saws.
- Be Careful When Engaging in Outdoor Activities: Activities such as gardening, cycling, or hiking can expose your eyes to debris. Wearing wraparound sunglasses can provide additional protection.
- Avoid Rubbing Your Eyes: If you feel something in your eye, don’t rub it because it could cause more damage. Instead, rinse your eyes with clean water or a saline solution.
- Use Caution with Contact Lenses: Make sure to keep contact lenses clean and handle them properly. Avoid wearing them in environments where foreign bodies are likely to be present, and never sleep with contact lenses unless prescribed.
- Educate Children: Emphasize the importance of eye safety and the use of protective eyewear during play or sports.
- Regular Eye Exams: Routine comprehensive eye exams can help detect and treat any underlying conditions that may increase the risk of corneal injury.
- Have First Aid Supplies on Hand: Keep a first aid kit with saline solution and an eye cup at home and at work to provide immediate assistance if a foreign object enters the eye.
Diagnostic methods
A corneal foreign body is diagnosed using a combination of patient history, clinical examination, and advanced diagnostic techniques to accurately locate and assess the object. Here are the main diagnostic methods used:
- Patient History and Symptom Evaluation: The first step is to obtain a detailed patient history in order to understand the circumstances surrounding the injury. This includes questions about the patient’s activity, the onset and nature of symptoms, and any immediate actions taken following the injury.
- Slit Lamp Examination: A slit lamp examination is an important tool for detecting corneal foreign bodies. This specialized microscope enables the ophthalmologist to examine the eye at high magnification and in bright light. By adjusting the angle and width of the light beam, the examiner can get a clear picture of the corneal surface and determine the location, size, and depth of the foreign body.
- Fluorescein Staining: A fluorescent dye is applied to the eye’s surface, highlighting corneal abrasions and foreign bodies. Under cobalt blue light, areas where the corneal epithelium has been disrupted will fluoresce brightly, making it easier to detect even small or embedded foreign objects.
- Eversion of the Upper Eyelid: To ensure that no foreign object is trapped beneath the upper eyelid, the clinician may gently evert (flip) the eyelid. This is important because foreign bodies can sometimes remain hidden and cause irritation if not identified and removed.
- Direct Visualization: For visible foreign bodies, direct visualization with the naked eye or magnifying tools may be sufficient. This method is especially effective for larger or superficially lodged foreign bodies.
- Anterior Segment Optical Coherence Tomography(AS-OCT): AS-OCT is an advanced imaging technique that generates high-resolution cross-sectional images of the cornea. This technology can help locate and assess the depth of embedded foreign bodies, especially when they are difficult to see with traditional methods.
- X-rays or CT Scans: If the foreign body appears to be metallic or has penetrated deeper into the eye, imaging techniques such as X-rays or CT scans can be used. These methods assist in determining the precise location and nature of the foreign body, thereby guiding the treatment plan.
- Ultrasound Biomicroscopy: This technique employs high-frequency ultrasound waves to produce detailed images of the eye’s anterior segment. It is especially useful for detecting foreign bodies that are invisible to other imaging techniques, providing important information about their size and location.
These diagnostic methods allow healthcare providers to accurately identify and assess corneal foreign bodies, ensuring appropriate and timely treatment to avoid complications.
Effective Treatments for Corneal Foreign Body
The treatment of corneal foreign bodies focuses on safely removing the object, relieving symptoms, and avoiding complications like infection or scarring. Here are the conventional treatment options and emerging therapies:
Standard Treatments
- Irrigation: For superficial foreign bodies, particularly those made of dust or sand, irrigation with sterile saline or eyewash solutions can aid in flushing the object. This method is frequently the first step in managing corneal foreign bodies and can be done at home or in a clinic.
- Topical Anesthetics: To make the removal process easier and reduce patient discomfort, topical anesthetic drops are used to numb the eyes. This enables a more thorough examination and easier removal of the foreign body.
- Cotton Swab or Spud: To gently lift and remove foreign bodies from the cornea, use a sterile cotton swab or a spud (a small, blunt instrument). This procedure should only be performed by a trained healthcare professional to avoid further injury.
- Needle Extraction: If the foreign body is embedded in the cornea, a sterile needle can be used to gently lift and extract the object. This procedure necessitates precision and expertise, and is usually carried out under slit lamp guidance to ensure accuracy.
- Antibiotic Eye Drops or Ointments: Following removal, antibiotic eye drops or ointments are prescribed to prevent infection. These medications assist the cornea in healing from the injury caused by the foreign body.
- Patching: For larger or more traumatic injuries, the eye may need to be patched to keep it closed and heal. However, this practice is less common nowadays because it can sometimes slow the healing process and increase the risk of infection.
Innovative and Emerging Therapies
- Laser-Assisted Removal: In certain circumstances, laser technology can be used to precisely target and remove corneal foreign bodies. This method provides high accuracy while minimizing trauma to the surrounding corneal tissue.
- Amniotic Membrane Transplantation: For severe corneal injuries caused by foreign bodies, amniotic membrane transplantation can promote healing and reduce inflammation. The amniotic membrane stimulates epithelial regeneration and has anti-inflammatory and scarring properties.
- Stem Cell Therapy: New research on stem cell therapy suggests that it has the potential to repair corneal damage caused by foreign bodies. Stem cell therapy is intended to regenerate damaged corneal tissue and restore normal function.
- Nanotechnology-Based Drug Delivery: Advances in nanotechnology are enabling the creation of targeted drug delivery systems for the eye. These systems can deliver antibiotics or anti-inflammatory medications directly to the site of injury, improving treatment efficacy and minimizing side effects.
- Biodegradable Implants: Biodegradable implants, which gradually release medication over time, are being investigated as a treatment option for preventing infections and promoting healing after foreign body removal.
By combining traditional and innovative treatment approaches, healthcare providers can effectively manage corneal foreign bodies, reduce complications, and improve patient outcomes.
Trusted Resources
Books
- “Clinical Procedures in Primary Eye Care” by David B. Elliott
- “Corneal Disorders: Clinical Diagnosis and Management” by Howard M. Leibowitz
Online Resources
- American Academy of Ophthalmology
- National Eye Institute
- MedlinePlus: Corneal Foreign Body
- Mayo Clinic: Corneal Foreign Body
- EyeWiki: Corneal Foreign Body